Gregory`s Pediatric Anesthesia Chapter 10
advertisement
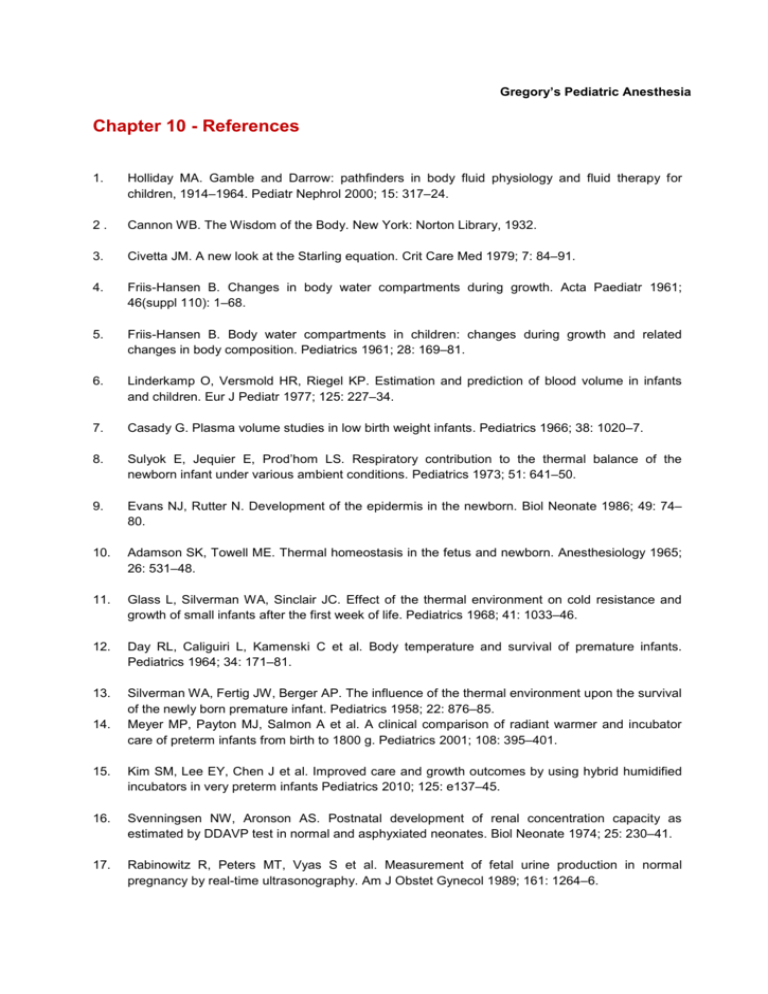
Gregory’s Pediatric Anesthesia Chapter 10 - References 1. Holliday MA. Gamble and Darrow: pathfinders in body fluid physiology and fluid therapy for children, 1914–1964. Pediatr Nephrol 2000; 15: 317–24. 2. Cannon WB. The Wisdom of the Body. New York: Norton Library, 1932. 3. Civetta JM. A new look at the Starling equation. Crit Care Med 1979; 7: 84–91. 4. Friis-Hansen B. Changes in body water compartments during growth. Acta Paediatr 1961; 46(suppl 110): 1–68. 5. Friis-Hansen B. Body water compartments in children: changes during growth and related changes in body composition. Pediatrics 1961; 28: 169–81. 6. Linderkamp O, Versmold HR, Riegel KP. Estimation and prediction of blood volume in infants and children. Eur J Pediatr 1977; 125: 227–34. 7. Casady G. Plasma volume studies in low birth weight infants. Pediatrics 1966; 38: 1020–7. 8. Sulyok E, Jequier E, Prod’hom LS. Respiratory contribution to the thermal balance of the newborn infant under various ambient conditions. Pediatrics 1973; 51: 641–50. 9. Evans NJ, Rutter N. Development of the epidermis in the newborn. Biol Neonate 1986; 49: 74– 80. 10. Adamson SK, Towell ME. Thermal homeostasis in the fetus and newborn. Anesthesiology 1965; 26: 531–48. 11. Glass L, Silverman WA, Sinclair JC. Effect of the thermal environment on cold resistance and growth of small infants after the first week of life. Pediatrics 1968; 41: 1033–46. 12. Day RL, Caliguiri L, Kamenski C et al. Body temperature and survival of premature infants. Pediatrics 1964; 34: 171–81. 13. Silverman WA, Fertig JW, Berger AP. The influence of the thermal environment upon the survival of the newly born premature infant. Pediatrics 1958; 22: 876–85. Meyer MP, Payton MJ, Salmon A et al. A clinical comparison of radiant warmer and incubator care of preterm infants from birth to 1800 g. Pediatrics 2001; 108: 395–401. 14. 15. Kim SM, Lee EY, Chen J et al. Improved care and growth outcomes by using hybrid humidified incubators in very preterm infants Pediatrics 2010; 125: e137–45. 16. Svenningsen NW, Aronson AS. Postnatal development of renal concentration capacity as estimated by DDAVP test in normal and asphyxiated neonates. Biol Neonate 1974; 25: 230–41. 17. Rabinowitz R, Peters MT, Vyas S et al. Measurement of fetal urine production in normal pregnancy by real-time ultrasonography. Am J Obstet Gynecol 1989; 161: 1264–6. 18. Vieux R, Hascoet JM, Merdariu D et al. Glomerular filtration rate reference values in very preterm infants. Pediatrics 2010; 125: e1186–92. 19. Bueva A, Guignard JP. Renal function in preterm neonates. Pediatr Res 11994; 36: 572–7. 20. Gallini F, Maggio L, Romagnoli C et al. Progression of renal function in preterm neonates with gestational age <32 weeks. Pediatr Nephrol 2000; 15: 119–24. 21. Vanpeé M, Herin P, Zetterström R et al. Postnatal development of renal function in very low birthweight infants. Acta Paediatr Scand 1988; 77: 191–7. 22. Holtbäck U, Aperia AC. Molecular determinants of sodium and water balance during early human development. Semin Neonatol 2003; 8: 291–9. 23. Rodriquez-Soriano J. New insights into the pathogenesis of renal tubular acidosis – from functional to molecular studies. Pediatr Nephrol 2000; 14: 1121–36. 24. Schwartz GJ, Haycock JB, Edelmann CM Jr et al. Late metabolic acidosis: a reassessment of the definition. J Pediatr 1979; 95: 102–7. 25. Elliot S, Goldsmith P, Knepper M et al. Urinary excretion of aquaporin-2 in humans: a potential marker of collecting duct responsiveness to vasopressin. J Am Soc Nephrol 1996; 7: 403–9. 26. Modi N. Hyponatraemia in the newborn. Arch Dis Child Fetal Neonatal Ed 1998; 78: F81–4. 27. Wiriyathian S, Rosenfeld CR, Arant BS et al. Urinary arginine vasopressin: pattern of excretion in the neonatal period. Pediatr Res 1986; 20: 103–8. 28. Gleason CA. Prostaglandins and the developing kidney. Semin Perinatol 1987; 11: 12–21. 29. Riordan JF. Angiotensin II: biosynthesis, molecular recognition, and signal transduction. Cell Mol Neurobiol 1995; 15: 637–51. 30. Godard C, Geering JM, Geering K et al. Plasma renin activity related to sodium balance, renal function and urinary vasopressin in the newborn infant. Pediatr Res 1979; 13: 742–5. 31. Sedman AB, Kershaw DB, Bunchman TE. Recognition and management of angiotensin converting enzyme inhibitor fetopathy. Pediatr Nephrol 1995; 9: 382–5. 32. Laragh JH. Atrial natriuretic hormone, the renin-aldosterone axis, and blood pressure-electrolyte homeostasis. N Engl J Med 1985; 313(21): 1330–40. 33. Bierd TM, Kattwinkel J, Chevalier RL et al. Interrelationship of atrial natriuretic peptide, atrial volume, and renal function in premature infants. J Pediatr 1990; 116: 753–9. 34. Klopfenstein HS, Rudolph AM. Postnatal changes in the circulation and responses to volume loading in sheep. Circ Res 1978; 42: 839–45. 35. Nakanishi T, Seguchi M, Takao A. Development of the myocardial contractile system. Experientia 1988; 44: 936–44. 36. Boucek RJ Jr, Shelton M, Artman M et al. Comparative effects of verapamil, nifedipine, and diltiazem on contractile function in the isolated immature and adult rabbit heart. Pediatr Res 1984; 18: 948–52. 37. Jarmakani JM, Nakanishi T, George BL et al. Effect of extracellular calcium on myocardial mechanical function in the neonatal rabbit. Dev Pharmacol Ther 1982; 5: 1–13. 38. Short BL, van Meurs K, Evans JR et al. Summary proceedings from the Cardiology Group on Cardiovascular Instability in Preterm Infants. Pediatrics 2006; 117: S34–9. 39. Evans N, Osborn D, Kluckow M. Preterm circulatory support is more complex than just blood pressure. Pediatrics 2005; 115: 1114–15. 40. Hegyi T, Anwar M, Carbone MT et al. Blood pressure ranges in premature infants: II. The first week of life. Pediatrics 1996; 97: 336–42. 41. Hegyi T, Carbone MT, Anwar M et al. Blood pressure ranges in premature infants. I. The first hours of life. J Pediatr 1994; 124: 627–33. 42. Development of audit measures and guidelines for good practice in the management of neonatal respiratory distress syndrome. Report of a Joint Working Group of the British Association of Perinatal Medicine and the Research Unit of the Royal College of Physicians. Arch Dis Child 1992; 67(10 Spec No): 1221–7. 43. Kluckow M, Evans N. Relationship between blood pressure and cardiac output in preterm infants requiring mechanical ventilation. J Pediatr 1996; 129: 506–12. 44. Groves AM, Kuschel CA, Knight DB et al. Relationship between blood pressure and blood flow in newborn preterm infants. Arch Dis Child Fetal Neonatal Ed 2008; 93: F29–F32. 45. Osborn DA, Evans N, Kluckow M. Clinical detection of low upper body blood flow in very premature infants using blood pressure, capillary refill time, and central–peripheral temperature difference. Arch Dis Child Fetal Neonatal Ed 2004; 89: F168–73. 46. Kluckow M, Evans N. Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child 2000; 82: F182–7. 47. Osborn D, Evans N, Kluckow M. Randomized trial of dobutamine versus dopamine in preterm infants with low system blood flow. J Pediatr 2002; 140: 183–91. 48. Tweed WA, Cote J, Pash M et al. Arterial oxygenation determines autoregulation of cerebral blood flow in the fetal lamb. Pediatr Res 1983; 17: 246–9. 49. Greisen G. To autoregulate or not to autoregulate – that is no longer the question. Semin Pediatr Neurol 2009; 16: 207–15. 50. Lou HC, Lassen NA, Friis-Hansen B. Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J Pediatr 1979; 94: 118–21. 51. Lou HC. Autoregulation of cerebral blood flow and brain lesions in newborn infants. Lancet 1998; 352: 1406. 52. Papile LA, Rudolph AM, Heymann MA. Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res 1985; 19: 159–61. 53. Kalhan S, Parimi P. Gluconeogenesis in the fetus and neonate. Semin Perinatol 2000; 24: 94– 106. Kalhan SC, Parimi P, van Beek R et al. Estimation of gluconeogenesis in newborn infants. Am J Physiol Endocrinol Metab 2001; 281: E991–7. 54. 55. Molina RD, Meschia G, Battaglia FC et al. Gestational maturation of placental glucose transfer capacity in sheep. Am J Physiol 1991; 261: R697–704. 56. Sunehag AL, Haymond MW, Schanler RJ et al. Gluconeogenesis in very low birth weight infants receiving total parenteral nutrition. Diabetes 1999; 48: 791–800. 57. Burns CM, Rutherford MA, Boardman JP et al. Pattern of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics 2008; 122: 65–74. 58. Windergerst KA, Buckingham B, Gandrud L et al. Association of hypoglycemia, hyperglycemia, and glucose variability with morbidity and death in the pediatric intensive care unit. Pediatrics 2006; 118: 173–9. 59. Andrew M, Paes B, Milner R et al. Development of the human coagulation system in the full-term infant. Blood 1987; 70: 165–72. 60. Andrew M, Paes B, Milner R et al. Development of the human coagulation system in the healthy premature infant. Blood 1988; 72: 1651–7. 61. Jopling J, Henry E, Wiedmeier SE et al. Reference ranges for hematocrit and blood hemoglobin concentration during the neonatal period: data from a multihospital health care system. Pediatrics 2009; 123: e333–7. 62. Snijders RJ, Abbas A, Melby O et al. Fetal plasma erythropoietin concentration in severe growth retardation. Am J Obstet Gynecol 1993; 68: 615–19. 63. Obladen M, Diepold K, Maier RF. Venous and arterial hematologic profiles of very low birth weight infants. European Multicenter rhEPO Study Group. Pediatrics 2000; 106: 707–11. 64. Herin P, Zetterström R. Sodium, potassium and chloride needs in low-birth-weight infants. Acta Paediatr 1994; 405(suppl): 43–8. 65. Hammarlund K, Sedin G, Strömberg B. Transepidermal water loss in newborn infants. VIII. Relation to gestational age and post-natal age in appropriate and small for gestational age infants. Acta Paediatr Scand 1983; 172: 721–8. 66. Gamble JL, Ross GS, Tisdall FF. The metabolism of fixed base in fasting. J Biol Chem 1923; 57: 633–95. 67. Darrow DC, Pratt EL, Flett J et al. Disturbances of water and electrolytes in infantile diarrhea. Pediatrics 1949; 1: 129–56. 68. Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics 1957; 19: 823–32. 69. Holliday MA, Freidman AL, Segar WE et al. Hospital-induced hyponatremia (reply). J Pediatr 2005; 147: 274–5. 70. Shaifee MAS, Bohn D, Horn E et al. How to select optimal maintenance intravenous fluid therapy. Q J Med 2003; 96: 601–10. 71. Moritz ML, Ayus JC. Water water everywhere: standardizing postoperative fluid therapy with 0.9% normal saline. Anesth Anal 2010; 110: 293–5. 72. Ayus JC, Achinger SG, Arieff A. Brain cell volume regulation in hyponatremia: role of sex, age, vasopressin, and hypoxia. Am J Physiol Renal Physiol 2008; 295: F619–24. 73. Sterns RH, Cappuccio JD, Silver SM et al. Neurologic sequelae after treatment of severe hyponatremia, a multicenter perspective. J Am Soc Nephrol 1994; 4: 1522–30. 74. Kozniewska E, Roberts TPL, Vexler ZS et al. Hormonal dependence of the effects of metabolic encephalopathy on cerebral perfusion and oxygen utilization in the rat. Circ Res 1995; 76: 551–8. 75. Rosenberg GA, Estrada E, Kyner WT. Vasopressin-induced brain edema is mediated by the V1 receptor. Adv Neurol 1990; 52: 149–54. 76. Arieff AI, Ayus J, Fraser C. Hyponatremia and death or permanent brain damage in healthy children. BMJ 1992; 304: 1218–22. 77. Arieff AI, Kozniewska E, Roberts T et al. Age, gender, and vasopressin affect survival and brain adaptation in rats with metabolic encephalopathy. Am J Physiol Regul Integr Comp Physiol 1995; 268: R1143–52. 78. Keating JP, Scjears GJ, Dodeg PR. Oral water intoxication in infants. An American epidemic. Am J Dis Child 1991; 145: 985–90. Bohn D. The problem of acute hyponatremia in hospitalized children: the solution is in the solution. Pediatr Crit Care Med 2008; 9: 658–9. 79. 80. Moritz ML, Ayus JC. Hospital-acquired hyponatremia – why are hyponatremic parenteral fluids still being used? Nat Clin Pract Nephrol 2007; 3: 374–82. 81. Burrows FA, Shutack JG, Crone RK. Inappropriate secretion of antidiuretic hormone in a post surgical pediatric population. Crit Care Med 1983; 11: 527–31. 82. Lieh-Lai MW, Stanitski DF, Sarnaik AP et al. Syndrome of inappropriate antidiuretic hormone secretion in children following spinal fusion. Crit Care Med 1999; 27: 622–7. 83. Arieff AI. Hyponatremia, convulsions, respiratory arrest, and permanent brain damage after elective surgery in healthy women. N Engl J Med 1986; 314: 1529–35. 84. Ayus JC, Arieff AI. Brain damage and postoperative hyponatremia: the role of gender. Neurology 1996; 46: 323–8. 85. Ayus JC, Wheeler JM, Arieff AI. Postoperative hyponatremic encephalopathy in menstruant women. Ann Intern Med 1992; 117: 891–7. 86. Arieff AI, Ayus J, Graser C. Hyponatremia and death or permanent brain damage in healthy children. BMJ 1992; 304: 1218–22. 87. Moritz ML, Ayus JC. Preventing neurological complications from dysnatremias in children. Pediatr Nephrol 2005; 20: 1687–700. 88. Kennedy PG, Mitchell DM, Hoffbrand BI. Severe hyponatraemia in hospital inpatients. BMJ 1978; 2: 1251–3. 89. Hoorn EJ, Lindemans J, Zietse R. Development of severe hyponatraemia in hospitalized patients: treatment-related risk factors and inadequate management. Nephrol Dial Transplant 2005; 21: 70–6. 90. Hoorn EJ, Zietze R Hyponatremia revisited: translating physiology to practice. Nephron Physiol 2008; 108: 46–59. 91. Hoorn EJ, van der Lubbe N, Zietse R. SIADH and hyponatraemia: why does it matter? NDT Plus 2009; 2(suppl 3): iii5–iii11. Judd BA, Haycock GB, Dalton RN et al. Antidiuretic hormone following surgery in children. Acta Paediatr Scand 1990; 79: 461–6. 92. 93. Holliday MA, Ray PE, Friedman AL. Fluid therapy for children: facts, fashions and questions. Arch Dis Child 2007; 92: 546–50. 94. Holliday MA, Friedman AL, Segar WE et al. Acute hospital-induced hyponatremia in children: a physiologic approach. J Pediatr 2004; 145: 584–7. 95. Montanana PA, Modesto I, Alapont V et al. The use of isotonic fluid as maintenance therapy prevents iatrogenic hyponatremia in pediatrics: a randomized, controlled open study. Pediatr Crit Care Med 2008; 9: 589–97. 96. Yung M, Keeley S. Randomized controlled trial of intravenous maintenance fluids. J Paediatr Child Health 2009; 45: 9–14. 97. Neville KA, Sandeman DJ, Rubinstein A et al. Prevention of hyponatremia during maintenance intravenous fluid administration: a prospective randomized study of fluid type versus fluid rate. J Pediatr 2010; 156: 313–19. 98. Hoorne EJ, Geary D, Robb M et al. Acute hyponatremia related to intravenous fluid administration in hospitalized children: an observational study. Pediatrics 2004; 113: 1279–84. 99. Bailey AG, McNaull PP, Jooste E et al. Perioperative crystalloid and colloid fluid management in children: where are we and how did we get here? Anesth Anal 2010; 110: 375–90. 100. Halberthal M, Halperin ML, Bohn D. Acute hyponatremia in children admitted to hospital: retrospective analysis of factors contributing to its development and resolution. BMJ 2001; 322: 780–2. 101. Furman E, Roman DG, Lemmer LA et al. Specific therapy in water, electrolyte and blood-volume replacement during pediatric surgery. Anesthesiology 1975; 42: 187–93. 102. ASA Task Force on Preoperative Fasting. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures. Anesthesiology 1999; 90: 896–905. 103. Kelnar CJ. Hypoglycaemia in children undergoing adenotonsillectomy. BMJ 1976; 1: 751–2. 104. Thomas DKM. Hypoglycemia in children before operation: its incidence and prevention. Br J Anaesth 1974; 46: 66–8. 105. Leelanukrom R, Cunliffe M. Intraoperative fluid and glucose management in children. Paediatr Anaesth 2000; 10: 353–9. 106. Fahy BG, Sheehy AM, Douglas B et al. Glucose control in the intensive care unit. Crit Care Med 2009; 37: 1769–76. 107. Srinivasan V, Spinella PC, Drott HR et al. Association of timing, duration, and intensity of hyperglycemia with intensive care unit mortality in critically ill children. Pediatr Crit Care Med 2004; 5: 329–36. 108. Rhodes ET, Ferrari LR, Wolfsdorf JI. Perioperative management of pediatric surgical patients with diabetes mellitus. Anesth Analg 2005; 101: 986–99. 109. Betts P, Brink S, Silink M et al. Management of children and adolescents with diabetes requiring surgery. Pediatric Diabetes 2009; 10(suppl 12): 169–74. 110. Karvonen M, Viik-Kajander M, Moltchanova E et al. Incidence of childhood type 1 diabetes worldwide: Diabetes Mondiale (DiaMond) Project Group. Diabetes Care 2000; 23: 1516–26. 111. Wild S, Roglic G, Green A et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27: 1047–53. 112. Rosenberg CS. Wound healing in the patient with diabetes mellitus. Nurs Clin North Am 1990; 25: 247–61. 113. Marhoffer W, Stein M, Maeser E et al. Impairment of polymorphonuclear leukocyte function and metabolic control of diabetes. Diabetes Care 1992; 15: 256–60. 114. Golden SH, Peart-Vigilance C, Kao WH et al. Perioperative glycemic control and the risk of infectious complications in a cohort of adults with diabetes. Diabetes Care 1999; 22: 1408–14. 115. American Diabetes Association. Type 2 diabetes in children and adolescents. Diabetes Care 2000; 23: 381–9. 116. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2004; 27: S5–10. 117. Cruse PJ, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg 1973; 107: 206–10. 118. Hjortrup A, Rasmussen BF, Kehlet H. Morbidity in diabetic and non-diabetic patients after major vascular surgery. BMJ (Clinical Res Ed) 1983; 287: 1107–8. 119. Zerr KJ, Furnary AP, Grunkemeier GL et al. Glucose control lowers the risk of wound infection in diabetics after open heart operations. Ann Thorac Surg 1997; 63: 356–61. 120. Van Den Berghe G, Wouters P, Weekwers F et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001; 345: 1359–67. 121. Misbin RI. The phantom of lactic acidosis due to metformin in patients with diabetes. Diabetes Care 2004; 27: 1791–3. 122. Mercker SK, Maier C, Neumann G et al. Lactic acidosis as a serious perioperative complication of antidiabetic biguanide medication with metformin. Anesthesiology 1997; 87: 1003–5. 123. Raucoules-Aime M, Labib Y, Levraut J et al. Use of i.v. insulin in well-controlled non-insulindependent diabetics undergoing major surgery. Br J Anaesth 1996; 76: 198–202. 124. Hemmerling TM, Schmid MC, Schmidt J et al. Comparison of a continuous glucose-insulinpotassium infusion versus intermittent bolus application of insulin on perioperative glucose control and hormone status in insulin-treated type 2 diabetics. J Clin Anesth 2001; 13: 293–300. 125. Darrow DC. Presidential address – American Pediatric Society. Am J Dis Child 1957; 94: 359– 66. 126. Engle WD. Definition of normal blood pressure range: the elusive target. In: Kleinman CS, Seri I (eds) Hemodynamics and Cardiology. Philadelphia: Saunders Elsevier Publishing, 2008, p. 48. Data from: Nuntnarumit P, Yang W, Gada-Ellzey HS. Blood pressure measurements in the newborn. Clin Perinatol 1999; 26: 981–96.