Administrative Office St. Joseph`s Hospital Site, L301
advertisement

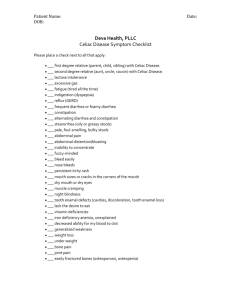
Administrative Office St. Joseph's Hospital Site, L301-10 50 Charlton Avenue East HAMILTON, Ontario, CANADA L8N 4A6 PHONE: (905) 521-6141 FAX: (905) 521-6142 http://www.fhs.mcmaster.ca/hrlmp/ Issue No. 42 QUARTERLY NEWSLETTER Spring, 1996 THE SEROLOGIC DIAGNOSIS OF CELIAC DISEASE: ANTIGLIADIN, ANTIRETICULIN AND ANTIENDOMYSIAL ANTIBODIES Clinical Features 1 The prevalence of Celiac disease (otherwise known as "Celiac sprue", "non-tropical sprue" or "glutensensitive enteropathy") is in the order of 1 in 1000 although this is probably an underestimate since a number of affected individuals are asymptomatic. The incidence is highest in children aged 1-3 and presents classically as diarrhea, growth retardation and anemia. Adolescents can present with delayed puberty and in adults, anemia without other GI symptoms can be a prominent feature. Cause and Pathogenesis 2 Small intestinal mucosal damage is caused by the fraction of wheat gluten containing gliadin polypeptides. The mechanism by which this toxic reaction occurs in susceptible individuals is not known, but there is strong evidence for an immune component. Thus the sera of affected individuals can contain antibodies against gliadin and mucosal components which are usually not found in significant titers in normal individuals, and these antibodies have proven to be useful for both the diagnosis and monitoring of celiac disease. They are antigliadin (AGA) IgA and IgG, antireticulin (ARA) IgA and antiendomysial (EMA) IgA. Diagnosis The European Society of Pediatric Gastroenterology and Nutrition (ESPGAN) acknowledges the diagnostic usefulness of "celiac antibodies" but states that a small intestinal biopsy is still needed to establish a positive diagnosis.3 The following table includes data from several recent studies. Sensitivity, Specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of the four antibodies in the diagnosis of celiac disease Sensitivity (%) Specificity (%) PPV (%) NPV (%) AGA IgG4 88 92 88 92 AGA IgA4 52 94 94 74 AGA IgG & 1gA5, 6 96-100 96-97 - - EMA IgA (age > 2)4 97 98 97 98 53-65 100 100 7177 99.6 99.3 99.3 99.6 ARA IgA4 AGA IgG, IgA, & EMA IgA7 The IgG antigliadin antibody (AGA IgG) and the IgA antiendomysial antibody (EMA IgA) have both high sensitivities and negative predictive values. AGA IgG, however, is found in normal individuals, individuals with various autoimmune disorders, cow's milk protein intolerance, acute infectious diarrhea, chronic intractable diarrhea, parasitosis, primary biliary cirrhosis and hepatitis C. 1 All three IgA species, AGA, ARA and EMA have high specificities and positive predictive values, however they can be negative in patients with selective IgA deficiency which is associated with celiac disease. Some clinicians recommend screening with all four antibodies to achieve the highest sensitivity and specificity. Who to Test Anyone with a clinical picture suspicious for celiac disease should have serologic screening. Positive IgA antibodies will usually return to normal within three months of the initiation of a gluten-free diet making them useful for monitoring compliance and efficacy of treatment.2 Anyone with a positive AGA IgG but negative IgA antibodies should be screened for selective IgA deficiency. Some authorities believe that first degree relatives of patients with celiac disease should be screened serologically, because of the high prevalence of asymptomatic celiac disease and the risk of GI lymphoma in untreated celiac patients. 1 As of yet there is no strong evidence to support this practice.8 Sample Required and Turnaround Time There is no patient preparation required. A minimum of 5 mL of whole blood should be collected in a redtopped tube and forwarded to the Clinical Immunology Laboratory at Chedoke-McMaster with a request for "Celiac Antibody Profile". Samples will be processed on a biweekly basis. Results will be reported as positive, negative or borderline and a written interpretation will be provided. When positive, a concentration will be given and a titre will also be provided for the EMA IgA. For more information contact: B. Roberge, Diagnostic Unit Manager, Regional Immunology Laboratory, Room 2N49, (905) 521-2100 Ext. 76267, Chedoke-McMaster Hospitals. Prepared by J. Cochrane, M.D. Resident in Medical Biochemistry Department of Pathology McMaster University References 1. Misra S, Ament ME: Diagnosis of coeliac sprue in 1994. Gastroenterol Clin of North Am 24(1):133-43, 1995 2. Trier JS: Celiac Sprue. New Engl J Med 325(24): 1709-19, 1991 3 Walker-Smith JA, Guandalini S, Schmitz J, Shmerling DH, Visakorpi JK: Revised criteria for diagnosis of coeliac disease. Report of Working Group of European Society of Pediatric Gastroenterology and Nutrition. Arch Dis Child 65: 909-91 1; 1990 4 . Lemer A, Kumar V, lancu TC: Immunological diagnosis of childhood coeliac disease: Comparison between antigliadin, antireticulin and antiendomysial antibodies. Clin Exp Immunol 95:78-82; 1994 5 Goncri J, Skerritt IH, Mitchell ID: A reliable screening test for coeliac disease: enzyme-linked immunosorbent assay to detect anti-gliadin antibodies in serum. Aust NZ J Med 21: 723-31, 1991 6. Burgin-Wolff A, Berger R, Gaze H, Huber H, Lentze MJ, Nussle D: IgG, IgA and IgE gliadin antibody determinations as screening test for untreated coeliac disease in children, a multicentre study. fur ] Pediatr 148:496-502, 1989 7. Burgin-WolB Gaze H, Hadziselimovic F, Huber H, Lentze MJ, Nussle D, Reymond-Denhet C: Antigliadin and antiendomysium antibody for coeliac disease Arch Dis Child 66:941-47. 1991 8. Howdle PD (ed): Coeliac Disease, Bllliere's Clin Gatroenterol 9(2), 1995 We are looking forward to providing further improvements in service, and welcome comments and enquiries. Feel free to phone us at 521-5084, or 521-2100, extension 3710. ********************* The Hamilton Health Sciences Laboratory Program is a collaborative program of Hamilton Civic, St. Joseph's and Chedoke-McMaster Hospitals, which operate Community Laboratory Services as a service to Hamilton Physicians and their patients. For further information concerning the Laboratory Program call Mr. A.J. Bailey at 572-7575 and for Community Laboratory Services telephone Mrs. K. Williams at 521-6052. COMMUNITY LABORATORY SERVICES Collection Centres Ancaster Centre 226 Wilson Street E. Ancaster, Ontario Tel: (905) 648-4080 Charlton Centre 25 Charlton Ave. E. Hamilton, Ontario Tel: (905) 521-6052 George St. Centre 196 George St. Hamilton, Ontario Tel: (905) 525-1562 Carlisle Centre 1493 Centre Rd. Carlisle, Ontario Tel: (905) 689-0818 Dundas Centre 16 Cross St. Dundas, Ont. Tel: (905) 627-3814 or (905) 627-7190 Concession Centre 688 Concession St. Hamilton, Ontario Tel: (905) 383-2021 First Place Centre 350 King St. E., Ste. 103 Hamilton, Ontario Tel: (905) 522-8765/66 North Hamilton Centre 554 John St. North Hamilton, Ontario Tel: (905) 522-4197 Stoney Creek Centre 2757 King Street E. Hamilton, Ontario Tel: (905) 573-4824 Fennell Centre 836 Fennell Street E Hamilton, Ontario Tel: (905) 383-0505 or (905) 383-9953 East Hamilton Centre 1463 Main St. East Hamilton, Ontario Tel: (905) 549-5004 For Housecalls throughout the region, telephone Mrs. K. Williams at (905) 5216052 For Laboratory Reference Centre Services phone Mrs. B. Baltzer at (905) 521-6065 or fax requests for information to (905) 528-1464