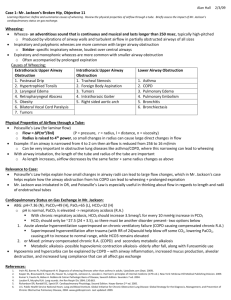
Asthma (outline only)
advertisement
ASTHMA Pathophysiology & Interventions for Respiratory Care Practitioners Myths • It’s all in your head. • While stress may play some role in onset of symptoms like wheezing, it is a chronic inflammatory airway disease • A poor mother-child relationship. • Another attempt to explain the condition psycho-socially. Myths • Asthma doesn’t kill anymore. • Accounts for 5,000 deaths per year • Asthma isn’t serious anymore. – Affects 14-15 million people in the U.S. – Probably most under-diagnosed condition. – Hospitalization and death rates highest for blacks, children, and poorer individuals. Myths • Asthma doesn’t require medical treatment. – About 470,000 hospitalizations each year. – About 100 million days of restricted activity annually, sick days, etc. • Children outgrow asthma. – Most common chronic disease of childhood. – Asthma is more common in children and young adults, but is present at all ages. Myths • Move to Arizona. • Buy a pet Chihuahua. – Allergens and triggers myth. – New allergens in different environments. – accounts for 8.8% of the Hawaii population • There is a cure for asthma. – Not yet. – Requires compliance of patient and the health care team. – New medications – New research into inflammatory process. Asthma and Urban Environment • • • • • Aeropollutants Beta-agonist bronchodilators Poverty Race and ethnicity Illicit drug use • • • • Psychosocial and family dysfunction Restricted access to health care Crowding Indoor allergens and pollutants Key Points - Changing Views • Historically, considered a disease of airway smooth muscle • Characterized by intermittent bronchospams due to variety of specific and nonspecific stimuli • Episodic bronchospasm associated with coughing, wheezing, tightness of chest, difficulty breathing. • Symptoms wax and wane, lasting couple of days to couple of weeks Perspective Change • Treat the disease, not the patient (vs. treat the patient, not the disease) • Too much focus on symptoms, but focus on the disease, inflammation, came from examining lungs of patients who died from asthma. • Saw cellular changes in airway Changes. . . • Structural changes of bronchi – Epithelium changes – Basement membrane changes – Smooth muscle growth – Goblet cell proliferation – Presence of eosinophils, mast cells, etc., in both atopic and nonatopic persons with asthma and even in people with mild disease Current Understanding • Airway inflammation • Many different cells and cellular elements involved, e.g., mast cells, eosinophils, T-lynmphocytes, macrophages, neutrophis, and epithelial cells • Inflammation causes recurrent episodes of wheezing, chest tightness, coughing. • Airflow obstruction, often reversible with treatment • Subset of COPD, but reversibility is key Inflammation - Bi-phasic • Working definition of asthma (1995, NHLBI) – Asthma is a chronic inflammatory disorder of the airways in which many cells & cellular elements play a role (mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, & epithelial cells). – In susceptible individuals , inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night/early morning. These episodes are associated with variable airflow obstruction often reversible spontaneously/treatment Inflammation • Bi-phasic, early and late phase • Inflammation causes increase in existing bronchial responsiveness to variety of stimulants, i.e., hyperresponsiveness • Episodic “attack” is an acute event, early phase, lung function can return to normal • Recurrent “attacks” are essentially the continuation of the early phase—but now second, or late phase response—chronic inflammation • This inflammation modifies the biology of the airway to cause bronchial hyperresponsiveness General Aspects of Inflammation • Redness – Due to dilatation of small blood vessels in damaged area • Heat – Due to increase blood flow through region • Swelling – From edema, accumulation of fluid in extra vascular spaces Pain stretching and distortion of tissues due to edema Early Phase • Inhalation of allergen or some trigger • Immediate, 5-30 minutes, signs of inflammation. • Due to release of chemical mediators from mast cells Exocytosis of Mast Cell Histamine Release Early Phase • Signs – – – – – Smooth muscle contractions—leading to bronchospasm (wheezing) Mucus secretion Cough Edema of the airway and further narrowing of bronchial tree Resolves within 1 hour, with or without therapeutic intervention Inflammation - Bi-phasic Arachidonic Acid Pathways Arachidonic Acid • A fatty acid produced from the membrane of mast cells • Helps to synthesize: – Cyclooxygenase pathway which produced prostaglandins (PG) – Lipoxygenase pathway which produced leukotrienes (LT) PG and LT All of the chemical reactions, chemical mediators used to be referred to as SRS-A, slow release substances of anaphylaxis Now known as either PG, LT • Prostaglandins are potent muscle constrictors • Leukotrienes are potent muscle constrictors • Both are mediating agents/chemicals of the inflammatory process. LT and PG Pathways Late Phase State Late Phase Features • 6-10 hours later, and then may continue for indefinite period of time (months) • Attraction and accumulation of inflammatory cells-all types of WBC – From degranulation of original mast cell chemical mediators – These are cytokines and chemotactic cytokines-(chemokines) proteins that attract WBCs Late Phase Features • Eosinophils and T lymphocytes (T cells) • Eosinophils migrate from blood to airway; and release more inflammatory mediators like leukotrienes. • T cells (Th2) produce Interleukins (IL) another chemical mediator (activates more T cells) Late Phase Signs • • • • • • Bronchospasm Further inflammation Airway edema Mucus production (hyperproduction) Obstructive airflows Increase airway hyper-responsiveness Signs of the Late Phase • Airway hyper-responsiveness to various stimuli—cold air, sneezing, fumes, stress (?) • This is smooth muscle dysfunction – “twitchy” airways, narrow too easily and too much • Loss of airway elasticity Inflammatory Pathway Airway Inflammation • Increase thickening of airway wall due to edema • Increased numbers of eosinophils, neutrophils, epithelial cells • Airway lumen filled with mucus from enlarged goblet cells Why a problem for some patients? • Key points – Chronic inflammatory disorder of the airways – Histopathologic features • • • • denudation of airway epithelium collagen deposition beneath basement membrane edema mast cell activation – Immune system features • inflammatory cell infiltration – Neutrophils (sudden, fatal asthma) – Eosinophils – Lymphocytes • Airway inflammation (AI) contributes to hyperresponsiveness, airflow limitation, symptoms & chronicity • AI causes types of airflow limitation: – Bronchoconstriction, edema, mucus plug formation, airway wall remodeling • Atopy is strongest predisposing factor for developing asthma – Atopy is the inherited propensity to produce abnormal amounts of IgE against common environment antigen Airway Inflammation & Lung Function May Vary • The cells that influence &/or regulate inflammation results in different types of AI: – Acute - early recruitment of cells – Subacute - cells activated to cause more persistent inflammatory pattern – Chronic - persistent level of cell damage & repair. Abnormal changes may be permanent Obstructive Defect • Airflow limitation – Acute bronchoconstriction • IgE -dependent mediator release from mast cell (leukotrienes, histamine, tryptase, prostaglandins) • aspirin /NSAID • non-IgE response (cold air, exercise, irritants) Chronic Airflow Limitation • Airflow limitation – Chronic mucus plug formation • secretions & inspissated plugs • persistent airflow limitation in severe intractable asthma – Airway remodeling • irreversible component of airflow limitation secondary to structural airway matrix changes • Airflow limitation – Airway remodeling • attributed to chronic, severe airway inflammation • early intervention with anti-inflammatory therapy suggests prevention of permanent airflow limitation Chronic Inflammation • Asthma is a reversible airway disease • However, chronic inflammation may result in irreversible airflow limitations AND • Airway remodeling - an altered pulmonary tree – – – – Smooth muscle over-development New vessels formation Goblet cells proliferation Thickening of basement membrane Chronic Inflammation • • • • Inflammation is in peripheral airways primarily But may affect central airways and even the alveoli Inflammatory cells seem to have a prolonged life in asthma Irreversible airflow may develop in some patients Presentation Complaining of. . . • “S” (subjective symptoms) – – – – – – Cough, esp. late at night Recurrent wheezing Recurrent shortness of breath Recurrent chest tightness Occurs at night, early morning Symptoms occur or worse with irritants PE • • • • • • Chest-wheezing on exhalation, sometimes on inhalation crackles I:E ratio-prolonged expiratory phase Increased AP diameter, especially during exacerbation Unable to complete full sentences Use of inspiratory accessory muscles PE • • • • Cough Sputum-clear,stringy, translucent Sternal retractions, intercostal retractions Dehydrated – – – – Increased meteabolism Increased insensible water loss Decreased fluid intake vomiting PE • Increased respiratory rate • Increased pulse rate • Increased blood pressure – All signs of hypoxemia PE • Pulsus paradoxus – >10 mmHg fall in systolic blood pressure on inspiration. 15-20 mmHg drop is severe – Mechanism: increased intrapleural pressures (thorax) promoting increased venous return & increased RV filling, decreased LV filling on contraction • If frequent ER visitor: – Has inhaled medications – Has no primary physician – No other inhaled medications, e.g., inhaled steroids, anti-inflammatory medications Diagnostic Exams • Pulse oximetry • Arterial blood gas analysis – Alkalemia, hypoxemia, hypocapnea • Calculate PA02, P(A-a)02, and Pa02/Fi02 • Bedside spirometry – Peak flow rates decreased • Chest film – Hyperinflation, hyperlucent, flat diaphragms, large AP diameter Pa02 and Relative Shunt • Hyperinflation or air trapping • Causes changes in V/Q, ie. mismatch • A decreased V to Q ratio, leading to: – Drop in PA02 and subsequent drop in Pa02 • As air trapping increases, lungs are less compliant • FRC increases • More (negative) intrapleural pressures needed to change AP diameter of chest cage Compliance and RR • • • • • • • As lung compliance decreases, ventilatory rate increases This increases patient’s minute ventilation (VE) PaC02 drops (<40mmHG) pH increases (alkalemia) This is a good sign. The patient is still attempting to ventilate. Danger signs—when the RR decreases; PaC02 begins to look normal (toward 40 mmHG)