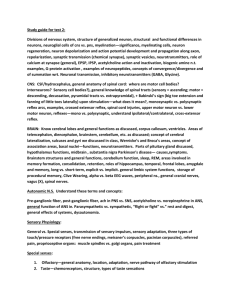
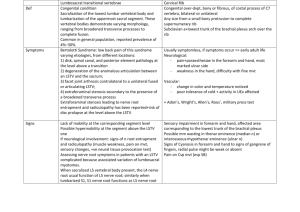
NEUROLOGIC INVESTIGATIONS
advertisement

NEUROLOGIC INVESTIGATIONS CSF Analysis CSF (general info): Produced by choroids plexus of ventricles, absorbed through villi of arachnoid granulations that project into the dural venous sinuses Production rate=.5 mL/min, total volume=150 mL, entire volume replaced every 5 hrs Lumbar puncture: CI: space occupying lesion causing mass effect, increased ICP (LP can cause cerebral or cerebellar herniation) CT: should be performed prior to LP (except in cases of suspected meningitis) Complication: low pressure HA is most common (tx: pt should lie flat, increase liquid intake and caffeine) Technique: o Pt position: lateral recumbent, legs flexed up over abdomen, pillow b/w legs o Level: L3-4 vertebral interspace (@ level of anterior superior iliac spine); spinal cord ends at L1-2 o Needle: inserted w/ bevel facing up, directed slightly rostrally to coincide w/ downward angulation of spinous process Interpretation of CSF findings: Normal CSF: clear, colorless fluid w/ glc content 2/3 that of blood, trace ptn, <5 cells present (lymphocytes), opening pressure of 60-150 mm water RBCs WBCs Elevated ptn Low glc Oligoclonal bands Positive EBV PCR No xanthocromia Xanthocromia (yellow discoloration of supernatant of spun CSF sample) Polymorphs Lymphocytes Traumatic tap SAH, hemorrhagic encephalitis Bacterial or early viral infection Infection (viral, fungal, mycobacterial), demyelination (MS), CNS lymphoma Infection, demyelination, tumor, age Bacterial or mycobacterial infection Demyelination (MS), CNS infections (Lyme Disease), Noninfectious inflammatory processes (SLE) Highly suggestive of CNS lymphoma in pts w/ AIDS or other immunosuppressed states CT Concept Characterizes degree of x-ray attenuation by tissue. Attenuation is the removal (by absorption or scatter) of x-ray photons and is quantified on an arbitrary scale (Hounsfield units) that is represented in shades of gray. Attenuation is dependent on atomic number and physical density of tissue. Axial or coronal plane Iodine is contrast agent used (if pt has allergy, do MRI instead); contrast enhancement indicates local disruption of blood-brain barrier Utility Initial investigation used in variety of neuro d/o (HA, trauma, seizures, SAH, stroke) Investigation of choice for demonstrating fresh blood Safety, tolerability, complications CI: pregnancy MRI Concept Uses radio frequency pulses (not x-rays). Images result from varying intensity of radio wave signals emanating from tissue in which hydrogen ions have been excited by a radio frequency pulse Pt is placed in a magnet and then a radio frequency (RF) is administered o TE=time to echo, the time interval at which the signal intensity is measured o TR=time to repetition, the time between RF pulses Gadolinium is contrast agent used Types T1-weighted o Short TE/TR o Fat is bright, water (CSF) is dark o Used to obtain gadolinium-enhanced images T2-weighted o Longer TE/TR o Water (CSF) is bright FLAIR (fluid attenuated inversion recovery) o Strong T2-weighted image, but one in which the signal from CSF has been inverted and is thus of low rather than high intensity o Used for demonstrating early or subtle T2 signal changes such as accumulation of edema Susceptibility-weighted imaging o Sensitive to the distruptive effect of a substance on the local magnetic field (calcium, bone, blood b/d products ferritin and hemosiderin); areas of increased susceptibility appear black Diffusion-weighted imaging (DWI) o Demonstrates cellular toxicity w/ high sensitivity o Most commonly used in diagnosis of acute stroke o Areas or restricted diffusion appear bright on DWI Utility Provides better anatomic definition Imaging of posterior fossa and craniocervical junction DWI is most sensitive for demonstrating early tissue ischemia and is useful in evaluation of pts w/ suspected stroke Safety, tolerability, complications Modality of choice in pregnancy When contrasted imaging is required, MRI may be preferable to CT when there is a history of allergy to IV contrast (gadolinium and iodine are not cross-reactive), or liver disease (gadolinium is not nephrotoxic) CI: metal objects, pacemaker/defibrillator devices, claustrophobia EEG Frequency patterns Alpha (8-13 Hz): posterior head regions in relaxed awake state w/ eyes closed Beta (14-30 Hz): frontal regions in relaxed awake state w/ eyes closed Theta (4-7 Hz): drowsiness/sleep Delta (.5-3 Hz): drowsiness/sleep Technique Montage=pattern w/ which electrodes are connected to each other o Bipolar: all electrodes are active, records difference in electrical activity b/w 2 adjacent electrodes o Referential: electrical activity recorded beneath the active electrode relative to a distant or common average electrode Clinical utility Limitations o Abnormal EEGs rarely are etiology-specific o EEG records electrical activity of cortical neurons, and thus surface EEG may be insensitive to dysfunction of deep structures o Interictal EEG may only be abnormal in 30% of adults w/ epilepsy Abnormal patterns o Focal arrhythmic or polymorphic slow activity in theta/delta range local pathology in underlying brain o Generalized arrhythmic slow activity diffuse encephalopathy o Sharp and spike wave discharges w/ or w/o accompanying slow wave interictal epileptiform findings o Rhythmic spike or sharp and slow wave discharges or rhythmic slow waves focal or generalized electrographic seizures Nerve Conduction Studies (NCS) Electrical stimulus applied over a nerve, and recordings are made from surface skin electrodes o Motor study: recording electrodes placed over end plate of a muscle innervated by nerve being stimulated; nerve stimulated in at least 2 locations (distal, proximal) and distance b/w 2 sites is measured Distal latency=time interval b/w stimulation over distal portion of nerve and initiation of CMAP CMAP=compound muscle action potential Conduction velocity=calculated by measuring the difference in latency to CMAP initiation b/w proximal and distal sites of stimualtion o Sensory study: nerve stimulated at one site; SNAP (sensory nerve AP) recorded either at more proximal site (orthograde study) or more distal site (antergrade study) Utility: assists localization of pathology w/in PNS Distal latency Conduction velocity CMAP amplitude EMG Nerve Conduction Studies in Demyelinating and Axonal Neuropathies Demyelinating Axonal Prolonged Normal Markedly reduced Normal; maybe slightly reduced Normal or mildly reduced Reduced Needle is inserted into individual muscles; recordings are made of muscle electrical activity upon insertion (insertional activity), while muscle is at rest (spontaneous activity) and during contraction (volitional motor unit potentials) Utility: assists localization of pathology w/in PNS Insertional activity Spontaneous activity Volitional motor unit potentials Recruitment EMG in Neurogenic and Myopathic Disorders Neurogenic Myopathic Increased (active denervation) Usually normal Increased (necrotizing myopathies) Increased (active denervation) Usually normal Increased (necrotizing myopathies) Large amplitude, polyphasic Small amplitude, polyphasic Reduced Usually normal THE APPROACH TO COMA AND ALTERED CONSCIOUSNESS General Coma=state of unarousable unresponsiveness Describe alterations of consciousness in terms of a pt’s responses to various degrees of stimulation Glasgow Coma Scale—has prognostic value in head trauma pts, is reproducible, and easy to use Clinical Approach to Altered Consciousness 1. ABCs: airway, breathing, circulation 2. Look for obvious clues to etiology a. Medical problems (diabetes, hepatic failure, seizure disorder) b. Circumstances in which patient was found c. Check for meningeal signs 3. Try reversing common reversible etiologies a. Naloxone (opiate OD) b. Thiamine (EtOH)—give before dextrose, which can precipitate Wernicke’s encephalopathy c. Dextrose 4. Check brainstem reflexes and look for focal signs a. Focal signs present suspect structural cause neuroimaging b. Focal signs absent suspect diffuse cause metabolic, toxic and/or infectious workup, neuroimaging Examination 1. Mental status testing a. Assess level of consciousness—an increasing gradient of stimulation should be applied and patient’s responses recorded b. For many pt’s, further cognitive testing may be impossible 2. Cranial nerve testing to assess brainstem function. Test these bs reflexes: a. Pupillary—II (afferent) III (efferent) b. Oculocephalic (doll’s eyes)—VIII (afferent) III, IV, VI (efferent)—forcibly turn head horizontally and vertically and observe for conjugate eye movement in opposite direction (CI if cervical spine injury not r/o) c. Caloric testing (if necessary, i.e., if turning head is CI or does not result in eye movement; never assume eyes are immobile unless caloric testing has been done)—inject 50 mL ice water into each ear and observe for conjugate eye deviation toward the ear injected d. Corneal—V (afferent) VII (efferent) e. Gag—IX (afferent) X/XI (efferent) 3. Motor tone a. Motor tone b. Decorticate posturing—bs dysfunction slightly more superior that that of decerebrate posturing c. Decerebrate posturing—bs dysfunction 4. 5. Muscle stretch reflexes, Babinski sign Sensory testing usually limited to testing of light touch or pain sensation; applying nailbed pressure to each limb may be useful in looking for gross sensory abnormalities Differential Diagnosis General: 2 ways in theory in which consciousness can be depressed: dysfunctional bs (e.g. pontine hemorrhage) or bilateral cerebral hemisphere dysfunction (e.g. hypoglycemia); BUT, unilateral cerebral hemisphere lesions, if large or severe enough to cause swelling and compression of opposite hemisphere or downward pressure on bs, can also lead to coma General approach o +/- bs reflexes indicates how deep coma is o +/- focal signs narrows differential and guides workup Structural causes of depressed consciousness: acute ischemic stroke, acute intracranial hemorrhage, brain tumor (w/ edema or hemorrhage), brain abscess Diffuse causes of depressed consciousness: metabolic, toxic, infectious, hypoxic-ischemic (respiratory failure, cardiac arrest) Laboratory and Radiographic Studies If STRUCTURAL cause is suspectedurgent head imaging, usually w/ noncontrast head CT; use CT rather than MRI even if focal brainstem signs are found (d/t possibility of a large cerebral hemisphere lesion compressing the bs) If DIFFUSE cause suspected extensive metabolic, toxic, or infectious workup o Blood testing: CBC, electrolytes, glc, liver function tests o If infection suspected: chest x-ray, urinalysis, blood or urine culture, LP (BUT perform CT 1 st! to avoid precipitating brain herniation) o Head imaging usually needed b/c it may demonstrate signs of global hypoxic-ischemic injury, diffuse cerebral edema, or bilateral lesions mimicking a diffuse process EEG nonspecific, but can be of use in helping to assess how deep a coma is, based on degree of background slowing Treatment and Prognosis Treatment Diffuse metabolic, infectious, toxic medical management Structural neurosurgical intervention If ICP increased raise head of bed, hyperventilation, osmotic diuretics (mannitol), corticosteroids for edema a/w brain tumors Prognosis Depends on o Etiology o Age Special Topics 1. Persistent vegetative state—may follow prolonged coma and is characterized by preserved sleep-wake cycles and maintenance of autonomic functions w/ absence of awareness and cognition 2. Locked-in syndrome—awareness and cognitive function are preserved but almost complete paralysis occurs; cause by large lesions in base of pons 3. Brain death—irreversible cessation of all functions of the entire brain, including the brainstem a. Comatose b. Absent bs reflexes c. No spontaneous respirations even when PCO2 has been allowed to rise (apnea test) NEURO-OPHTHALMOLOGY Anatomy Coherent visual image: retinal axons lateral geniculate nucleus optic radiations in cerebral cortex primary visual cortex (visual area 1, Brodmann’s area 17, striate cortex). V1 receives visual info from contralateral visual hemifield. Perception of motion, depth, color, location, form: V1 o Associative visual cortex (areas 18, 29) o Higher-order centers in posterior parietal and inferior temporal cortices Visual Loss +/- visual phenomena 1. Positive: brightness, shimmering, sparkling, hallucinations, shining, flickering, colors (suggest migraines or seizures) 2. Negative: blackness, grayness, dim vision, shade-obscuring vision (suggests stroke, TIA) Clinical evaluation of visual loss 1. Visual acuity problem in refractive apparatus of eye or optic nerve a. Hand-held Snellen b. Pinhole (if VA is poor) if pinhole test improves VA, then problem is in refraction c. If pt cannot read the letters count fingers perception of movement perception of bright light 2. Assessment of color vision a. Ishihara plates (red desaturation seen early in optic nerve problems [esp. optic neuritis]) 3. Test for afferent pupillary defects a. Size of pupil (anisocoria?) b. Light reaction, direct and consensual c. Accomodation (near reaction) 4. Visual fields 5. Ophthalmoscopic exam retinal nerve fiber layer damage, optic atrophy, swollen disc, abnormal disc, vascular lesions, retinal emboli Monocular visual loss v. binocular visual loss Monocular suggests problems in eye, optic nerve, or chiasm Binocular suggest chiasm or retrochiasmal lesion Visual Loss According to Localization Lesion Level Visual Field Defect Optic nerve Ipsilateral blindness Chiasm Bitemporal visual field defect (tunnel vision) Optic tract Contralateral homonymous hemianopia Optic radiations (parietal) Contralateral inferior homonymous quadrantonopia Optic radiations (temporal, or Meyer’s loop) Contralateral superior homonymous quadrantonopia Optic radiations (both) Contralateral homonymous hemianopia Occipital cortex Contralateral homonymous hemianopia w/ macular sparing Disorders of the Pupil Anatomy Light retinal ganglion cells optic nerve optic chiasm optic tract pretectal midbrain nuclei (EdingerWestphal) in rostral portion of 3rd nerve Efferent PNS fibers from EW travel w/ CNIII (thru cavernous sinus), ultimately synapsing in ciliar ganglion sphincter pupillae (constrictor) SNS innervates dilator pupillae o 1st order neuron: ipsilateral posterolateral hypothalamus down brainstem to IML @ C8-T1 spinal level o 2nd order neuron: synapse in superior cervical ganglion o 3rd order neuron: travel along internal carotid into cavernous sinus orbit Clinical Assessment Condition Physiologic anisocoria Horner’s syndrome Signs/Symptoms Asymmetric pupils Etiology Up to 25% of normal people Ipsilateral miosis, ptosis, ipsilateral anhidrosis Impaired SNS innervation of pupil CNIII palsy (complete) Mydriasis, ptosis, ophthalmoplegia Compression of CNIII: initially produces dilated pupil w/o compromising eye movements (b/c PNS fibers run in outer part of CNIII, while motor fibers are more internal) Vascular compromise CNIII Test Amount of anisocoria does not change with different illumination Cocaine eyedrops that fail to dilate the abnormal pupil (neg) Hydroxyamphetamine eyedrops allows for pharmacologic localization if cocaine test is neg pre- v. postganglionic Horner’s (the pupil w/ post-gang Horner’s fails to dilate) Adie’s pupil (tonic pupil) Dilated, with segmental contraction and light-near dissociation; anisocoria, photophobia, blurred near vision Argyll Robertson pupils Small, poorly reactive to light but have preserved near response (accommodation normal) ischemia (diabetes): normal, reactive pupil, but palsy of ocular muscles innervated by CNIII Interruption of PNS supply arising from ciliary ganglion LND: normally pupil constriction to light greater than to near stimulus; opposite is true in LND (present when there is a defect in light response as in optic neuropathy or d/t aberrant regeneration as in tonic pupil) Syphilis Abnormal Optic Disc See pages 38-39 (table) Note: painful vision loss=optic neuritis; sudden painless vision loss=ischemia Diplopia Strabismus Comitant strabismus Noncomitant strabismus Phoria Tropia Some Terms Used to Describe Eye Misalignment Misalignment of eyes Misalignment is constant in all directions of gaze, and each eye has full ROM (ophthalmologic problem) Degree of misalignment varies w/ direction of gaze (neurologic problem) Misalignment of eyes when binocular vision is absent Misalignment of eyes when both eyes are opened and binocular vision is possible Anatomy of Eye Movements (SO4 LR6 AR3) CNIII: dysfunction produces droopy dilated down and out; most common cause of CNIII dysfunction in older adults include microvascular occlusion and ischemia d/t HTN, diabetes mellitus and atherosclerosis; patterns of dysfunction include o CNIII nucleus: bilateral ptosis, weakness of contralateral superior rectus o Subarachnoid space: meningismus, constitutional sxs, CN defects o Tentorial edge compression: depressed level of consciousness, hemiparesis, hx of trauma or supratentorial mass lesion CNIV: superior oblique intorts, depresses, adducts; dysfunction is worse on downgaze and pts c/o diplopia while reading and descending stairs and compensate w/ a contralateral head tilt (diplopia improves w/ head tilt away from side of lesion CNVI: lateral rectus; o Lesions produce esotropia o Destruction of abducens nucleus in brainstem ipsilateral conjugate gaze palsy b/c of damage of interneurons connected to contralateral 3rd nerve through the MLF (medial longitudinal fasciculus) Clinical Evaluation of Diplopia Ask: o Monocular or binocular? o If binocular, is it horizontal or vertical? o Is it worse near or far? o Is the problem localized to an extraocular muscle (paresis or fatigue), brainstem MLF (internuclear opthalmoplegia), or to the orbit itself? Tests o Cover test: detects a tropia; pt fixates on a small target, then cover one eye; watch other eye; if eye makes a refixation movement, this means that this eye was not aligned on the target; if eye moves nasally, pt has an exotropia, and if temporally, and esotropia; e.g. CNIII palsy exotropia and hypotropia of paretic eye; CNVI palsy produces esotropia of affected eye o Alternate cover test: detects phoria (eso or exophoria); phoria do not cause diplopia b/c eyes are aligned when both are opened simultaneously o Park’s 3-step test: detects CNIV palsy; 1) hypertropia of paretic eye 2) which increases when the pt looks to the opposite side and when 3) pt tilts the head to the same sider o Oculocephalic maneuver (doll’s eye test) o Saccades: rapid conjugate movement of the eyes between objects (fingertips); in general d/o of eye movements will produce slowness of saccades in the direction of the paretic muscle Pupillary size and reflexes Periocular signs or proptosis o o Horizontal Gaze Internuclear opthlamoplegia (INO) o MLF connects CNVI nucleus w/ contralateral CNIII nucleus o Clinical characteristics of a RINO Inability to adduct R eye in left lateral gaze Nystagmus of abducting left eye Adduction during convergence is maintained b/c this action does not depend on the MLF o Bilateral INOs can be seen in Wernicke’s encephalopathy “One and a half syndrome” o D/t lesion of ipsilateral MLF + ipsilateral PPRF (paramedian pontine reticular formation=premotor substrate for ipislateral horizontal gaze) OR CNVI nucleus; causes are MS and brainstem ischemia o Clinical characteristics Ipsilateral lateral gaze palsy and INO in contralateral lateral gaze The only movement present in the lateral plane is abduction of contralateral eye Vertical Gaze Controlled by rostral interstitial nucleus of the MLF (riMLF) located in the pretectal area near CNIII nucleus. Fibers controlling upgaze from riMLF cross to contralateral side using posterior commisure to communicate w/ inferior oblique and superior rectus subnuclei of CNIII complex Abnormal vertical gaze movements d/t dorsal midbrain syndromes o Parinaud’s syndrome: upgaze disturbance, convergence-retraction nystagmus on attempted upgaze, lightnear dissociation of pupils (d/t pineal tumor compressing dorsal midbrain) o Skew deviation: vertical tropia d/t brainstem or cerebellar lesion; hypotropic (lower) eye often on side of lesion Supranuclear Eye Movements Saccades: rapid eye movements that redirect the fovea to a new target Voluntary horizontal saccades originate in frontal eye field and superior colliculus contralateral to the direction of gaze; these areas have direct connection to contralateral PPRF Vertical saccades may also originate in frontal eye fields or superior colliculus but connect to contralateral riMLF Ocular motor apraxia=inability to produce saccades Abnormal saccades: hypermetric (overshoot), hypometric (undershoot); see table 4-6 on p. 42 Pursuit Movements: permit eyes to conjugately track a moving visual target to keep it in focus Control is hemispheric and ipsilateral Vestibulo-ocular Reflex (VOR): coordinates eye movements w/ head movement, allowing visual image to not slip during head movement Semicircular canals (rotation) and otoliths (linear acceleration)vestibular nucleiabducens nuclei CN III/IV via MLF Abnormalities of VOR result in nystagmus: Nystagmus: rhythmic to-and-fro movement of the eyes Types o Rhythmic o Jerk: eye drifts away from fixation in a pursuit-like movement and returns with a fast, saccadic movement; the direction of nystagmus is named by the direction of the saccadic fast component Etiologies o Congenital o Physiologic o CNS dysfunction, peripheral vestibular loss, visual loss Peripheral: usually unidirectional, w/ fast phase away from the side of the lesion; combines horizontal and torsional movements and is inhibited by fixation; tinnitus or deafness often present; severe vertigo; duration is short by recurrent Central: normally bi-directional, often purely horizontal, vertical, or torsional, and not inhibited by fixation; tinnitus and deafness rarely present; mild vertigo; duration may be chronic See table on p. 43 (4-7) THE APPROACH TO WEAKNESS Approach to Weakness Flowchart 1. Make sure that true weakness (i.e. decreased strength) is the complaint (NOT general sense of fatigue, NOT clumsy or numb, NOT a limb that is too painful to move) 2. ID which muscles are weak 3. Determine the pattern of weakness (muscle, NMJ, nerve, root, plexus, cord, brain?) 4. Look for associated signs/symptoms (numbness, tingling, painful; reflexes?). Are they consistent with localization? 5. Consider the differential diagnosis of d/o w/in your localization 6. Use lab tests and EMG/NCS if needed a. Blood tests or neuroimaging b. EMG/NCS to further localize problem to a particular segment of the peripheral nervous system Differential Diagnosis of Weakness Anatomic Location Primary Muscle NMJ Peripheral Nerve Mononeuropathies Mononeuropathy Multiplex Polyneuropathy Nerve Root Pattern of Weakness Associated Si/Sx Lab Studies Symmetric, proximal weakness and can affect neck muscles (not usually affected in a brain or nerve lesion) Distal muscles affected later or not as severely Proximal weakness; some can lead to ptosis and weakness of extraocular, bulbar, and neck muscles Fluctuation of weakness is important—degree may change from hr to hr, may be worse after using muscles or toward end of day and improve after resting or in the morning (fatiguability) or improve after exercise Muscle pain (if process is inflammatory, e.g. polymyositis) Sensory si/sx are not present Sensory si/sx are not present ANS features sometimes present Serum CK level is elevated in some d/o EMG may show characteristic “myopathic” pattern Weakness of muscles innervated by a single peripheral nerve Sensory sxs (e.g. numbness, tingling, pain) in distribution of the peripheral nerve Characteristically a/w pain EMG/NCS: confirm clinical suspicion of problem w/ peripheral nerve NCS: does the pathologic process involve axons or myelin of the nerve EMG: relative acuity or chronicity of d/o Certain systemic d/o can lead to dysfxn of multiple peripheral nerves in succession Peripheral nerves are all affected diffusely, w/ dysfxn occurring in longest nerves 1st (progression of weakness from distal to proximal, symmetric) Usually have associated sensory loss and depressed or absent reflexes, especially in distal extremities EMG/NCS can demonstrate nearly pathognomonic findings for some d/o Some d/o have specific serum markers (anti-AChR Igs in myasthenia gravis) Differential Diagnosis Acquired (myopathies) d/t inflammatory or toxic etiology Congenital (muscular dystrophies) Myasthenia Gravis Lambert-Eaton Myasthenic Syndrome Usually occur d/t entrapment (e.g. Carpal Tunnel Syndrome) A/w systemic vasculitis, metabolic, or rheumatologic d/o Demyelinating polyneuropathies can be hereditary (Charcot-MarieTooth) or acquired (Guillain-Barre) Radiculopathy Dysfxn of single nerve root Pain or tingling radiating out from back or neck Objective sensory loss rare in d/o of single nerve root b/c of overlap from adjacent roots If nerve root subserves a particular muscle stretch reflex, that reflex may be depressed or absent EMG/NCS can confirm that nerve roots are the culprit; can differentiate b/w root v. peripheral nerve problem MRI (spine): for single rad., to r/o structural etiologies LP: for polyrad. to look for infectious or inflammatory processes Herniated discs Shingles Inflammation Infection Polyradiculopathy Dysfxn of multiple nerve roots Multiple muscles in a limb are weak and do not conform to a particular nerve root or peripheral nerve pattern Sensory findings (in distribution of one or more roots or nerves) Dropped reflexes EMG/NCS: confirms the localization MRI of brachial or lumbosacral plexi to r/o mass lesions Spinal Cord Weakness in UMN pattern below lesion, and in a nerve root pattern at lesion level MRI (spine): r/o structural etiologies or demonstrate intrinsic inflammation LP: evaluate infectious or inflammatory etiology Cerebral Hemispheres/ Brainstem Hemisphere: contralateral side in UMN pattern Parasagittal: contralateral leg Lateral hemisphere: arm and face Deep hemisphere (e.g. internal capsule): legs, arms, and face Base of pons: ipsilateral face, contralateral arm, leg (crossed signs) b/c descending motor fibers to face have crossed at that level by those to body have not Maybe sensory loss below level of lesion d/t interruption of ascending tracts Reflexes below lesion are typically increased, and Babinski may be + Bladder/bowel incontinence maybe Cognitive signs Idiopathic inflammation, radiation, metastases, hemorrhage, trauma Diabetic pts characteristic lumbosacral plexopathy (diabetic amyotrophy) Inflammation (e.g. transverse myelitis) Infarction Compression ALS (degeneration of corticospinal tracts and anterior horn cells) Plexus Brachial Lumbosacral Left hemisphere: aphasia, apraxia Right hemisphere: neglect, visuospatial dysfunction Brainstem: CN dysfunction CT or MRI Stroke, demyelinating disease, traumatic injury, tumor, infection THE SENSORY SYSTEM Anatomy of Sensory Pathways Modality Tract Pain and temperature Spinothalamic tract Proprioception, vibration, light touch Dorsal columns 1st order neuron Synapse at level of dorsal horn of spinal cord 2nd order neuron Cross and travel contralaterally in STT Terminates in thalamus Legsarms Mediallateral Travel ipsilaterally in dorsal column system reaching 2nd order neuron at level of medulla in nuclei gracilis and cuneatus Axons from nuclei gracilis and cuneatus cross at lower medulla to form the medial lemniscus Nucleus gracilis Nucleus cuneatus Medial lemniscus Facial sensation Somatotopic Arrangement Sacralcervical Lateralmedial CNV Legsarms Lateralmedial 3rd order neuron Cortical projections to postcentral cortex Fiber type Thinly myelinated and unmyelinated slowly conducting fibers (Adelta and C) Heavilymyelinated Aalpha and Abeta) Terminates in thalamus Examining the Sensory System Touch wisp of cotton Pain pin Joint position sense/proprioception moving great toe up and down, moving object up or down on skin and asking pt the direction of movement Vibration 128-Hz tuning fork applied to toes and other bony structures Temperature cold tuning fork Sensory Abnormalities: Terms Paresthesia Dysesthesia Hyperesthesia Hypoesthesia Allodynia Dissociated sensory loss Negative symptoms Positive symptoms Abnormal sensation described by pt as tingling, prickling, pins and needles, etc. Unpleasant sensations triggered by painless stimuli Increased sensitivity to sensory stimuli Diminished sensitivity to sensory stimuli Pain provoked by normally innocuous stimuli Loss of one of sensory systems w/ preservation of another one, e.g. in a central cord syndrome, you will get loss of pain and temperature (STT) w/ preservation of light touch, proprioception, and vibration sense (dorsal columns) Numbness, loss of cold/warm sensation, blindness, deafness (d/t disruption of nerve excitation) Pain, paresthesias, visual sparkles, tinnitus (d/t excitation or disinhibition) Approach to Pt with Sensory Loss Recognize sensory abnormality by modality Judge level at which the abnormality is produced Establish a diff dx of pathologic processes that can affect the particular modality/sensory system Establish the cause: primary neurologic disease OR systemic disease Patterns of Sensory Loss According to Localization Site of Lesions Sensory Findings Peripheral nerve Loss of LT, T, PP, proprioception in influenced area Root Loss of all sensory modalities in a dermatomal distribution Plexus Sensory loss in distribution of 2 or more peripheral nerves Spinal cord Sensory level: bilateral loss of all sensory modalities Sensory dissociation Contralateral hypesthesia and ipsilateral loss of proprioception (Brown-Sequard syndrome) Proprioceptive loss and corticospinal tract involvement Saddle anesthesia Ipsilateral facial numbness and contralateral body numbness Brainstem Other Neurologic Abnormalities Associated weakness in muscles innervated by that nerve; distal muscle weakness, atrophy, areflexia (LMN signs) Weakness in a myotomal distribution, atrophy, segmental hyporeflexia Muscle weakness that cannot be localized to a single nerve or root Paraplegia, tetraplegia; initially areflexia, then hyperreflexia below the lesion and Babinski sign (UMN signs) Examples Peroneal neuropathy Median and ulnar neuropathies L5 radiculopathy Cervical radiculopathy Brachial plexopathy d/t trauma, inflammation, infiltration, etc. Myelopathy Central cord syndrome Brown-Sequard syndrome Alternating hemiplegia; CN findings, INO, ataxia Thalamus Hemibody anesthesia May have motor findings Posterior limb of internal capsule Hemibody anesthesia Hemiplegia Cortex All modalities affected on contralateral side Sensory neglect Agraphesthesia Psychogenic Hyperesthesia for one modality in one area w/ anesthesia for another modality in same area; changing sensory findings Nonphysiologic sensory level changes (abrupt midline changes, vibration asymmetry over forehead) Any Posterior circulation strokes Tumor Lacunar stroke Hemmorhage Lacunar stroke Hemorrhage Tumor Parietal stroke Hemorrhage AVM Psychogenic (a diagnosis of exclusion) VERTIGO AND DIZZINESS “Dizziness” Vertigo: illusion or hallucination of movement that is usually rotatory, but may be linear Light-headedness: feeling faint, refers to presyncopal state Dysequilibrium: sensation of imbalance or unsteadiness usually referable to legs rather than to a feeling inside head Vertigo D/t acute asymmetry of neural activity b/w L and R vestibular nuclei Does NOT result from slow unilateral loss of vestibular fxn (acoustic neuroma) or from symmetric bilateral loss of fxn (ototoxic drugs) Approach to determining etiology o Periodicity/duration of sxs o Positional or spontaneous sxs o Peripheral or central origin Peripheral tinnitus, hearing loss; accompanying N/V more prominent Central diplopia, dysarthria, dysphagia, or other sxs of brainstem dysfunction; ability to walk or maintain posture may be more impaired Spontaneous Vertigo: Single prolonged episode Vestibular neuronitis Acute unilateral (complete or incomplete) peripheral vestibulopathy; sudden and spontaneous onset of vertigo, N/V; onset over min-hrs, peak w/in 24 hrs, sxs improve gradually over several days/wks; nystagmust is strictly unilateral and may be suppressed by visual fixation; recovery represents central compensation for loss of peripheral vestibular fxn Labyrinthine concussion Can result from head injury; vertigo sometimes accompanied by hearing loss and tinnitus Infarction of labyrinth, Blood supply to central/peripheral vestibular systems via vertebrobasilar system (posterior and brainstem, or cerebellum inferior cerebellar aa. and superior cerebellar artery) and to inner ear via anterior inferior cerebellar artery (infarction of inner ear sudden onset of deafness or vertigo or both) Brainstem or cerebellar stroke most important diff dx in pts w/ suspected acute vestibular neuronitis; if a central-type nystagmus is present, then cerebellar or brainstem infarction w/ associated CN si/sx, weakness, ataxia, or sensory changes that clearly indicate a central process Spontaneous vertigo: recurrent episodes Meniere’s disease Episodic vertigo w/ N/V; fluctuating, but progressive hearing loss, tinnitus, and a sensation of fullness or pressure in ear; d/t an intermittent increase in endolymphatic volume Perilymph fistula D/t disruption of lining of endolymphatic system; pt reports hearing “pop” at time of a sudden increase in middle ear pressure w/ sneezing, noseblowing, coughing, or straining, which is followed by abrupt onset of vertigo Migraine Positional vertigo: peripheral BPPV (benign positional Episodes precipitated by changes in position such as turning over in bed or looking upward; paroxysmal vertigo) attacks are brief (sec-min), and sxs typically begin after a few seconds’ latency following change in position; d/t freely moving Ca++ carbonate crystals w/in one of semicircular canals; when head is stationary, they settle in most dependent part of canal (posteriorly); w/ head movements, they move slower than endolymph w/in which they lie, and their inertia once the head comes to rest causes ongoing stimulation of the hair cells that results in the illusion of movement (vertigo); Dix-Hallpike test is diagnostic (downbeating and torsional nystagmus); Epley maneuver can be used to remove crystals from posterior canal Syncope Transient LOC and postural tone d/t brain hypoperfusion o Hypotension d/t cardiac dz o Low intravascular volume o Excessive vasodilation Presyncopal sxs include: light-headedness, HA, neck pain, blurring of vision, cognitive slowing, buckling of knees 2 neurologic varieties (both involve ANS dysfunction) o Neurogenic syncope (more common): acute hypotension results from transient failure of ANS cardiovascular control; an acute hemodynamic rxn involving a reflex that is triggered by excessive afferent discharges from arterial (including heart and great vessels) or visceral mechanoreceptors; efferent impulses via vagus lead to cardio-inhibition and vasodepression that result in hypotension and bradycardia Micturition syncope trigger is rapid emptying of distended bladder Carotid sinus hypersensitivity trigger is compression of carotid sinus Neurocardiogenic syncope vigorous contraction of an underfilled ventricle Vasovagal syncope trigger is strong emotions or pain o Neurogenic orthostatic hypotension: d/t persistent ANS failure; d/t intravascular volume depletion (dehydration, Addison’s disease) or d/t inability to activate efferent SNS fibers appropriately upon assumption of the upright posture; the underlying pathology is either primary or secondary ANS failure (e.g. d/t diabetic ANS neuropathy), but the hallmark of both is failure to release noradrenaline upon standing; consider contribution of drugs such as diuretics, antihypertensives, vasodilators, and antidepressants; drug management to ameliorate sxs include midodrine and fludrocortisone ATAXIA AND GAIT DISORDERS Ataxia vs. Other Gait Disorders Ataxia: general term describing manifestations of dz of cerebellum or its connections Other: NOT ALL ataxia is cerebellar in origin, e.g. de-afferentation resulting from loss of position sense also results in ataxia THUS: distinguish b/w cerebellar v. sensory ataxia Ataxias General Vermal lesions truncal/gait ataxia Hemispheric lesions ipsilateral limb ataxia Si/Sx of Cerebellar Disease Dysmetria abnormality of range and force of movement; manifests as erratic, jerky movements w/ over- and undershooting the target (limb or ocular dysmetria) Intention tremor rhythmic side-to-side oscillations of the limb as it approaches the target Dysdiadochokinesia abnormality of rate and rhythm of movement demonstrated by rapid alternating movement test Gait ataxia broad-based and unsteady, w/ inability to walk in straight line and tendency to lurch from side to side Truncal ataxia impaired control of truncal posture; when severe, unable to even site unsupported Dysarthria slow scanning and monotonous speech Nystagmus Diseases Disease Cerebellar hemmorhage/ infarction Etiology Hemorrhage/infarction Characteristics Abrupt onset of vertigo, vomiting, inability to walk Postinfectious cerebellitis Typical b/w ages 2-7 following varicella or viral infection Episodic ataxias Inherited mutations in Ca++ and K+ channels Underlying gynecologic or small cell lung cancer Acute onset of limb and gait ataxia, dysarthria; severity ranges from mild unsteadiness to inability to walk Brief episodes of ataxia, vertigo, N/V Acute/subacute onset of pancerebellar syndrome w/ truncal, gait, limb ataxia; dysarthria; ocular dysmetria and nystagmus Vermis bears brunt of damageprogressive gait and truncal ataxia evolving over wks-mo Paraneoplastic cerebellar degeneration Alcoholic cerebellar degeneration Long-standing alcohol abuse; most common cause of acquired cerebellar degeneration Friedrich’s ataxia AR, inherited, childhood onset Progressive, affects arms>legs; severe dysarthria AD spinocerebellar degenerations AD, inherited, onset in young adult life D/t trinucleotide CAG expansion Miller-Fisher Syndrome Variant of GuillainBarre syndrome (mediated by postinfectious immune process) Insidious onset of progressive impairment of gat and dysarthria in young adult life Triad of ataxia, areflexia, ophthalmoplegia Ass. Si/Sx Level of arousal may be depressed if 4th ventricle is compressed w/ hydrocephalus or if there is pressure on BS Course + Prognosis Medical emergency Lasts a few weeks, recovery is usually complete MRI usually normal Anti-Yo, anti-Hu autoantibodies in serum Disease peaks in a period of weeks then stabilizes, leaving patient w/ profound disability Alcoholic polyneuropathy Cessation of drinking and supplementation of nutrition offer the best (though limited) chance of improving Loss of reflexes, spasticity, extensor plantar responses, impaired vibration and position sense Mild to moderate cognitive decline is a late feature IgG anti-GQ1b antibodies in serum of >90% Self-limiting Usually full recovery Gait Disorders Gait Disorder Hemiplegic Anatomical Location Brainstem Cerebral hemisphere Paraplegic Spinal cord Akinetic-rigid Bihemispheral Basal ganglia Frontal Frontal lobes Subcortical Waddling Hip-girdle weakness Sensory Ataxia (Slapping) Large-fiber neuropathy Dorsal columns Description Pathology Affected leg is stiff and does not flex at hip; leg is circumducted, w/ tendency to scrape floor w/ toes; arm is held in flexion and adduction and does not swing freely; the spastic (paraparetic) gait is essentially that of a bilateral hemiplegia; adductor tone is increased, and legs tend to cross during walking (scissoring gait) Stroke, tumor, trauma Demylination (MS), transverse myelitis, compressive myelopathy Stooped posture; narrow-based, slow, shuffling gait w/ small steps and reduced arm swing; arms carried flexed and slightly ahead of body; difficulty w/ gait initiation; postural reflexes are impaired and pt may take series of rapid small steps (festination) forward (propulsion) or backward (retropulsion) in an effort to preserve equlibrium Flexed posture; feet may be slightly apart; gait initiation is impaired, and word “magnetic” describes difficulty lifting feet off ground; pt advances w/ small, shuffling, and hesitant steps; w/ increasing severity, pt may make abortive stepping movements in one place w/o ability to move forward D/t loss of proprioceptive input from feet; cautious, wide-based gait; slow steps; contact w/ ground is made by heel and forefoot then strikes floor w/ a slapping sound (slapping gait); walking on uneven surfaces or in dark is especially difficult Diffuse anoxic injury Parkinson’s Disease Hydrocephalus, tumor, stroke, neurodegenerative d/o Binswanger’s disease Muscular dystrophy, spi9nal muscular atrophy, acquired proximal myopathy Vitamin B12 deficiency Tabes dorsalis URINARY AND SEXUAL DYSFUNCTION URINARY Anatomy/Physiology of Continence Circuit Circuit 1 Circuit 2 (spino-bulbarspinal) Circuit 3 Connections Dorsomedial frontal lobe to M region (pons) Reflex arc starting in bladder projecting to M region (pons) w/ outflow connections to PNS sacral spinal motor nuclei Spinal segmental reflex arc w/ afferents from detrusor muscle to pudendal nucleus and efferent fibers to striated sphincter muscles Function Volitional control of micturition Pontine micturition center o Areas M region stimulation decrease in urethral pressure, then rise in detrusor muscle pressure and voiding; M region projects to sacral cord IML L region (same level) stimulation contraction of urethral sphincter (storage) o Damage loss of inhibitory control over spinal reflexes (circuit 3) and as bladder distends, micturition reflex is automatically activated w/o pt’s awareness or control, and detrusor hyperreflexia and incontinence occurs Muscles of micturition o Detrusor (smooth): PNS causes contraction; during filling it is inhibited, during micturition it is stimulated o Internal urethral sphincter (smooth): SNS causes contraction; stim during filling, inh during micturition o External urethral sphincter (skeletal): Somatic motor causes contraction; stim during filling, inh during mic Evaluation of Incontinence Urodynamic studies PVR (postvoid residual): normal<50mL; if increased implies poor bladder emptying (sphincter dyssynergia, atonic bladder are common neurogenic causes) Cystometry: gives info re bladder compliance, capacity, volume at 1 st sensation and at urge to void; voiding pressure; presence of uninhibited detrusor contractions Cystourethroscopy: assesses integrity of lower urinary system, and IDs important urethral and bladder lesions Retrograde urethrography Neurophysiologic studies: sphincter and pelvic floor EMG Type of neurogenic bladder Spastic bladder Capacity Compliance Other Indicates… Decreased Reduced Uninhibited detrusor contractions Atonic bladder Increased Increased Low voiding pressure and flow rate UMN problem d/t frontal lobe, pontine, or suprasacral spinal cord lesion LMN problem d/t lesion at level of conus medullaris, cauda equina, or sacral plexus, or peripheral nerve dysfunction Type of incontinence Urge Description Etiology Involuntary loss of urine a/w strong desire to void (urgency) Detrusor instability (DI) Detrusor hyperreflexia (if DI d/t neurologic problem) Stress Involuntary loss of urine during coughing, sneezing, laughing, or activities that increase intraabdominal pressure Urge + stress Involuntary loss of urine a/w overdistension of bladder; constant dribbling Weak pelvic floor muscles Mixed Overflow Underactive or acontractile detrusor (drugs, diabetic neuropathy, lower spinal cord injury, or radical pelvic surgery that interrups innervation of detrusor) Clinical expression Spastic bladder Patient population Strokes, suprasacral spinal cord lesions, MS Associated si/sx Detrusor-sphincter dyssynergia (DSD): inappropriate contraction of external sphincter w/ detrusor contraction urinary retention, vesicourethral reflux, and renal damage Multiparous women Atonic bladder Incontinence in the Neurologic Patient Stroke and spinal cord disease usually produce an UMN bladder or spastic bladder w/ or w/o sphincter dyssynergia o Supraspinal dz Stroke Parkinson’s (40-70%) o Spinal cord dz Spinal cord injury Multiple sclerosis (75%) Small-fiber neuropathies can produce a neurogenic atonic bladder w/ high PVR (risk to upper urinary tract), e.g. as in diabetic neuropathy Treatment of Urinary Incontinence Goals Preservation of upper urinary tract fxn Improvement of pt’s urinary symptoms that impair quality of life Treatments Disorder Urge incontinence (spastic bladder) Stress incontinence Atonic bladder w/ overflow incontinence Detrusor dyssynergia Treatments 1. Anticholinergic agents: Tolterodine (Detrol), Oxybutynin (Ditropan), Propantheline 2. TCAs: imipramine 3. Desmopressin spray/tabs (DDAVP): used to treat diabetes insipidus, but produces a significant reduction in voiding frequency 4. Intravesical capsaicin: for intractable detrusor hyperreflexia; has neurotoxic effect on afferent C fibers that drive volume-determined reflex detrusor contractions 1. Alpha-adrenergic agonist drugs: Phenylpropanolamine, Pseudoephedrine (these stimulate smooth muscle alpha-adrenergic receptors contraction) 2. Estrogen therapy: adjunctive in post-menopausal women 1. Crede’s maneuver or valsalva maneuver to empty bladder 2. Intermittent self-catheterization (mainstay of long-term tx) 3. Pharmacotherapy usually not effective; cholinergic agent bethanecol (stimulates cholinergic receptors, increasing detrusor muscle tone 1. Intermittent catheterization 2. Suprapubic catheterizaition 3. Sacral nerve stimulation ERECTILE DYSFUNCTION Persistent inability to attain or maintain penile erection sufficient for sexual intercourse 10-20 million American men affected 80% of cases are biologic or organic in origin Anatomy and Physiology Pudendal nerve: carries motor and sensory fibers that innervate the penis and clitoris PNS: o Sacral cord S2-S4, erection o Local mediators: NO, cGMP primarily released by PNS activity contributing to sustained erection SNS: cells in spinal cord levels T11-T12 through hypogastric plexus, ejaculation Management Requires recognizing etiology (neurogenic, vascular, traumatic, endocrine, psychogenic, drugs) and treating underlying cause Pharmacotherapy: o Viagra (25-100 mg/day, 30-60 min before intercourse): SE include facial flushing, HA o Intraurethral suppositories o Intracavernosal injections of alprostadil (Caverject) HEADACHE AND FACIAL PAIN Pathophysiology Caused by disturbance/irritation of pain-sensitive structures in head o W/in cranium: blood vessels, meninges, CN V, IX, X (brain parenchyma itself + bone are pain-insensitive) o Outside cranium: periosteum of skull, muscles, nerves, vessels, subcutaneous tissues, eyes, ears, sinuses, mucus membranes Pain pathway o Irritation of pain-sensitive structure nociceptive input relayed to brain via CN V or upper cervical roots CNV: dermatomal distribution on face, anterior and middle cranial fossas (thus, painful stimulation of structures in ant/mid fossas referred to eye or front or side of head) Upper cervical roots: dermatomal on posterior surface of head and neck and ears, posterior fossa (thus, painful stimulation of structures in posterior fossa referred to back of head and upper part of neck) 3 General Classes of HAs Primary (migraine, cluster, tension) not a/w underlying structural cause HA a/w serious neurologic dz (brain tumor, meningitis, aneurysm) HA/pain from structures in skull and face (eyes, sinuses, mouth) History of the Presenting HA Hx Component Onset and frequency of pain Location of pain +/- prodromal symptoms? Precipitating factors Description of pain Associated sx/neurologic signs Example Unilateral cluster, migraine Bilateral tension Scintillating scotoma prior to classic migraine Alcohol as a trigger for cluster Nitrite-containing food (hot dog/salami), tyramine-containing cheese as migraine trigger Lancinating/shooting pain in V2/V3 distribution trigeminal neuralgia (tic douloureux) Unilateral throbbing pain migraine Dull, bandlike or tightening pain tension Sharp, stabbing pain esp. behind one eye cluster N/V migraine, increased ICP d/t hydrocephalus or tumor Photophobia, phonophobia, increased frequency of HA at menstruation migraine Fever meningitis, local infection such as dental abscess Unilateral lacrimation or rhinorrhea cluster Primary Headaches Primary HA Type MaleFemale Ratio F>M Age of Onset Type of Pain Associated Si/Sx Treatment Teen years Unilateral or bilateral, pulsing or throbbing Tension F=M Any age Bilateral and occipital; pain is dull and bandlike, not throbbing N/V, photophobia, phonophobia Aura is a transient focal neuro sx preceding HA; most common type is visual (flashing lights, zigzag lines marching across visual field); develop over 5-20 min, and last 15 min1 hr; HA usually follows w/in 20-60 min and lasts 4-72 hrs Muscle spasm may be involved Cluster M>>F 3rd decade of life HAs occur in clusters in which HA recur cyclically (3-4x/day per cluster) followed by remission; each cluster lasts up to several months and remission can be mo-yrs Pain behind one eye or over lateral part of nose Prophylaxis: avoid triggers, meds (betablockers like propranolol, Ca++ channel blockers like verapamil, TCAs like amitriptyline, some anticonvulsants like depakote) Abortive: simple analgesics like acetominophen, aspirin, NSAIDS, ergot alkaloids and selective 5-HT1 agonists like sumatriptan Many of those used for migraine Also, PT, stress management, biofeedback, psychotherapy Avoid possible precipitants (e.g. EtOH, strenuous exercise) Verapamil for prophylaxis Symptomatic tx includes inhalation of pure oxygen (>90% effective); sumatriptan and dihydroergotamine can be used too Migraine (w/ aura= ”classic”) (w/o aura= ”common”) Ipsilateral conjunctival injection, lacrimation, nasal congestion, and occasional Horner’s syndrome Secondary HAs HA Type Subarachnoid Hemorrhage Etiology Nontraumatic: ruptured aneurysm, bleeding from A-V malformation Description Sudden, severe, “worst HA of my life” Associated Si/Sx LOC, vomiting, neck stiffness Diagnosis LP or CT: look for evidence of hemorrhage or heme b/d in CSF Temporal Arteritis (Giant Cell Arteritis) Subacute granulomatous inflammatory condition involving branches of external carotid artery, esp. temporal arteries Occurs in elderly, unilateral or bilateral, over temporal arteries Scalp tenderness, jaw pain during chewing (jaw claudication), involvement of ophthalmic artery can lead to blindness Elevated ESR to 100 Definitive dx made by temporal artery biopsy demonstrating vasculitis Trigeminal Neuralgia (Tic Douloureux) Microvascular compression of trigeminal nerve Idiopathic Intracranial HTN (Pseudotumor Cerebri) A/w obesity Facial pain syndrome in which brief severe electrical shocklike pains occur in distribution of a branch of CNV (2 and 3 most common); most common in middle age and elderly; can be precipitated by movement, a cold breeze, or tactile stimulation in a trigger zone Women in 2-4th decades of life Post-Lumbar Puncture or Low-Pressure HA Following LP HA in an upright position starting w/in 48 hrs of LP and resolving in several days w/o tx; HA relieved when lying down Treatment Acute control of BP for adequate brain perfusion, monitoring for vasospasm and acute obstructive hydrocephalus d/t subarachnoid blood Definitive tx: surgical resection or clipping of aneurysm Prednisone in decreasing doses for several months and then continued for next 1-2 yrs Carbamazepine Bilateral visual sxs: fleeting loss of visual acuity, scotoma, double vision, perhaps papilledema CT/MRI normal LP shows increased pressure >250 mm water Acetazolamide (CA inhibitor): inhibits CSF formation Furosemide Oral steroids Serial LP to decrease CSF pressure If tx is ineffective, pts may be left w/ permanent visual loss IV caffeine sodium benzoate Blood patch