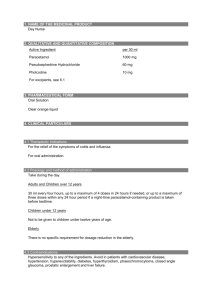
1. name of the medicinal product
advertisement

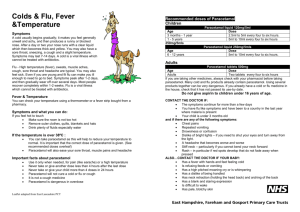
SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Quramol 500 mg effervescent tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each effervescent tablet contains 500 mg paracetamol. Excipients with known effect: Contains sodium 209.6 mg (9.12 mmol) and sorbitol (E420) 100 mg (0.55 mmol) per tablet. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Effervescent tablet. White, round tablet with diameter 23 mm. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Quramol is indicated for the short-term treatment of painful and/or febrile conditions, such as pain and fever associated with colds and flu, headache, muscle and joint pain, toothache and menstrual pain. 4.2 Posology and method of administration Posology The product is recommended for adults and adolescents aged 12 years and above. Paediatric population For children weighing 41–50 kg (age about 12 to 15 years), the dosage is 1–2 tablets at a time, to be repeated every 6 hours as required, the maximum being 6 tablets per day. Adults and adolescents For adults and adolescents weighing more than 50 kg (aged about 15 years or older) the usual single dose is 1–2 tablets at a time, to be repeated every 6 hours as required, the maximum being 8 tablets per day. Generally, it is not necessary to exceed the dose of 3 g paracetamol per day (6 tablets per day). However, in more severe pain, the maximum dosage may be increased up to 4 g per day (8 tablets per day). Doses should never be taken more frequently than every 4 hours. Special groups of patients Impaired liver function: In patients with impaired hepatic function or Gilbert’s syndrome, the dose must be reduced or the dosing interval prolonged. Impaired kidney function: In patients with renal insufficiency, the dose should be reduced: Glomerular filtration rate Dose 10–50 ml/min 500 mg every 6 hours < 10 ml/min 500 mg every 8 hours Elderly patients: Dose adjustment is not required in the elderly. Method of administration Oral use. Allow the tablet to dissolve completely in a glass (1.5–2 desilitres) of water. 4.3 Contraindications Hypersensitivity to the active substance or to any of the excipients listed in section 6.1. Severe hepatic insufficiency. 4.4 Special warnings and precautions for use Caution is advised in the administration of paracetamol to patients with moderate and severe renal insufficiency, mild to moderate hepatocellular insufficiency (including Gilbert’s syndrome), severe hepatic insufficiency (Child-Pugh > 9), acute hepatitis, concomitant treatment with medicinal products affecting hepatic functions, glucose-6-phosphatedehydrogenase deficiency, haemolytic anaemia, dehydration, alcohol abuse and chronic malnutrition. Patients should be advised not to take any other paracetamol-containing products concurrently due to the risk of severe liver damage in case of overdose (see section 4.9). If the pain persists for more than 5 days or the fever lasts for more than 3 days or gets worse a physician should be consulted. Alcoholic beverages should be avoided while taking this product because concomitant use of paracetamol may cause liver damage. Paracetamol should be given with caution to patients with alcohol dependence. In case of overdose, concomitant use of barbiturates, alcohol or other agents with hepatotoxic effect will increase the risk of liver damage. In general, habitual intake of analgesics, particularly a combination of several analgesic substances, can lead to permanent renal damage with the risk of renal failure (analgesic nephropathy). There is a possible risk of metabolic acidosis associated with paracetamol overdose in patients with additional risk factors, such as malnutrition, or sepsis-like inflammatory response. This medicinal product contains sodium (209.6 mg per tablet). To be taken into consideration by patients on a controlled sodium diet. This medicinal product contains sorbitol (100 mg per tablet). Patients with rare hereditary problems of fructose intolerance should not take this medicine. 4.5 Interaction with other medicinal products and other forms of interaction Probenecid inhibits the binding of paracetamol to glucuronic acid, thus leading to a reduction in paracetamol clearance by a factor of approximately 2. In patients concurrently taking probenecid, the paracetamol dose should be reduced. Enzyme-inducing drugs such as certain antiepileptics (phenytoin, phenobarbital, carbamazepine) decreased plasma AUC of paracetamol to approximately 60% in pharmacokinetic studies. Other substances with enzyme-inducing properties (i.e. rifampicin, Hypericum) could also result in decreased concentrations of paracetamol. In addition, the risk of liver damage during treatment with the maximum recommended dose of paracetamol is probably higher in patients who receive enzymeinducing drugs. Zidovudine may affect paracetamol metabolism and vice versa, which may add to the toxicity of both. Repeated paracetamol intake for longer than one week enhances the effects of anticoagulants, particularly warfarin. Therefore long-term administration of paracetamol in patients who are being treated with anticoagulants should only take place under medicinal supervision. The effect may occur already at daily doses of 1.5–2 g for 5–7 days. If paracetamol is used in doses at > 2 g daily, INR values (International Normalized Ratio) should be monitored. Occasional paracetamol intake has no significant effects on bleeding tendency. Concurrent intake of medicinal products that accelerate gastric emptying, such as metoclopramide or domperidone, accelerates the absorption and onset of effect of paracetamol. Cholestyramine may reduce the absorption of paracetamol and should therefore not be administered within an hour following paracetamol administration. Isoniazid may affect the pharmacokinetics of paracetamol with possible potentiation of liver toxicity. Concurrent intake of medicines that slow gastric emptying can delay the absorption and onset of effect of paracetamol. Paracetamol may affect the pharmacokinetics of chloramphenicol. Monitoring of chloramphenicol plasma levels is recommended if combining paracetamol with chloramphenicol injection treatment. Ethyl alcohol potentiates paracetamol toxicity, possibly by inducing hepatic production of paracetamol-derived hepatotoxic products. Effects on laboratory tests Intake of paracetamol can affect tests for uric acid using phosphotungstic acid and blood sugar tests using glucose-oxidase-peroxidase. 4.6 Fertility, pregnancy and lactation Pregnancy Epidemiological studies concerning the use of oral therapeutic doses of paracetamol have shown no adverse effects on human pregnancy or on the foetus or newborn. Paracetamol may be used at therapeutic doses during pregnancy after consideration has been given to the benefit versus risk ratio. During pregnancy, paracetamol should not be taken for a long period, at high doses or in combination with other medicinal products, as safety of use has not been established in such cases. Breastfeeding Low levels of paracetamol are excreted in human milk. No undesirable effects on breastfed infants have been reported. Paracetamol can be used during breast-feeding as long as the recommended dosage is not exceeded. In case of long-term use, caution should be exercised. Fertility There are no concerns about effects on fertility due to paracetamol treatment. 4.7 Effects on ability to drive and use machines Quramol has no or negligible influence on the ability to drive and use machines. 4.8 Undesirable effects Adverse effects are rare at common therapeutic doses. Liver damage has rarely been described when paracetamol has been used at therapeutic doses, but in patients with a history of liver damage or using paracetamol combined with some other agent damaging the liver (such as alcohol) the risk of liver damage must be taken into consideration. Adverse reactions are listed below by system organ class and frequency. Frequencies are defined as: very common (≥ 1/10); common (≥ 1/100 to < 1/10); uncommon (≥ 1/1,000 to < 1/100); rare (≥ 1/10,000 to < 1/1,000); very rare (< 1/10,000); not known (cannot be estimated from the available data). Frequency Rare (≥ 1/10,000 to < 1/1,000) System Blood and lymphatic system disorders Immune system disorders Psychiatric disorders Nervous system disorders Eye disorders Gastrointestinal disorders Hepatobiliary disorders Very Rare (< 10,000) Not known Skin and subcutaneous tissue disorders General disorders and administration site conditions Immune system disorders Metabolism and nutrition disorders Respiratory, thoracic and mediastinal disorders Hepatobiliary disorders Renal and urinary disorders General disorders and administration site conditions Skin and subcutaneous tissue disorders Symptoms Platelet disorders, stem cell disorders, agranulocytosis, leukopenia, thrombocytopenia, haemolytic anaemia, pancytopenia Allergies (excluding angioedema) Depression NOS, confusion, hallucinations Tremor NOS, headache NOS Abnormal vision Haemorrhage NOS, abdominal pain NOS, diarrhoea NOS, nausea, vomiting Abnormal hepatic function, hepatic failure, hepatic necrosis, jaundice Pruritus, rash, angioedema, urticaria, sweating, purpura Oedema, hyperthermia Anaphylactic shock, hypersensitivity reaction (requiring discontinuation of treatment) Hypoglycaemia Bronchospasm Hepatotoxicity Sterile pyuria (cloudy urine) and renal side effects Dizziness (excluding vertigo), malaise, sedation, drug interaction NOS Stevens-Johnson syndrome, toxic epidermal necrolysis Interstitial nephritis has been reported incidentally after prolonged use of high doses. Some cases of erythema multiforme, oedema of the larynx, anaemia, liver alteration and hepatitis, renal alteration (severe renal impairment, haematuria, anuresis) and vertigo have been reported. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system listed in Appendix V*. 4.9 Overdose Symptoms At particular risk of intoxication are elderly patients, young children, persons with hepatic disease, chronic alcohol abuse, chronic malnutrition and those concurrently taking medicinal products that lead to enzyme induction. In such cases, overdose can be fatal. In an acute overdose, paracetamol may exert a hepatotoxic effect or even cause necrosis of the liver. Overdose of paracetamol, including high total dose levels reached over a prolonged period, may cause analgesic induced nephropathy with irreversible liver failure. Patients should be warned not to take other products containing paracetamol concurrently. Interstitial nephritis has been reported incidentally after prolonged use of high doses. Some cases of epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, oedema of the larynx, anaphylactic shock, anaemia, liver alteration and hepatitis, renal alteration (severe renal impairment, haematuria, anuresis), gastrointestinal effects and vertigo have been reported. Symptoms of paracetamol overdose in the first 24 hours are pallor, nausea, vomiting, and anorexia. Abdominal pain may be the first indication of liver damage, which is not usually apparent for 24 to 48 hours. Sometimes clinical symptoms of liver damage may be delayed for up to 4 to 6 days after ingestion. Liver damage is generally at a maximum 72 to 96 hours after ingestion. Abnormalities of glucose metabolism and metabolic acidosis may occur. Acute renal failure with acute tubular necrosis may develop even in the absence of severe liver damage. Other non-hepatic symptoms, such as myocardial anomalies and pancreatitis, may occur following paracetamol overdose. Management of overdose Treatment of overdose should be started as soon as possible after intake (preferably within 10– 12 hours) in order to prevent/diminish liver damage. Early administration of N-acetylcysteine i.v. or per os as an antidote to paracetamol, possibly gastric lavage and/or administration of oral methionine (if vomiting is not a problem), may have beneficial effect up to at least 48 hours after the overdose. The mode of administration of N-acetylcysteine should be considered individually taking into account the consciousness of the patient and his/her tendency to vomit. Treatment should be started as soon as possible but it will be useful even if started as late as 36 hours after intake. Plasma paracetamol concentration should be measured at 4 hours or later after ingestion. Administration of activated charcoal and monitoring of breathing and circulation may be useful. If an oral antidote is given, it should be noted that medicinal charcoal also adsorbs the antidote. In cases of convulsions, diazepam may be administered. For more accurate instructions for treatment of paracetamol intoxication national poison information service should always be consulted. 5. PHARMACOLOGICAL PROPERTIES 5.1 Pharmacodynamic properties Pharmacotherapeutic group: other analgesic and antipyretics; anilides, ATC code: N02BE01. Paracetamol has analgesic and antipyretic properties. It is used for the relief of mild to moderate pain and for fever. The primary mechanism of action may be the inhibition of prostaglandins synthesis. Paracetamol produces peripheral vasodilatation yielding increased blood flow through the skin, perspiration and heat loss. The analgesic effect starts within 30 minutes, with maximum effect within 1 to 2 hours and lasts up to 4 to 5 hours. The antipyretic effect starts within 30 to 60 minutes. The maximum antipyretic effect is between 2 to 3 hours and the effect lasts up to 8 hours. Unlike acetyl salicylic acid, paracetamol does not cause gastrointestinal irritation and is well tolerated by patients. Thrombocyte aggregation and bleeding time are generally not affected by paracetamol. Patients with hypersensitivity to acetyl salicylic acid generally tolerate paracetamol. 5.2 Pharmacokinetic properties Absorption Paracetamol is rapidly and almost completely absorbed from the gastrointestinal tract with a bioavailability of 80–88%. Peak plasma concentration occurs after 30 to 60 minutes. Distribution Paracetamol is distributed rapidly into all tissues. Blood, plasma and saliva concentrations are comparable. Protein binding is low with recommended doses. Biotransformation Most of the paracetamol dose is metabolized in the liver to nontoxic sulphate and glucuronide conjugates. A small part of the dose is metabolized to a reactive, potentially toxic intermediate product that binds to liver glutathione and forms nontoxic cysteine and mercaptopurine derivatives excreted via the kidneys. At therapeutic doses sulphate/glucuronide reactions are not saturated but high overdoses (of 140 mg/kg or more) saturate these reactions. In such cases, the amount of reactive intermediate product may deplete liver glutathione reserves, and the toxic metabolite will bind to liver cell proteins causing liver cell necrosis. Elimination Elimination is mainly in the urine. 90% of the absorbed amount is renally excreted within 24 hours, mainly as glucuronides (60–80%) and sulphate conjugates (20–30%). Less than 5% is eliminated in unchanged form. The elimination half-life of paracetamol after oral and i.v. administration is 1.5– 3 hours in adults. Renal insufficiency In patients with severe renal insufficiency (creatinine clearance < 10 ml/min), elimination of paracetamol and its metabolites is delayed. Elderly patients Conjugation is unchanged in this patient group. Paediatric population In neonates and children < 12 years sulphate conjugation is the main elimination route and glucuronidation is lower than in adults. Total elimination in children is comparable to that in adults, due to an increased capacity for sulphate conjugation. In children the formation of the toxic intermediate product is reduced compared with adults. Additionally, neonates have an increased ability to replete liver glutathione. Therefore, severe liver damage caused by paracetamol would seem to be rarer in children than in adults. The elimination half-life of paracetamol is 2–2.5 hours in children. 5.3 Preclinical safety data Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity, carcinogenic potential or toxicity to reproduction. Overdose may lead to serious hepatotoxicity. 6. PHARMACEUTICAL PARTICULARS 6.1 List of excipients Anhydrous citric acid Sodium hydrogen carbonate Anhydrous sodium carbonate Sorbitol (E420) Saccharin sodium Macrogol Povidone 6.2 Incompatibilities Not applicable. 6.3 Shelf life 3 years. 6.4 Special precautions for storage Store in the original package in order to protect from moisture. 6.5 Nature and contents of container A round polypropylene tube closed with a polyethylene stopper containing a desiccant cartridge. Pack size: 16 tablets. Aluminium/polyethylene blister strip. Pack sizes: 8, 12, 16, 20 and 100 tablets. Not all pack sizes may be marketed. 6.6 Special precautions for disposal and other handling No special requirements. 7. MARKETING AUTHORISATION HOLDER Orion Corporation Orionintie 1 FI-02200 Espoo Finland 8. MARKETING AUTHORISATION NUMBER(S) [To be completed nationally] 9. DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION Date of first authorisation: 20.6.2012 10. DATE OF REVISION OF THE TEXT 16 April 2015