Faculty of Liaison Psychiatry – Royal College of Psychiatrists
advertisement

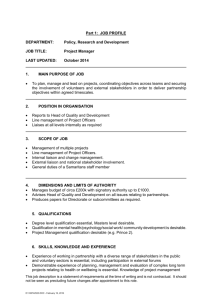
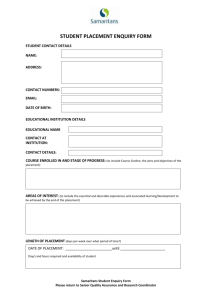
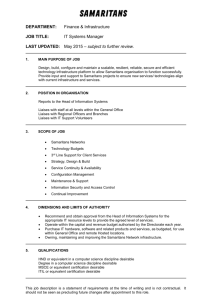
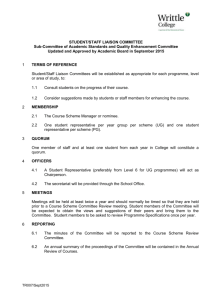
Faculty of Liaison Psychiatry – Royal College of Psychiatrists JISC UPDATE May 2013 A lot of useful content this month – much to think about…. Child and Adolescent Mental Health Liaison services A question was raised about hospitals’ experiences of paediatric liaison input to the general hospital – as this seems to vary so widely. Lucy Palmer from the Royal College told us that there had been a special interest group for paediatric liaison and they developed some (draft) standards - see below. 1) The majority of liaison professionals are satisfied with the length of time they are able to spend on each assessment (including face to face time, reading notes and writing up notes) 2) The majority of young people (or carer, if present) is satisfied with the length of time spent on the mental health assessment 3) The peer review team (or Accreditation Committee) agrees that the majority of care plans are well constructed Note: Care plans should: * Consider young person's level of functioning and communication needs; * Consider the young person's family and community needs and context; * Demonstrate that the assessor has made efforts to access past notes; * Include a clear formulation of diagnosis; * Indicate a care/discharge plan which aims to address problems and build on the service user's (and carer's) strengths and needs 4) If the young person presents with a companion, the assessor offers them the choice of having the companion present during the assessment . Note: this should only happen after the assessor has spent some time alone with the patient, to ensure that the patient can speak privately at first (if applicable). In other cases, where the companion wishes to speak to the assessor in private, this should also be facilitated (with the patient's permission). Young people's and/or their parents/carers involvement with other agencies are clearly identified during assessment 5) Assessments of individuals' ability to consent are made in accordance with the relevant legal principles: * Under 16s are presumed not to be competent to make decisions about their treatment unless they are assessed to be Gillick/Fraser competent * People aged 16 and over are presumed to have capacity to make decisions about their treatment unless it is established that they lack capacity (section 1 MCA 2005) 6) All assessments relating to the young person's ability to consent are recorded in their notes 7) Where young people are not able to give consent, their views are ascertained as far as possible and taken into account Note: consent from someone with parental responsibility is obtained or recorded in accordance with the MCA 2005. 8) Staff must be clear on who holds parental responsibility (if applicable) and this should be recorded in the case notes We were told that Anthony Crabb has taken over as chair of the Paediatric Liaison Network (now officially an RCPsych network) and that there is a survey on national service provision pending. Samaritans A Liaison Team has just developed a Samaritans link with A+E at Frimley Park Hospital. As this is a new service, they have gone through rigorous preparation; induction of volunteers and A+E staff, in-house public relations, document and policy development, scrutiny by the acute hospital clinical governance committee etc and they are more than happy to share the experience and documentation with other departments that may be interested in similar work with the third sector. The links with the psychiatric teams need developing as this is primarily an acute hospital initiative driven by a superb Head of Corporate Affairs and fully supported by the A+E manager. In addition to the presence of two Samaritans in A+E (very limited time slot at present) there is the facility for referral at any time during the week of individuals who consent and wish to have subsequent follow-up telephone support. Experience of working with the Samaritans in this area has been very good so far. Professor White is one of a number of consultants who advise and support the Samaritans; ‘I would second Malcolm’s positive approach to the involvement of the Samaritans in A & E departments. The UK Samaritans have recently been offering support to several statutory agencies, including prisons, and I am aware of very positive feedback received. I would encourage colleagues to follow Malcolm and Adrian’s examples in making links with local Samaritan branches to enhance services to patients attending A & E. They are very keen to make these links. Although volunteers, I can speak to the remarkable capabilities of the Samaritans, their professional approach to selection, training, and supervision, which I hope will reassure those of us concerned about clinical governance. The international equivalent of the Samaritans is “Befrienders Worldwide”. The Samaritans are a relatively underused resource to help our patients.’ Durham and Darlington have similarly been involved with service development for many years; Samaritans offer follow up sessions (1to1 or telephone) after self harm assessment if they refer (a simple form); something they developed as part of the RCPsych Self Harm Collaborative; also they have been active in their suicide prevention task force They ran a suicide risk management training for mental health teams and the Samaritans helped with role play; MH staff commented 'I’ve forgotten how to listen and encourage like that' (and be comfortable staying with suicide emotions). This clinician calls them 'the calm amongst the storm'. Bristol has an arrangement where they can ask their local Samaritans to offer a follow-up phone call to anyone seen once they have left the A&E dept. ‘Specialling’ A Liaison service is trying to help the general hospital address the large scale use of RMN 1-1 'specialling' for patients who need to remain in the hospital because of their physical condition; but who have behavioural disturbance. They have developed a risk assessment tool to help decide whether an RMN is warranted; and follow up patients to give advice on RMNs continued use. Are there any liaison psychiatry services that employ nurses as part of their teams to provide this? Or are there any other solutions? A respondent said that their service employs a specialist mental health nurse with a background in teaching who provides specialist assessment of those on 'specials' with development of individualised plans; and also both classroom (mainly mental health 1st aid) and 1:1 'at the time' teaching of the RGNs. It seems to work really well. The Chelsea and Westminster Hospital has a lead nurse for mental health who works with liaison – ‘he is involved with us in deciding when to special patients on the wards. The acute trust pays for this, and the lead nurse has created a bank of RMNs, to reduce expense. His name and contact: paul.morris@nhs.net An initiative being tried in North West London is to use the dementia CQUIN funds to employ a nurse specialist who will be responsible for both the CQUIN targets; and also aim to reduce 1:1 use in the elderly with delirium/dementia by providing ward nurses/HCAs with training. Psycho-oncology Does anyone have experience in setting up such a service? Their oncology service funds psychology and use their general liaison service for inpatients. However referrals are rising and are often time consuming and challenging; in addition to increased acute medicine referrals. This struggle to cover this work was echoed from Southampton. A Bristol colleague suggested contacting Dr Alex Mitchell at Leicester ; who has a brilliant business plan for Psycho-oncology. Interview rooms in the ED Below are some good examples of assessment rooms which meet PLAN standards. 1. This shows an observation window and sturdy seating. Nothing else is in the room which can potentially cause harm. 2. – Below - An example of 2 doors in an assessment room. 3. – See below - This room has a strip alarm and enough room for four people to sit comfortably. The bright sofa’s make the room more welcoming. 4. Below is an example of how lightweight canvas pictures can add warmth to an assessment room, but they need to be securely and safely attached to the wall. 5. Below - This shows a room with 2 doors which open both ways, and has an observation panel whilst also ensuring privacy. Also again, a strip alarm is clearly visible. 6. Below demonstrates a room which has frosted, toughened glass for privacy and safety, sturdy furniture and is also a good sized room. The Royal College has guidance (through PLAN) on what is an acceptable standard for our interview room. The standard set out in PLAN is ‘Can the liaison team access facilities and equipment for conducting high risk assessments’? PLAN requires the following: 1. Be located to, or within, the main Emergency Department or Acute medical Unit 2. Have a door which opens both ways and is not lockable from the inside 3. Have an observation panel or window 4. Have a panic button or alarm system (unless staff carry alarms at all times) 5. Only include furniture, fittings and equipment which are unlikely to be used to cause harm 6. Ideally, the facilities should also include two doors On further discussion with Lucy Palmer, another sensible requirement is around size of room – and a room that can accommodate 4 people seated with comfort is recommended. Jackie Gordon Worthing