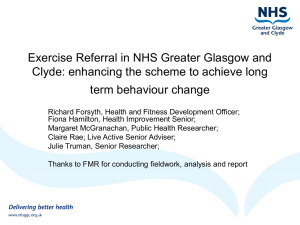
CHRONIC DISEASE IN NHS GREATER GLASGOW & CLYDE
advertisement

NHS GREATER GLASGOW &CLYDE CHRONIC DISEASE IN NHS GREATER GLASGOW & CLYDE Insights from Local Enhanced Services 2008-2009 April 2010 KEEP WELL/ENHANCED SERVICES DATA GROUP Contents Section I INTRODUCTION II POPULATION NEED III Page 3 4 2.1: Disease prevalence 2.2: Premature disease 2.3: Comorbidity 2.4: Levels of service utilisation relative to need 4 5 5 6 CLINICAL SERVICE DELIVERY & KEY OUTCOMES 8 3.1: Coronary Heart Disease 3.2: Stroke 3.3: Type 2 Diabetes 3.4: Discussion points 8 12 17 22 Foreword This paper provides some initial insights into the challenges and achievements of NHS GG&C’s care for patients with three major chronic diseases, Coronary Heart Disease (CHD), Stroke and Type 2 Diabetes through its programme of Local Enhanced Services. LES are contractual arrangements with primary care services, designed to augment the basic GMS Quality & Outcomes Framework (QOF) specification. Enhanced services for these three chronic diseases have now been established for over five years in Greater Glasgow and are being incrementally introduced into Clyde. The LES contracting process generates a rich quantity of clinical and process data, which is essential for programme delivery. However, these data are also enormously valuable in building a picture of the needs and characteristics of patients with chronic disease and in helping us to understand how our local healthcare system is responding to their needs. In this short introductory paper, we provide a brief overview of these themes, drawing on data from the LES to provide important insights into the following aspects of CHD, Stroke and Type 2 Diabetes: Estimates of population need Levels of service utilisation relative to need Variations in care processes Variations in clinical status Variations in clinical management These themes will be further developed in a series of detailed thematic reports during 2010. Anne Scoular, Keep Well/Enhanced Services Data Group Chair April 2010 2 I Introduction In common with many developed healthcare systems, NHS GG&C delivers an evidence-based programme of chronic disease management (CDM); randomised trials show that effective CDM programmes, incorporating proactive case-finding, assessment, care and ongoing monitoring of people with chronic disease, are highly cost effective. Not only do they achieve significantly reductions in hospitalisation rates and bed days, but they also improve health status, increase participation in health-promoting behaviours, improve communication with physicians and reduce fatigue, disability and the social/role limitations associated with chronic disease. Although CDM operates at a basic level through the GMS Quality & Outcomes Framework (QoF) contract across the entire GG&C area, Local Enhanced Services (LES) contracts extend the clinically based QoF into the all-important health related behaviour areas, using the practice nurse annual interview to screen for problems and support onward referral to appropriate services who can provide ongoing support for individuals. This includes compliance; up to half of all people with long term conditions do not take, or do not regularly take, their prescribed medication, with a serious impact on their quality of life, clinical outcomes and cost effectiveness. Coverage of the GG&C population is, however, not yet complete, as summarised below: Diabetes: Established across entire GG&C area CHD: Established across most of the GG&C area, except Renfrewshire. Stroke: Old Greater Glasgow area only (not operational in Clyde). The completeness of chronic disease registers allows some estimation of the prevalence of these diseases at community level in the CHCPs where the LESs are established. Caution should be used in interpreting population prevalence data in areas where there is only partial coverage by the LES. This applies in North Lanarkshire, South Lanarkshire and West Dunbartonshire. Data from North and South Lanarkshire have therefore been excluded from this paper and will be presented separately, as the NHS GG&C CDM programme only operates in a small proportion of the entire Local Authority area. Data from West Dunbartonshire are also complex to interpret, as the new CHCP incorporates some practices who were previously part of the old Argyll & Clyde Health Board area and others who were within Greater Glasgow. As the CHD and diabetes LESs are now established in West Dunbartonshire, valid prevalence estimates can be generated at CHCP level. However, the stroke LES is only operational in practices within the old ‘Greater Glasgow Health Board’ locality, thus the numbers of patients on the stroke register has not been used to estimate CHCP level stroke prevalence. The information presented in this paper largely draws on data from the 2008/09 contracting year, with appropriate comparisons with previous years when relevant. 3 II Population need 2.1 Disease prevalence Crude CHD and stroke show twofold variations in prevalence within GG&C (Figure 1), with the highest prevalence in East Glasgow and the lowest in East Renfrewshire. Crude rates of disease reflect the actual prevalence of disease. Figure 1: Crude CHD, Stroke & Type 2 Diabetes prevalence, by CHCP 70.0 Crude prevalence per 1,000 60.0 50.0 40.0 30.0 20.0 10.0 0.0 East Glasgow South East Glasgow Inverclyde West Glasgow South West Glasgow East Renfrewshire (pt) CHD 59.8 52.5 48.5 West East North Glasgow Dunbartonshire Dunbartonshire 45.6 41.9 39.6 39.4 36.8 26.0 Stroke 29.5 27.2 22.1 20.3 19.8 17.5 13.5 T2 Diabetes 44.2 44.2 37.6 37.4 36.1 34.4 34.1 30.0 29.3 19.5 CHD, stroke and, to a lesser extent, Type 2 diabetes are all commoner among older people. South Asian populations have an approximately fourfold increased risk of Type 2 Diabetes. Thus, some of this variation could simply be due to their differing population structures. However, even after standardisation for age and sex, the steep internal gradient in disease prevalence within GG&C remains (Figure 2). Figure 2: Age & sex standardised disease prevalence, by CHCP 45.0 Age & sex standardised prevalence per 1,000 40.0 35.0 30.0 25.0 20.0 15.0 10.0 5.0 0.0 East Glasgow SE Glasgow Inverclyde W Glasgow W Dun N Glasgow SW Glasgow East Dun East Ren CHD 41.9 41.4 32.5 30.4 30.0 27.1 25.2 22.9 13.6 Stroke 19.0 19.6 12.6 11.1 10.8 5.9 Diabetes 31.6 35.1 21.0 25.7 18.4 11.6 14.4 23.7 29.7 26.4 4 Renfrewshire 25.1 As there are no current reliable estimates of the ethnic composition in each CHCP, it was not possible to standardise for ethnicity. 2.2 Premature disease The GG&C population experiences more premature cardiovascular disease compared with other regions and developed nations. There are also large spatial variations in disease prevalence within GG&C, with a five-fold variation between East Renfrewshire and East Glasgow in CHD prevalence in those aged less than 65 years (Figure 3). Socioeconomic deprivation explains some of this effect, acting through a variety of different mechanisms. Figure 3: CHD, Stroke & Type 2 Diabetes prevalence (per 1,000), males <65yrs CHD 70.0 60.0 50.0 40.0 30.0 20.0 10.0 0.0 2.3 Type 2 Diabetes Stroke 50.0 45.0 40.0 35.0 30.0 25.0 20.0 15.0 10.0 5.0 0.0 35.0 30.0 25.0 20.0 15.0 10.0 5.0 0.0 Comorbidity 87,554 individual patients appeared on one or more of the three disease registers during the financial year 2008/09; 16,818 (19%) had two diagnoses and 1,193 (1%) had all three (Figure 4). Figure 4: Comorbidity Total CHD 44,654 CHD 29,746 (34%) Total Type 2 diabetes 42,152 CHD & T2 diabetes 8,235 (9%) Type 2 diabetes 29,622 (34%) All 3 1,193 (1%) Diabetes & Stroke 3,102 (4%) CHD & Stroke 5,481 (6%) Stroke 10,176 (12%) Total Stroke 19,952 In eight CHCPs, the LES programme is fully implemented across all three disease areas; in these areas, we can use the LES data to estimate the population prevalence of individuals with at least one chronic disease (ie diabetes, CHD and/or Stroke). Again, the highest prevalence (110.4 per 1,000) is observed in East Glasgow and the lowest (50.5 per 1,000) in East Renfrewshire (Figure 5,overleaf). 5 Figure 5: Crude chronic disease prevalence,* by CHCP, 2008-09 *Diagnosed with: Diabetes, CHD and/or Stroke as proportion of total CHCP population 120.0 100.0 80.0 60.0 40.0 20.0 0.0 East Glasgow South East Glasgow West Glasgow East Dunbartonshire South West Glasgow North Glasgow East Renfrewshire 110.4 104.0 80.1 78.9 74.1 73.8 50.5 Prevalence/1,000 2.4: Levels of service utilisation relative to need The total volume of individual diagnosed on the diabetes, CHD and Stroke registers in each CHCP is shown in Figure 6. This includes those who are exception coded and also does not reflect the number of individuals involved, as many have more than one disease (see previous section). Figure 6: Number of chronic disease registrations in 2008-09, by CHCP 18000 16000 14000 12000 10000 8000 6000 4000 2000 0 East South West Dunbartonshi Glasgow re North Glasgow West East Dunbartonshi Inverclyde Renfrewshire Renfrewshire re (pt) East Glasgow West Glasgow South East Glasgow Type 2 diabetes 5463 4994 4475 3979 3183 2934 3417 Stroke 3651 2806 2748 2029 2337 1977 1124 CHD 7389 5453 5315 4255 4444 3959 4165 2798 6385 1716 1184 3984 2280 Of the total cohort of patients on each disease register, the overall proportion who received disease monitoring in 2008/09 was 70.9% for stroke patients, 77.2% for CHD and 83.5% for diabetes, with significant variations between CHCPs (Table 1). 6 The between-CHCP variation was greatest for stroke (ranging from 56.9 to 75.0%) and least for diabetes (72.7 to 86.5%). As with all healthcare performance monitoring, there are many possible reasons for these variations and adjustment for age, sex, comorbidity and other determinants of casemix within each CHCP would be required before drawing any substantive conclusions. Table 1: Proportion of patients who received monitoring in 2008/09, by CHCP Proportion of patients on each disease register who received disease monitoring in 2008/09 Type 2 Diabetes CHCP % (95% ci) Inverclyde 86.5 (85.1 to 87.7) West Dun 83.0 (81.7 to 84.2) Renfrewshire 80.3 (79.3 to 81.2) SW Glasgow 78.8 (77.5 to 80.1) E Glasgow 77.8 (76.7 to 78.9) East Ren 77.6 (75.5 to79.5) W Glasgow 77.0 (75.8 to78.1) East Dun 76.8 (75.3 to 78.2) SE Glasgow 73.7 (72.4 to75.0) N Glasgow 72.7 (71.1 to 74.3) Overall 83.5 (83.2 to 83.9) CHCP West Dun Inverclyde SW Glasgow W Glasgow East Dun E Glasgow East Ren N Glasgow SE Glasgow Overall CHD % (95% ci) 80.3 (79.0 to 81.4) 77.4 (76.1 to 78.7) 75.6 (74.2 to 76.8) 73.4 (72.2 to 74.5) 72.1 (70.7 to 73.4) 71.9 (70.9 to 72.9) 66.8 (64.8 to 68.7) 65.3 (63.8 to 66.8) 62.9 (61.6 to 64.2) 77.2 (72.2 to 74.5) 7 CHCP West Dun SW Glasgow W Glasgow East Dun E Glasgow N Glasgow East Ren SE Glasgow Overall Stroke % (95% ci) 75.0 (72.4 to 77.4) 71.4 (69.4 to 73.3) 70.2 (68.5 to 71.8) 65.0 (63.1 to 66.9) 65.0 (63.5 to 66.6) 60.6 (58.5 to 62.8) 56.9 (54.1 to 59.7) 56.9 (55.0 to 58.7) 70.9 (70.2 to 71.6) III: Clinical service delivery & key outcomes 3.1: Coronary Heart Disease Of the 44,635 patients on the disease register, 7,867 (17.6%) were exception coded. Results presented from this point onwards relate to the remaining 36,768 patients. 20,839 (57%) were male and 15,929 (43%) female. Women were, on average, slightly older (mean age 73.6 years) than men (mean age 69.5 years). Ethnicity information was available in 29,822 (81%) of patients. Overall, 28,844 (96.7%) were white (Table 2) Table 2: Non-exception coded CHD patients, by ethnic subgroup Ethnic subgroup White South Asian Black Chinese Other ethnic subgroups TOTAL (known ethnicity) Number (%) 28,844 (96.7%) 746 (2.5%) 21 (0.07%) 12 (0.04%) 150 (0.5%) 29,822 (100%) There were significant variations across GG&C in the ethnic composition of the CHD register; non-white patients represented a very small minority (0.7%) of CHD patients in West Dunbartonshire, but 10.3% in SE Glasgow (Figure 7). In SE Glasgow, nonwhite subgroups were virtually all South Asian, whereas North Glasgow, Inverclyde and West Dunbartonshire were more diverse. Figure 7: Spatial variations in ethnic distribution of diagnosed CHD patients Ethnic distribution within non-white subgroup 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Other Chinese Black South Asian The patient’s postcode of residence was known in 34244 (93%), allowing estimation of small area deprivation. The vast majority of GG&C’s CHD patients live in highly deprived areas, with an inverse relationship between age and deprivation (Figure 8). Figure 8: Mean age by SIMD deprivation quintile of diagnosed CHD patients 73.0 16,000 72.0 14,000 71.0 12,000 10,000 70.0 8,000 69.0 6,000 68.0 4,000 67.0 2,000 0 Number Mean age 1 (Most deprived) 2 3 4 5 (Least deprived) 15,701 6,971 4,100 3,967 3,505 68.5 70.7 71.1 71.6 72.0 8 66.0 Mean age (years) Pts on disease register 18,000 Cholesterol monitoring: 27,766 (76%) patients had total cholesterol recorded in the past year, of whom 20,187 values were considered to be valid (2-15 mmol/l). Of these, 15,706 (78%) met the target cholesterol value (<5 mmol/l). There was considerable variation by CHCP in the proportion of patients monitored, ranging from 63% in SE Glasgow to 88% in SW Glasgow, however the proportion of patients who met the target cholesterol value was similar across the system (Figure 9). Figure 9: Cholesterol monitoring activity & outcomes in CHD patients, by CHCP 7000 100.0 90.0 80.0 5000 70.0 4000 60.0 50.0 3000 40.0 2000 30.0 20.0 1000 0 % pts Number of pts 6000 10.0 SW Glasgow W Glasgow N Glasgow West Dun E Glasgow East Dun East Ren Inverclyde SE Glasgow Patients 3380 4318 3000 3568 6183 3634 1757 3704 4563 Recorded 2964 3544 2414 2708 4683 2751 1251 2520 2851 Useable 2091 2632 2216 1934 3542 1444 1088 1137 2323 Healthy range 1609 2067 1697 1474 2731 1139 887 896 1799 % healthy range 76.9 78.5 76.6 76.2 77.1 78.9 81.5 78.8 77.4 % recorded 87.7 82.1 80.5 75.9 75.7 75.7 71.2 68.0 62.5 0.0 Support with stopping smoking: 30,988 (84%) patients had smoking status recorded in the past year. Overall, 7,476 (24%) of CHD patients were current smokers; however this ranged from 7.4% in the least deprived areas to 28.5% in the most deprived (Figure 10). Figure 10: Smoking in CHD patients, by deprivation quintile 5000 30.0 4500 Pts who smoke 3500 20.0 3000 2500 15.0 2000 10.0 1500 1000 % who smoke 25.0 4000 5.0 500 0 1 (Most deprived) 2 Smokers 4479 1438 % CHD pts who smoke 28.5 20.6 4 5 (Least deprived) 611 421 261 14.9 10.6 7.4 3 0.0 The proportion of CHD patients in whom smoking status was recorded ranged from 69% in SE Glasgow to 96% in SW Glasgow (Figure 11, overleaf). Around one third of smokers were recorded as wanting to stop, although again this varied from 17% in Inverclyde to 42% in North Glasgow. The proportion of all smokers referred to smoking cessation services ranged from 13% in Inverclyde to 61% in East 9 Renfrewshire; in four CHCPs, the number of smokers referred to smoking cessation services exceeded those wanting to stop. 1800 100.0 1600 90.0 1400 80.0 70.0 1200 % Number Figure 11: Documented support to CHD patients who smoke, by CHCP 60.0 1000 50.0 800 40.0 600 30.0 400 20.0 200 10.0 0 E Glasgow W Glasgow SW Glasgow N Glasgow Current smokers 1655 1065 921 815 781 Want to stop 605 380 323 343 225 Referred smoking cessation 717 530 366 214 % status recorded 84.2 92.7 95.7 % smokers referred 43.3 49.8 % who want stop 36.6 35.7 0.0 SE Glasgow East Dun East Ren 616 576 422 140 107 165 105 57 162 80 94 65 85 84.9 91.0 73.5 68.5 88.2 86.2 39.7 26.3 20.7 13.0 16.3 15.4 60.7 35.1 42.1 28.8 17.4 28.6 24.8 40.7 West Dun Inverclyde Recording of Body Mass Index (BMI): 23,940 (65%) patients had a BMI recorded in the past year. Of these, 2,236 (9.3%) were excluded from the analyses as their BMI fell outside a plausible range of 10-150. Of the remainder, the mean BMI was 28.5 and only 5,575 (26%) CHD patients were of healthy weight (BMI 18.5 – 25); this proportion decreased from 20 to 14% with increasing deprivation (Table 3). Table 3: Proportion (%) CHD patients with healthy weight SIMD Quintile 1 Most deprived 2 3 4 5 Least deprived TOTAL (known postcode) Number (%) 2228 (14.2%) 1114 (16.0%) 576 (14.0%) 684 (17.2%) 686 (19.6%) 5,288 (100% Figure 12: BMI in CHD patients, by CHCP 90.0 80.0 % CHD patients 70.0 60.0 50.0 40.0 30.0 20.0 10.0 0.0 East Ren East Dun SE Glasgow W Glasgow SW Glasgow E Glasgow % healthy BMI 30.4 30.1 28.1 27.1 25.3 24.2 23.7 23.0 22.4 % recorded 72.3 72.8 53.5 73.1 78.7 70.3 63.3 40.3 61.4 10 West Dun Inverclyde N Glasgow Assessment of mental health: Assessment of patients’ mental wellbeing, using HADS scoring for anxiety and depression, is an important component of the annual review. Valid reasons for excluding patients from this component of the review include ongoing psychological care, receipt of psychoactive medication or unsuitability for HADS scoring. During 2008/2009, 9,501 (25.8%) CHD patients were excluded for one of these reasons. Of those eligible, 12,873 patients (47%) had a recorded HADS score for anxiety and 12,825 (47%) for depression. Figure 14: % Eligible patients assessed for anxiety & depression, by CHCP 100.0 % patients with recorded HADS 90.0 80.0 70.0 60.0 50.0 40.0 30.0 20.0 10.0 0.0 East Ren East Dun W Glasgow SW Glasgow West Dun E Glasgow N Glasgow SE Glasgow Inverclyde % recorded (anxiety) 46.3 40.6 37.3 35.4 33.6 27.3 22.9 19.8 8.4 % recorded (depression) 46.6 40.9 38.1 36.2 34.1 27.6 23.0 20.6 8.2 Of the eligible patients with valid values, 514 (4%) had HADS scores suggesting significant anxiety (>12) and 263 (2%) had equivalent scores for depression. A substantial number of patients were reported to have declined HADS; 1,488 (12%) for anxiety and 1,475 (12%) for depression. Conversely, 41% of the patients excepted from HADS actually did have scoring performed (3,923 for anxiety and 3,937 for depression). There was some variation in these proportions across CHCPs, particularly in the proportions reported to have declined HADS (Figure 15). Figure 15: HADS scores for depression in CHD patients, by CHCP 11 Finally, there was a strong association between residential deprivation and poor mental health, as evidenced by HADS scores over 12 (Figure 16). Figure 16: % patients with significant anxiety & depression, by SIMD quintile 3.2: Stroke Of the 19,952 patients on the disease register, 4,653 (30.4%) were exception coded. Results presented below relate to the remaining 15,299 patients. 7,557 (49%) were male and 7,742 (51%) female. Women were, on average, slightly older (mean age 73.4 years) than men (mean age 70.8 years). Ethnicity information was available in 12,543 (82%) of patients. Overall, 12,219 (97.2%) were white (Table 4) Table 4: Non-exception coded stroke patients, by ethnic subgroup Ethnic subgroup White South Asian Black Chinese Other ethnic subgroups TOTAL (known ethnicity) Number (%) 12,219 (97.2%) 227 (1.8%) 10 (0.08%) 39 (0.3%) 48 (0.4%) 12,543 (100%) As with CHD, there were significant variations across GG&C in the ethnic composition of the stroke register (Figure 17) Figure 17: Spatial variations in ethnic distribution of diagnosed stroke patients 100% % White 100.0 90.0 80.0 70.0 60.0 50.0 40.0 30.0 20.0 10.0 0.0 90% GG&C average=97.2% 80% 70% 60% 50% 40% 30% Chinese 20% Black 10% South Asian 0% 12 Other The patient’s postcode of residence was known in 14,675 (96%) patients, allowing estimation of small area deprivation. The vast majority of GG&C’s stroke patients live in highly deprived areas, with an inverse relationship between age and deprivation (Figure 18). Figure 18: Mean age by SIMD deprivation quintile of diagnosed stroke patients Cholesterol monitoring: 11,093 (73%) patients had total cholesterol recorded in the past year, of whom 8,530 values were considered to be valid (2-15 mmol/l). Of these, 6,323 (74%) met the target cholesterol value (<5 mmol/l). There was considerable variation by CHCP in the proportion of patients monitored, ranging from 58% in SE Glasgow to 85% in SW Glasgow, however the proportion of patients who met the target cholesterol value was similar across the system (Figure 19). Figure 19: Cholesterol monitoring & outcomes in stroke patients, by CHCP Support with stopping smoking: 12,314 (80%) patients had smoking status recorded in the past year. Overall, 3,361 (27%) of CHD patients were current smokers; however this ranged from 9% in the least deprived areas to 30% in the most deprived (Figure 20, overleaf). 13 Figure 20: Smoking in stroke patients, by deprivation quintile The percentage of patients in whom smoking status was recorded ranged from 62% in SE Glasgow to 94% in SW Glasgow (Figure 21). The proportion of smokers recorded as wanting to stop varied from 21% in East Dunbartonshire to 41% in East Renfrewshire. The proportion referred to smoking cessation services ranged from 13% in SE Glasgow to 61% in East Renfrewshire; in four CHCPs, the number of smokers referred to smoking cessation services exceeded those wanting to stop. Figure 21: Documented support to stroke patients who smoke, by CHCP Recording of Body Mass Index (BMI): 9,463 (62%) patients had a BMI recorded in the past year. Of these, 842 (8.9%) were excluded from the analyses as their BMI fell outside a plausible range of 10-150. Of the remainder, the mean BMI was 27.7 and only 2,734 (31.6%) of stroke patients were of healthy weight (BMI 18.5 – 25), decreasing from 24 to 16% with increasing deprivation (Table 5). 14 Table 5: Proportion (%) stroke patients with healthy weight SIMD Quintile 1 Most deprived 2 3 4 5 Least deprived TOTAL (known postcode) Number (%) 1,090 (16.4%) 523 (17.6%) 302 (17.7%) 356 (20.0%) 367 (23.6%) 2,734 (100% Figure 22: BMI in stroke patients, by CHCP Assessment of mental health: During 2008/2009, 4,262 (27.9%) stroke patients were excluded from HADS assessment. Of those eligible, 4,908 patients (44.5%) had a recorded HADS score for anxiety and 4,895 (44.4%) for depression. Figure 23: % Eligible stroke pts assessed for anxiety & depression, by CHCP Of the eligible patients with valid values, 203 (4%) had HADS scores suggesting significant anxiety (>12) and 117 (2%) had equivalent scores for depression. 15 A substantial number of patients were reported to have declined HADS; 678 (13.8%) for anxiety and 670 (13.7%) for depression. Conversely, 40% of the patients excepted from HADS actually did have scoring performed (1,707 for anxiety and 1,693 for depression). There was some variation in these proportions across CHCPs, particularly in the proportions reported to have declined HADS (Figure 24). Figure 24: HADS scores for depression in stroke patients, by CHCP Finally, there was a strong association between residential deprivation and poor mental health. Figure 25 shows the proportion of stroke patients with HADS scores of greater than 12. Figure 25: % patients with significant anxiety & depression, by SIMD quintile 16 3.3: Type 2 Diabetes Of the 42,152 patients on the disease register, 7,647 (18.1%) were exception coded. Results presented below relate to the remaining 34,505 patients. 18,780 (54%) were male and 15,725 (46%) female. Women were, on average, slightly older (mean age 66.1 years) than men (mean age 63.2 years). Ethnicity information was available in 29,966 (87%) of patients. A higher proportion of diabetic patients (8.7%) were of nonwhite ethnic subgroups compared with 2.7 and 3.3 for stroke and CHD respectively (Table 6). Table 6: Non-exception coded Type 2 diabetic patients, by ethnic subgroup Ethnic subgroup White South Asian Black Chinese Other ethnic subgroups TOTAL (known ethnicity) Number (%) 27,365 (91.3%) 1,939 (6.5%) 127 (0.4%) 197 (0.7%) 535 (1.2%) 29,966 (100%) In contrast to patients on the CHD and stroke registers, non-white ethnic subgroups accounted for a substantial proportion of diabetic patients in some CHCPs, accounting for up to 28% (Figure 26). In some areas, patients of South Asian ethnicity were clearly predominant, whereas others were more diverse. Figure 26: Spatial variations in ethnic distribution of diabetic patients The patient’s postcode of residence was known in 32,996 (96%). In contrast to CHD and stroke, diabetic patients were less concentrated to GG&C’s most deprived areas, with only 2.5 years’ difference in mean age between patients resident in the most deprived areas compared with the most affluent (Figure 27). Figure 27: Mean age by SIMD deprivation quintile of diabetic patients 17 Cholesterol monitoring: 28,858 (84%) patients had total cholesterol recorded in the past year, of whom 20,963 (73%) values were considered to be valid (2-15 mmol/l). Of these, 15,472 (74%) met the target cholesterol value (<5 mmol/l). The proportion of patients monitored was more consistent across CHCPS compared with the stroke and CHD patient groups (Figure 28). Figure 28: Cholesterol monitoring & outcomes in diabetic patients, by CHCP Support with stopping smoking: 31,452 (91%) patients had smoking status recorded in the past year. Overall, 6,150 (20%) of diabetic patients were current smokers; however this ranged from 9.2% in the least deprived areas to 23.8% in the most deprived (Figure 29). Figure 29: Smoking in diabetic patients, by deprivation quintile Recording of smoking status in diabetic patients was more consistent across CHCPs compared with the other two disease areas (Figure 30, overleaf). The proportion of smokers recorded as wanting to stop ranged from 38% in East Glasgow to 51% in East Renfrewshire. The proportion of all smokers referred to smoking cessation services ranged from 9% in Inverclyde to 64% in East Renfrewshire; in five CHCPs, 18 the number of smokers referred to smoking cessation services exceeded those wanting to stop. Figure 30: Support to diabetic patients who smoke, by CHCP Recording of Body Mass Index (BMI): 27,364 (79%) patients had a BMI recorded in the past year. Of these, 2,873 (11%) were excluded as their BMI fell outside a plausible range of 10-150. Of the remainder, the mean BMI was 31.4. Only 3,282 (13%) were of healthy weight, a smaller proportion than the other disease areas, with little deprivation gradient (Table 7). Table 7: Proportion (%) diabetic patients with healthy weight SIMD Quintile 1 Most deprived 2 3 4 5 Least deprived TOTAL (known postcode) Number (%) 1,231 (12.4%) 666 (13.5%) 401 (13.3%) 419 (15.0%) 404 (15.3%) 3,282 (100% Figure 31: BMI in diabetic patients, by CHCP 19 Assessment of mental health: During 2008/2009, 9,169 (27%) diabetic patients were excluded from HADS assessment. Of those eligible, the proportion with recorded scores varied enormously across CHCPs (Figure 23). The average for GG&C as a whole was 38%, for both anxiety and depression assessment. Figure 23: % Eligible diabetic pts assessed for anxiety & depression, by CHCP Of the eligible patients with valid values, 432 (3%) had HADS scores suggesting significant anxiety (>12) and 240 (2%) had equivalent scores for depression. Around 11% of patients were reported to have declined HADS; 1,477 for anxiety and 1,450 for depression. Conversely, 40% of the patients excepted from HADS actually did have scoring performed (3,684 for anxiety and 3,671 for depression, with variations between CHCPs (Figure 24). Figure 24: HADS scores for depression in diabetic patients, by CHCP 20 Finally, in contrast to other disease areas, although there was some association between residential deprivation and poor mental health, this appeared to be strongly concentrated in the most deprived areas rather than an overall gradient, suggesting confounding with other cofactors (Figure 25). Figure 25: % patients with significant anxiety & depression, by SIMD quintile Assessment of glycaemic control: During 2008/2009, 22,650 (66%) diabetic patients had HbA1c measurements, of which 97% had valid values. Of these, 12,074 (55%) were in the target range of <7.5%. Recording was uniform across deprivation quintiles (Figure 26) Figure 26: % Recording of HbA1c, by residential deprivation quintile However, there was some evidence that glycaemic control was poorer among patients living in more deprived areas (Figure 27, overleaf). 21 Figure 27: % Achievement of HbA1c levels within ‘healthy’ range (<7.5%) 3.4 Discussion points This paper represents a first step in demonstrating the potential for understanding variations in the needs and characteristics of patients with chronic disease and in helping us to understand how our local healthcare system is responding to their needs. As powerfully demonstrated in each of the sections on clinical service delivery, there remain enormous health inequalities within our Board area, yet in several areas there is evidence of considerable progress in achieving more even distribution of intermediate clinical outcomes (such as cholesterol values) as a result of the LES programmes. In some areas, there is a clear need to do better, both in terms of data recording and, possibly to achieve more appropriate referral patterns to services, such as smoking cessation services. 3.5 Next steps We would be very grateful for commenst and feedback on the contents of this document. It is planned to release a series of further thematic issues that will address: Local report for North & South Lanarkshire Multiple morbidity in GG&C The challenge of overweight & obesity in patients with chronic disease The challenge of alcohol misuse in patients with chronic disease Blood pressure management – tackling the ‘rule of halves’ in GG&C Reducing the prevention gap in chronic disease management Impact of LES on CVD burden in GG&C Referral to health improvement services Finally, although every effort has been made to ensure accuracy of all data, there may be areas of omission or definitional issues that will be addressed in further editions as we continue to improve the quality and consistency of data collection, recording and analysis. 22