outline26447
advertisement

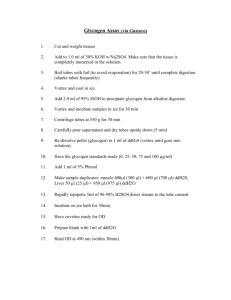
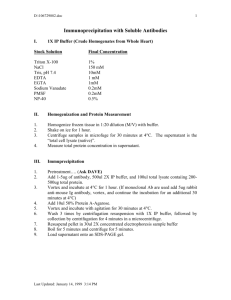
Vortex Vein Varices Case Report I. Case History a. Patient demographics: 60 year-old Caucasian male b. Chief complaint: wants new glasses c. Ocular, medical history: i. Cataract OU, no DR on previous 3 exams ii. Type 2 diabetes mellitus x 2 years, hypertension, hyperlipidemia, and obesity; stopped smoking 4 months prior d. Medications: Clotrimazole cream, Metformin, HCTZ; stopped Lisinopril and Rosuvastatin due to leg pain e. Other salient information: none II. Pertinent findings a. Clinical: i. BCVA: 20/20 OD, OS ii. Cover Test / Motilities / Confrontation fields / Pupils: normal iii. Slit Lamp Exam: non-contributory iv. IOP: 15 OD, 14 OS v. DFE: 1. Nuclear sclerotic cataract OU and Cortical cataract OS not affecting VAs 2. Lattice degeneration without holes (superior) OS 3. New (not seen on last 2 exams) 3DD dark gray domeshaped lesion superior-nasal OD without drusen or lipofuscin; 1.5DD dark gray slightly elevated round lesion superior-nasal OS without drusen or lipofuscin b. Physical: i. Vitals: BP: 144/89, Pulse: 90, Respiration: 18, Temperature 96.8° F, Pain: 0 ii. Weight: 290 lbs., Height: 70 inches iii. Normal physical exam c. Laboratory studies: i. HbA1C: 7.5 H, FBG: 155 H ii. CBC / Chem 7 / TSH / PSA / Liver panel: normal iii. Lipid panel: triglycerides 330 H, other components close to normal iv. Urinalysis: microalbumin/creatinine ratio 327.13 H, microalbumin 30.40 H, other components normal d. Radiology studies: ophthalmic ultrasound i. OD: thickness 0.87 – 1.1mm, 4 – 5mm long, higher reflectivity by Ascan, no posterior extension ii. OS: 0.67mm at thickest point, 3.5 – 4.4mm long, no posterior extension III. Differential diagnosis a. Primary/leading: Vortex vein varix i. Size: 1-3DD at base; 2DD in height Vortex Vein Varices Page 1 IV. V. ii. Color: grey-green to venous-colored iii. Location: usually nasally at equator iv. Red-free filter: black and larger v. FA: no leakage; no secondary vascular supply vi. B-scan: dynamic b. Other: Choroidal melanoma i. Size: 2-10DD ii. Color: grey-green with possibly subretinal fluid or orange pigmentation iii. Location: anywhere iv. Red-free filter: no color change v. FA: pinpoint leakage; secondary vascular supply vi. B-scan: stable; elevated Diagnosis and discussion a. Elaborate on the condition: i. First described by Rutnin in 1967 ii. First reported cases by Osher in 1981 iii. Unilateral or bilateral, either eye, single or double, equatorial location, usually nasal fundus iv. Benign, asymptomatic v. No predilection for age or gender vi. Unrelated to systemic disease vii. Rare; <1% (Osher), 0.052% (Lopez) b. Expound on the unique features: i. Color: grey-green, dark red-brown, dark red to burgundy, venouscolored ii. Shape: smooth, ,elevated, dome-shaped, round iii. Size: 1-3 DD, up to 6mm in diameter, up to 3mm thick iv. Noted on sustained gaze; may require extended duration of gaze (5 seconds) for ampulla to fill v. Lesion expands when choroidal venous pressure exceeds IOP (congestion at ampulla) 1. Extreme gaze in direction of lesion 2. Head below heart (e.g., reclined) 3. Valsalva maneuver (reclined or sitting) vi. Lesion flattens when IOP exceeds choroidal venous pressure (congestion at ampulla relieved) 1. Gaze directed elsewhere (e.g., primary gaze) 2. Head elevated 3. Digital pressure (e.g., ophthalmodynamometry, ultrasound probe, scleral depression, contact fundus lens) regardless of gaze or head position Treatment, management a. Treatment and response to treatment: no treatment necessary b. Summary of cases in the literature: i. 22 cases reported (33 lesions) Vortex Vein Varices Page 2 ii. Ages: 23-71 iii. Male: 42%, Female: 58% iv. OD: 50%, OS: 50% v. Superior nasal: 61%, Inferior nasal: 39% vi. Bilateral: 14% vii. Multiple: 27% viii. Maximum diameter: 6mm ix. Maximum height: 2DD, 2.6mm x. One report of not seeing on prior exam c. Bibliography: Buettner H. Varix of the vortex vein ampulla simulating choroidal melanoma. Am J Ophthalmol 1990; 109(5): 607-8. Da Cruz L, James B, et al. Multiple vortex vein varices masquerading as choroidal secondaries. Br J Ophthalmol 1994; 78: 800-1. Gunduz K, Shields CL, Shields JA. Varix of the vortex vein ampulla simulating choroidal melanoma – report of four cases. Retina 1998; 18(4): 343-7. Hunter JE. Vortex vein varix. Am J Optom Physiol Opt 1983; 60(12): 995-6. Kang HK, Beaumont PE, Chang AA. Indocyanine green angiographic features of varix of the vortex vein ampulla. Clin Exper Ophthalmol 2000; 28(4): 321-3. Khan J, Damato BE. Accuracy of choroidal melanoma diagnosis by general ophthalmologists: a prospective study. Eye 2007; 21: 595-7. Lopez P. Varix of the vortex vein ampulla. J Am Optom Assoc 1986; 57(2): 104-8. Levy J, Yagev R, et al. Varix of the vortex vein ampulla: a small case series. Euro J Ophthalmol 2005; 15(3): 424-7. Osher RH, Abrams GW, et al. Varix of the vortex ampulla. Am J Ophthalmol 1981; 92(6): 653-60. Potter JW, Vandervort RS, Thallemer JM. The clinical significance of the vortex veins. J Am Optom Assoc 1984; 55(11): 822-4. Rutnin U. Fundus appearance in normal eyes. Am J Ophthalmol 1967; 64(5): 821-39. Seregard S, Daunius C, et al. Two cases of primary bilateral malignant melanoma of the choroid. Br J Ophthalmol 1988; 72: 244-5. Shields CL, Shields JA, De Potter P. Patterns of Indocyanine green videoangiography of choroidal tumors. Br J Ophthalmol 1995; 79: 237-45. Singh AD, De Potter P, et al. Indocyanine green angiography and ultrasonography of a varix of vortex vein. Arch Ophthalmol 1993; 111: 1283-4. The Collaborative Ocular Melanoma Study Group. Accuracy of diagnosis of choroidal melanomas in the collaborative ocular Vortex Vein Varices Page 3 VI. melanoma study. COMS report number 1. Arch Ophthalmol 1990; 108: 1268-73. Tomasini DN. Varix of the vortex ampulla: a dynamic phenomenon. Clin Eye Vis Care 2000; 12(3-4): 151-4. Wolfensberger TJ. Varix der vortex ampulla: ungewohnliche differentialdiagnose bei aderhauttumoren (Varix of the vortex vein as a differential diagnosis in tumors of the choroid). Klin Monatsbl Augenheilkd 1997; 210(5): 334-6. Conclusion a. Clinical pearls, take away points i. Usually found on routine DFE with BIO ii. Unknown etiology; no treatment required iii. 3-mirror contact fundus lens provides quick, easy, and inexpensive method to verify disappearance (i.e., flattening) iv. Fluctuating dynamic nature is characteristic and diagnostic v. Misdiagnosis of vortex vein varix for choroidal melanoma: 0.036% (Khan), 0.020% (C Shields) vi. Misdiagnosis of retinal lesion for choroidal melanoma: 30% (Khan), 0.48% (COMS) vii. Primary bilateral choroidal melanoma: 1 case every 18 years in US viii. If in doubt, refer for ultrasound ix. If still in doubt, refer to retinal specialist Vortex Vein Varices Page 4