Clinic Flow
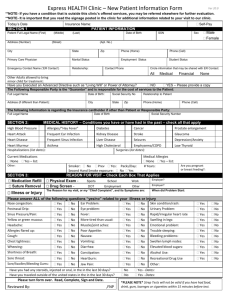
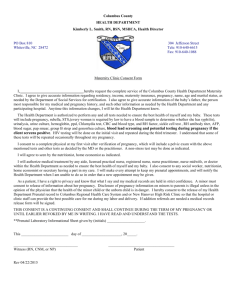
advertisement
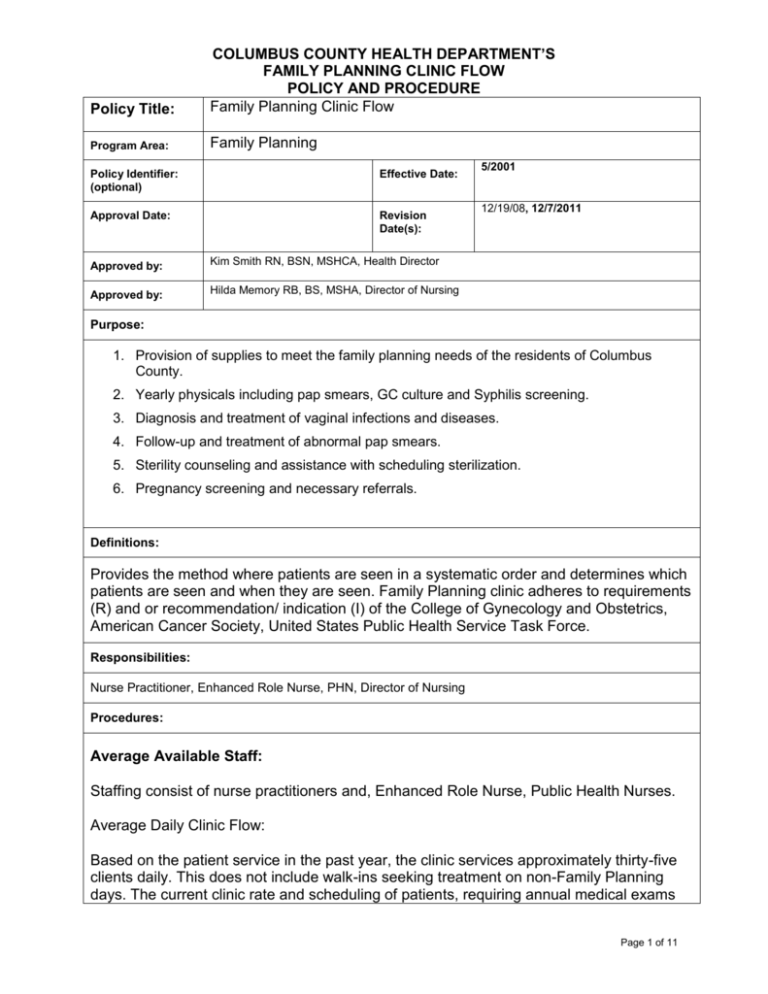
Policy Title: COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE Family Planning Clinic Flow Program Area: Family Planning Policy Identifier: (optional) Effective Date: Approval Date: Revision Date(s): Approved by: Kim Smith RN, BSN, MSHCA, Health Director Approved by: Hilda Memory RB, BS, MSHA, Director of Nursing 5/2001 12/19/08, 12/7/2011 Purpose: 1. Provision of supplies to meet the family planning needs of the residents of Columbus County. 2. Yearly physicals including pap smears, GC culture and Syphilis screening. 3. Diagnosis and treatment of vaginal infections and diseases. 4. Follow-up and treatment of abnormal pap smears. 5. Sterility counseling and assistance with scheduling sterilization. 6. Pregnancy screening and necessary referrals. Definitions: Provides the method where patients are seen in a systematic order and determines which patients are seen and when they are seen. Family Planning clinic adheres to requirements (R) and or recommendation/ indication (I) of the College of Gynecology and Obstetrics, American Cancer Society, United States Public Health Service Task Force. Responsibilities: Nurse Practitioner, Enhanced Role Nurse, PHN, Director of Nursing Procedures: Average Available Staff: Staffing consist of nurse practitioners and, Enhanced Role Nurse, Public Health Nurses. Average Daily Clinic Flow: Based on the patient service in the past year, the clinic services approximately thirty-five clients daily. This does not include walk-ins seeking treatment on non-Family Planning days. The current clinic rate and scheduling of patients, requiring annual medical exams Page 1 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE and initial visit exams each clinic day in the A.M. and the P.M. is a maximum of fifteen patients, with a preference of ten. Essential Components of Initial/Annual Examination Visit Requirements: 1. Laboratory: A. The following test is performed as indicated (I) by history, physical, method, or previous lab test, and /or ACOCG/ACS/USPSTF guidelines. Anemia Assessment Gonorrhea- The Health Department must screen all females who are less than 25 years of age and those older than 25 and having symptoms, sex partner referral, high risk history, i.e. new or multiple partners, and or testing for IUD insertion, 3months post positive for CT and GC on all initial and return visits Chlamydia- The Health Department must screen all females who are less than 25 years of age and those older than 25 and having symptoms, sex partner referral, high risk history, i.e. new or multiple partners, and or testing for IUD insertion, 3months post positive for CT and GC on all initial and return visits Diabetes Testing Cholesterol and Lipids Hepatitis B Syphilis serology Rubella titer Urinalysis HIV B. Pap Smear Pap Smears will be initiated 3 year after the onset of sexual activity or at the age of 21, every 2 years from age 20-30, then age 30 years and greater every 3 years after 3 years of negative results or as indicated by history, physical, method, or previous lab test, and /or ACOCG/ACS/USPSTF guidelines. Abnormal Pap Smear follow-up should be in accordance with Pap Smear Screening: A Guide for Health Departments Page 2 of 11 II COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE Immunity Assessment for Rubella and Tetanus-Diphtheria 1. Initial Visit (or completion of the initial data base) a. Rubella assessment is met if the patient’s record contains documentation of Administration documentation to include the specific date and place, if other than the local health department. Note: Rubella vaccine was not available until June 9, 1969. Measles-Rubella combined vaccine was not available until April 22, 1971. Any history entries prior to these dates should be ignored. Rubella vaccine in the absence of pregnancy, agreement to avoid pregnancy for three months, and informed consent obtained. Laboratory test for Rubella indication no need for vaccine. Refusal of the vaccine with the provision of counseling to susceptible patient, including informed consent (advantages and disadvantages of immunity). Contraindications of vaccine (pregnancy) For question regarding varicella refer to varicella policy. (Refer to the Family Planning Service Manual for additional information) b. Assessment of Tetanus-Diphtheria is met if the record contains documentation of one of the following: Administration documentation of Tetanus within ten years. If the source of documentation is oral the source of documentation should be documented in the record. Refusal of the vaccine with the provision of counseling to susceptible patients. 2. Reassessment of immunity status at the time of complete physical or as indicated by history, physical, method, or previous lab test. III. History (refer to Form DEHNR 2814F or 4060) http://whb.ncpublichealth.com/Forms/4060F-WEB-062110.pdf http://whb.ncpublichealth.com/Forms/2814-F-061410.pdf A. General-Initial visit history requirement is satisfied if the following information is obtained and documented in the clinical record: 1. Social- Name, age, marital status, education, occupation 2. Medical- Past significant illnesses, hospitalizations, Page 3 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE of having blood transfusions or exposure to blood products, chronic or acute medical conditions, allergies 3. Surgical- Past Surgeries 4. Menstrual- Last menstrual period, age of menarche, frequency, duration, problems 5. Contraceptive- Present and past methods, problems or reason for discontinuing 6. Obstetrical- Total number of pregnancies (term, preterm, abortions, and living) Any complications of pregnancy or delivery 7. Sexual- Age at onset of sexual activity (for teenagers) 8. Immunizations- Rubella and Tetanus immunity assessment 9. Drugs/Medications- Includes prescription, non-prescription, illegal, drugs, alcohol and tobacco amount per day 10. Douching- frequency, reason 11. Family Medical Presence of significant health problems of immediate family members( i.e. Malignancies, heart disease, Diabetes, High Blood Pressure, genetic disorders, etc. B. Update of the General History requirement at the Complete Physical (12 months or 24 months) is met by the documentation of any problems or changes since the last visit. Specifically, the last menstrual period is documented and the response to the following specific questions regarding methods of contraception. 1. Combined Pills - A- Abdominal pain (severe) C- chest pain (severe, cough, shortness of breath or sharp pain on breathing in) H- headaches (severe) dizziness, weakness, or numbness, especially if one-sided E- eye problems (vision loss or blurring), speech problems S- severe leg pain (calf or thigh) Page 4 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE 2. IUD P- period late (pregnancy), abnormal spotting or bleeding A- abdominal pain, pain with intercourse I- infection exposure (any STD), abnormal discharge N- not feeling well, fever, chills S- String missing, shorter or longer 3. Implanon Sever lower abdominal pain (ectopic pregnancy is rare but can occur) Heavy vaginal bleeding Arm pain Pus or bleeding at the insertion site (signs of possible infection) Expulsion of an implant Delayed menstrual periods after a long interval of regular periods Migraine headaches, repeated very painful headaches, or blurred vision Mood swings, depression 4. Depo-Provera Repeated, very painful headaches Heavy bleeding Depression Severe, lower abdominal pain (may be a sign of pregnancy) Pus, prolonged pain, or bleeding at injection site 5. Progestin-Only Pills (Minipills) Abdominal pain-may be due to an ovarian cyst or an ectopic pregnancy Delayed period after several months of regular cycles may be a sign of pregnancy Repeated very severe headaches Pill taken too late-even if only 3 hours late use a back-up contraceptive for the next 2 days. Be careful to use minipills on time 6. Vaginal Barriers Sudden high fever Page 5 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE Vomiting, diarrhea Dizziness, faintness, weakness Sore throat, aching muscles and joints Rash (like a sunburn) C. “Method Specific” history requirements for revisits are met by documentation of any problems or changes since the last visit. Specifically, the last menstrual period is documented and the responses to the following specific questions regarding contraceptive methods. 1. Combined Pills- A- abdominal pain (severe) C- chest pain (severe, cough, shortness of breath or sharp pain on breathing in) H- headaches (severe), dizziness, weakness, or numbness, E- eye problems (vision loss or blurring), speech problems S- severe leg pain 2. IUD- P- period late (pregnancy), abnormal spotting or bleeding A- abdominal pain, pain with intercourse I- infection exposure (any STD), abnormal discharge N- not feeling well, fever, chills S- string missing, shorter or longer 3. Implanon Sharp chest pain, coughing blood, or sudden shortness of breath (possible clot in the lung) Persistent pain in the calf (back of lower leg) (possible clot in the leg) Crushing chest pain or heaviness in the chest ( possible heart attack) Sudden severe headache or vomiting, dizziness of fainting, problems with vision or speech, weakness, or numbness in an arm or leg (possible stroke) Sudden partial or complete blindness ( possible clot in the eye) Yellowing of the skin or whites of the eyes (jaundice), especially with fever, tiredness, loss of appetite, dark colored urine, or light colored bowel movements (possible liver problems) Page 6 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE Severe pain, swelling, or tenderness in the abdomen ( possibly indicating an ectopic pregnancy, a ruptured or twisted ovarian follicle, or gall bladder or liver problems) Breast lumps Difficulty in sleeping, weakness, lack of energy, tiredness, or sadness (possible severe depression0 Heavy vaginal bleeding Depo-Provera Repeated, very painful headaches Heavy bleeding Depression Severe, lower abdominal pain (may be a sign of pregnancy) Pus, prolonged pain, or bleeding at injection site Progestin-Only Pills (Minipills) Abdominal pain-may be due to an ovarian cyst or an ectopic pregnancy Delayed period after several months of regular cycles may be a sign of pregnancy. Repeated, very severe headaches Pill taken too late- even if only 3 hours late use a back up contraceptive for the next 2 days Vaginal Barriers Sudden high fevers Vomiting, diarrhea Dizziness, faintness, weakness Sore throat, aching muscles and joints Rash (like a sunburn) Page 7 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE IV. Physical Examination A. General physical examination is met if the following components are completed at the Initial Visit and annually.* Note: Requirements for the Initial Visit may also be met if the physical exam components are provided at the time of, or prior to, the completion of the initial data base (patient and family history). Even though the initial data base is often completed at the time of the Initial Visit, it may be gathered over two closely spaced visits. The components are completed when a code or description of findings is entered for all items regardless of method. 1. Height, weight and blood pressure (height not indicated on subsequent exams if growth is compete). 2. Thyroid 3. Heart 4. Lungs 5. Breast ( SBE instructed or reviewed at Initial Visit and reviewed and annually) Inspection and palpation of breast for masses or lumps, tenderness, symmetry, or nipple discharge. 6. Lungs 7. Heart 8. Abdomen 9. Neurological 10. Musculoskeletal 11. Extremities 12. Pelvic Examinations External genitalia ( e.g. general appearance, hair distribution, or lesions) Urethra meatus ( e.g., size, location, lesions, or prolapse) Urethra (e.g., masses, tenderness, or scarring) Page 8 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE Bladder ( e.g., fullness, masses, or tenderness) Vagina ( e.g., general appearance, estrogen effect, discharge, lesions, pelvic support, cystocele, or rectocele) Cervix (e.g., general appearance, lesions or discharge) Uterus (e.g., size, contour, position, mobility, tenderness, consistency, descent, or support) Adnexa (ovaries and oviducts) and parametria (soft tissure about the uterus). (e.g., masses, tenderness, organomegaly, or nodularity Anus and perineum Digital rectal examination including sphincter tone, presence of hemorrhoids, and rectal masses. *Repeating the physical is not necessary when the last physical was performed within six months, documented in the clinical record, and was within normal limits as judged by the family planning clinician. *Rectal examinations is indicated in the presence of the following. 1. Rectal pain 2. Itching 3. Bleeding 4. Significant change in bowel habits 5. Evidence of cystocele or rectocele 6. Inability to palpate uterus on vaginal examination B. Method Specific Physical Exam requirements for Revisits and Complete Physical are as follows 1. Hormone contraception Depo-Provera, Implanon a. Weight e. Abdominal palpation b. Blood pressure f. Pelvic exam* c. Extremities g. Heart and lungs d. Breast (SBE reviewed) h. Thyroid 2. IUD a. Revisit within three months of insertion-IUD check b. Revisit every twelve months- BP, Pelvic exam* Page 9 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE c. Complete physical annually 3. Diaphragm a. Revisit is required for fitting exam within one month of fitting for the non-experienced user. b. Revisit at twelve months-pelvic exam* c. Complete physical annually * Includes examination of cervix, uterus, and adnexa. Rectal examination is indicated in the presence of the following: 1. Rectal Pain 2. Itching 3. Bleeding 4. Significant change in bowel habits 5. Evidence of cystocele or rectocele 6. Inability to Palpate the uterus on vaginal exam V. Education and counseling A. These activities must be completed prior to or at the same time of the receipt of contraceptive methods: 1. Information on the various contraceptive methods and their risks and benefits 2. Method specific informed consent process documenting the patient’s Voluntary consent to receive treatment and services 3. Counsel post partum clients to delay pregnancy for at least 18 months after delivery. C. Method of specific informed consent process must be renewed and updated When there is any change in the method of contraception. Page 10 of 11 COLUMBUS COUNTY HEALTH DEPARTMENT’S FAMILY PLANNING CLINIC FLOW POLICY AND PROCEDURE VI. Plan/Method/Recommendation A. Assess all findings B. Consider client desire C. Review of medical contraindications D. Application of method physiology to client and client’s needs E. Consideration of application of desired method to client F. Assist in choosing most appropriate method G. Explain method H. Plan evaluation of method I. Assist with appointment scheduling for abnormal findings Laws and Rules: Title X Guidelines Reference(s): Page 11 of 11