UB-PandP - Counseling Center Village
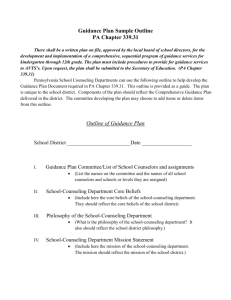
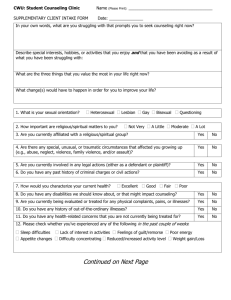
advertisement

1 UNIVERSITY AT BUFFALO COUNSELING SERVICES POLICY & PROCEDURE MANUAL 2010 2 COUNSELING SERVICES PHILOSOPHY & MISSION STATEMENT .............................................. 5 GOALS ........................................................................................................................................................... 5 STUDENT WELLNESS TEAM.................................................................................................................... 5 MISSION STATEMENT ..................................................................................................................................... 5 VISION STATEMENT ....................................................................................................................................... 5 EQUAL OPPORTUNITY .................................................................................................................................... 6 COUNSELING POLICIES AND PROCEDURES ..................................................................................... 6 ELIGIBILITY FOR SERVICES ............................................................................................................................ 6 LIMITATIONS OF SERVICES............................................................................................................................. 7 INITIAL ASSESSMENT PROCEDURES ............................................................................................................... 8 REFERRAL GUIDELINES AND PROCEDURES .................................................................................................. 10 WAIT LIST POLICY ....................................................................................................................................... 11 GROUP THERAPY POLICIES AND PROCEDURES ............................................................................................. 12 COUPLES COUNSELING ................................................................................................................................ 13 PSYCHIATRIC SERVICES AND PROCEDURES.................................................................................................. 13 CRISIS INTERVENTION .................................................................................................................................. 15 UBCS Philosophy on Crisis Intervention ............................................................................................... 15 1) Goals of Crisis Intervention ............................................................................................................ 16 2) What Crisis Intervention is NOT..................................................................................................... 16 3) Crisis Situations .............................................................................................................................. 16 4) Recommendations for Crisis Intervention ...................................................................................... 16 5) Procedure ........................................................................................................................................ 17 6) Guidelines for Interventions (See Appendix L - Guidelines for Assessing Suicidality) .................. 17 8) Duty to Warn ................................................................................................................................... 18 9) Counselor-on-Call .......................................................................................................................... 18 10) Responding to the Death of a Campus Member ......................................................................... 19 CRISIS HOURS .............................................................................................................................................. 19 MANDATED ASSESSMENTS .......................................................................................................................... 20 USE OF ASSESSMENT INSTRUMENTS ............................................................................................................ 21 MANDATED REPORTING............................................................................................................................... 21 MULTILINGUAL COUNSELORS AS TRANSLATORS ......................................................................................... 22 PAPERWORK GUIDELINES ............................................................................................................................ 22 1) Initial Assessment............................................................................................................................ 22 2) Session Notes .................................................................................................................................. 23 3) Lethality Consultation Notes........................................................................................................... 23 4) Other Consultation Notes, Phone calls, & Email ........................................................................... 23 5) Termination/Transfer Summary ...................................................................................................... 24 6) Follow up contact with clients ........................................................................................................ 24 7) Treatment Plans .............................................................................................................................. 24 GENERAL OFFICE PROCEDURES AND POLICIES .......................................................................... 25 ETHICS ......................................................................................................................................................... 25 CONFIDENTIALITY ....................................................................................................................................... 25 MAINTAINING CLIENT FILES ........................................................................................................................ 26 TRANSFERRING CLIENT CASES ................................................................................................................... 27 NO SHOW/CANCELLATION POLICY .............................................................................................................. 27 TERMINATION OR TRANSFER SUMMARIES ................................................................................................... 28 REQUEST FOR RELEASE OF INFORMATION ................................................................................................... 28 MAILING RECORDS AND COMMUNICATIONS OF CONFIDENTIAL INFORMATION ........................................... 28 3 CLIENT REQUESTS FOR HIS/HER RECORDS .................................................................................................. 29 REQUEST FOR EXCUSE FROM CLASS ............................................................................................................ 29 REQUEST FOR LETTERS SUPPORTING A LEAVE OF ABSENCE OR COURSE WITHDRAWAL ............................. 29 CLIENT EVALUATION OF SERVICES .............................................................................................................. 29 SUPERVISION ............................................................................................................................................... 30 SENIOR STAFF PEER SUPERVISION CONSULTATION ..................................................................................... 30 PRIVATE PRACTICE GUIDELINES .................................................................................................................. 31 RESEARCH POLICY ....................................................................................................................................... 31 INTERNAL USE OF EMAIL ............................................................................................................................. 32 STAFF LIBRARY ........................................................................................................................................... 32 OUTREACH SERVICES .................................................................................................................................. 33 CONSULTATION............................................................................................................................................ 34 TRAINING PROGRAMS ............................................................................................................................ 36 LEVELS OF TRAINEES ................................................................................................................................... 36 First-Year Practicum Students ................................................................................................................ 36 Advanced Psychology Practicum Students/Externs ................................................................................ 36 Predoctoral Psychology Interns ............................................................................................................. 36 Social Work Interns................................................................................................................................. 36 REQUIREMENTS............................................................................................................................................ 36 TRAINEE ELIGIBILITY................................................................................................................................... 37 EVALUATION OF TRAINEES .......................................................................................................................... 37 COORDINATION OF TRAINING ...................................................................................................................... 37 OFFICE OPERATIONS .............................................................................................................................. 37 OFFICE HOURS ............................................................................................................................................. 37 MINIMUM WORKLOAD EXPECTATIONS ........................................................................................................ 37 STAFF MEETINGS ......................................................................................................................................... 38 STAFF SCHEDULES ....................................................................................................................................... 38 VACATION AND SICK LEAVE........................................................................................................................ 39 COMPENSATORY TIME ................................................................................................................................. 40 REQUESTS FOR “ONE TIME” SCHEDULE ADJUSTMENTS ............................................................................... 40 TIME SHEETS ............................................................................................................................................... 41 STAFF INITIAL ASSESSMENT AND WALK-IN CRISIS COVERAGE RESPONSIBILITIES ...................................... 42 STAFF GRIEVANCE PROCEDURES ................................................................................................................. 42 ADDRESSING STAFF MEMBER IMPAIRMENT ................................................................................................. 42 EXTENDED COUNSELOR ABSENCE COVERAGE ............................................................................................ 42 PROFESSIONAL DEVELOPMENT .................................................................................................................... 43 SNOW DAYS ................................................................................................................................................. 43 OFFICE EQUIPMENT ..................................................................................................................................... 43 DEALING WITH THE MEDIA .......................................................................................................................... 44 REQUESTS FOR INFORMATIONAL INTERVIEWS ............................................................................................. 44 PROFESSIONAL BEHAVIOR ........................................................................................................................... 44 Dress Code .............................................................................................................................................. 44 Appropriate Use of Email ....................................................................................................................... 44 Appropriate Use of Cell Phones ............................................................................................................. 44 FRONT DESK PROTOCOL .............................................................................................................................. 44 COMPUTER SHORTCUTS ............................................................................................................................... 45 DURESS ALARM PROCEDURES ..................................................................................................................... 45 BUILDING EVACUATION PLAN ..................................................................................................................... 47 WEB CAMS .................................................................................................................................................. 47 APPENDICES ............................................................................................................................................... 48 4 APPENDIX A: TREATMENT OF MINORS POLICY STATEMENT AND GUIDELINES ......... 49 APPENDIX B: CASE AUDIT FORM – SENIOR STAFF FORM ................................................... 50 APPENDIX C: CASE AUDIT FORM – SUPPORT STAFF ........................................................... 51 APPENDIX D: RIGHTS, PRIVACY, RESPONSIBILITIES AND CONSENT TO TREATMENT ............................................................................................................................................................. 53 APPENDIX E: GUIDELINE FOR CASE DISPOSITION AND COUNSELOR ASSIGNMENTS 54 APPENDIX F: REFERRAL FORM .................................................................................................. 55 APPENDIX G: CONSENT TO RECORD FORM ........................................................................... 56 APPENDIX H: COUPLES COUNSELING POLICY FOR NON-STUDENT PARTNERS .......... 57 APPENDIX I: PSYCHIATRIC SERVICES INFORMED CONSENT FORM ............................... 58 APPENDIX J: CPEP EVALUATION REFERRAL PROCEDURES .............................................. 59 APPENDIX K: GUIDELINES FOR SAME DAY EMERGENCY CONSULTATIONS ............... 60 APPENDIX L: GUIDELINES FOR ASSESSING SUICIDALITY ................................................. 61 APPENDIX M: NYS MENTAL HYGIENE LAW – HOSPITAL COMMITTALS ........................ 63 APPENDIX N: HEALTH INSURANCE CLAIM FORM FOR INTERNATIONAL STUDENTS TRANSPORTED VIA AMBULANCE ............................................................................................. 64 APPENDIX O: CRISIS CLIENT PROCEDURES ........................................................................... 66 APPENDIX P: REFERRAL FORM FOR MANDATED ASSESSMENTS .................................... 67 APPENDIX Q: ASSESSMENT VERIFICATION FORM ............................................................... 68 APPENDIX R: POLICY AND GUIDELINES FOR USE OF PSYCHOLOGICAL ASSESSMENTS ................................................................................................................................. 69 APPENDIX S: CONSENT TO PSYCHOLOGICAL ASSESSMENT ............................................. 71 APPENDIX T: AVAILABLE PSYCHOLOGICAL ASSESSMENT INSTRUMENTS ................. 72 APPENDIX U: MANDATED REPORTING OF CHILD ABUSE .................................................. 75 APPENDIX V: WEBSITE INFORMATION ABOUT EMAIL CONFIDENTIALITY AND ONLINE SERVICES .......................................................................................................................... 76 APPENDIX W: LIST OF COMMITTEES ....................................................................................... 79 APPENDIX X: SEXUAL ASSAULT RESPONSE GUIDELINES ................................................. 80 APPENDIX Y: UB’S SEXUAL HARRASSMENT POLICY .......................................................... 83 APPENDIX Z: UBCS ORGANIZATIONAL CHART .................................................................... 86 APPENDIX AA: DUE PROCESS PROCEDURES FOR ADDRESSING STAFF GRIEVANCES 87 APPENDIX BB: DUE PROCESS PROCEDURES FOR ADDRESSING STAFF IMPAIRMENT 88 APPENDIX CC: BUILDING EVACUATION PLAN ..................................................................... 89 APPENDIX DD: STUDENT ASSISTANT APPOINTMENT CHECKLIST ................................... 91 5 COUNSELING SERVICES PHILOSOPHY & MISSION STATEMENT Counseling Services assists students in resolving personal difficulties and in acquiring those skills, attitudes, and resources necessary to both succeed in the college environment and pursue productive and satisfying lives. Counseling Services strives to contribute to the overall educational mission of the University by facilitating the academic, emotional, social, and vocational development of students and by serving as mental health consultants to the entire campus community. Respect for diversity and a commitment to students' personal growth are guiding principles in the work we do. Goals The four major goals of Counseling Services are to: 1. Provide individual, group, and couples counseling, as well as crisis intervention to address the personal, career, and educational concerns of a diverse student population and assist students in overcoming obstacles to their educational success. 2. Provide outreach programming that enhances the well being of the campus community. 3. Provide consultation services that enhance the well being of the campus community. 4. Provide training experiences for advanced graduate students in human service disciplines so they can become effective providers of psychological and counseling services. Counseling Services is a part of University at Buffalo’s “Wellness Team.” The Wellness Team is also comprised of Health Services and Wellness Education. All of these units are a part of the Division of Student Affairs. STUDENT WELLNESS TEAM Mission Statement The Student Wellness Team fosters optimal academic functioning and social development through services and strategies that enhance multiple dimensions of individual health and cultivates an environment supportive of life-long healthy behaviors. Vision Statement Putting “Students First,” the UB Wellness Team is committed to empowering students to play an active role in their wellness. Objectives: 1. The Wellness Team fosters a holistic view of wellness, encompassing physical, emotional, intellectual, environmental, social, cultural, occupational, and spiritual health. 2. Staffed by caring professionals, the Wellness Team offers primary health care, mental health services, wellness education, sexual health services, and nutritional counseling, as well as consultation, prevention, and training programs to the University at Buffalo community. 3. The Wellness Team is committed to excellence in compassionate, inclusive, student-focused care. 6 Equal Opportunity The University at Buffalo (UB, University) is committed to ensuring equal employment, educational opportunity, and equal access to services, programs, and activities without regard to an individual's race, color, national origin, sex, religion, age, disability, gender, pregnancy, gender identity, sexual orientation, predisposing genetic characteristics, marital status, veteran status, military status, domestic violence victim status, or ex-offender status. This includes, but is not limited to, recruitment, the application process, examination and testing, hiring, training, grading, disciplinary actions, rates of pay or other compensation, advancement, classification, transfer and reassignment, discharge, and all other terms and conditions of employment, educational status, and access to University programs and activities. Employees, students, applicants or other members of the University community (including but not limited to vendors, visitors, and guests) may not be subjected to harassment that is prohibited by law or treated adversely based upon a protected characteristic. The University will provide accommodations to individuals with disabilities in accordance with its Reasonable Accommodation Policy. The University will also provide accommodations to ensure the full participation of individuals in University programs, when such accommodations are reasonable and necessary due to an individual's religion, pregnancy, maternity, or breastfeeding status. COUNSELING POLICIES AND PROCEDURES Eligibility for Services 1. All currently enrolled full, part-time, graduate, undergraduate, and ELI (English Language Institute) students are eligible for counseling and health services. Students on a Leave of Absence are NOT currently enrolled and are not eligible for counseling. Counseling services are defined as an initial assessment appointment in which recommendations will be made regarding whether a client will continue to receive services at UBCS or if a referral will be made for on-campus or communitybased services. Note: Students who are under the age of 18 are generally considered minors and different criteria apply (see Appendix A - Treatment of Minors Policy). International students who are in the OPT (Optional Practical Training) Program need to show a valid OPT card, provide a letter from their department saying they are in the program, or provide a letter from the Insurance Office stating their status. Visiting Scholars need to provide a letter from their department stating that they are a visiting scholar or a letter from the Insurance Office stating their status. Visiting Scholars must pay the health fee to be eligible to utilize services. 2. All faculty and staff are eligible for consultation regarding student related issues. For faculty and staff seeking psychological treatment, we provide referrals to off-campus providers. Referrals are also available to faculty and staff through the EAP office at (716) 829-2231. 3. Access to Services: Fall semester Health Fee will enable students to use services from August 1st to December 31st. Spring Semester Health Fee will enable students to use services from January 1st to July 31st (note bullet b. below). Students on campus for a summer orientation prior to August 1st may be seen for emergency concerns only. Students registered for a summer session are assessed the summer health fee (listed as the comprehensive fee) and are, therefore, eligible for services until the end of the summer session that they are registered for, or until July 31st, whichever is later. EOP students are eligible for services prior to their first semester, SHS will obtain consent for underage students. a. Postdoctoral Associates and Residents are not eligible for services. Students supported by Fellowships are eligible to be seen if they are registered for coursework. b. Non-UB students who are attending UB Summer School are eligible for services only while attending summer sessions. Since each summer session is only six weeks long, this needs to be 7 c. d. e. f. g. h. i. j. k. discussed before a decision for on-campus treatment is made. Students attending summer academic programs (ELI, Fulbright Scholars, CADS/EOP, and Summer Research) are eligible to be seen without payment of the summer health fee (their fees are waived by the University or paid for by their department). Students must identify themselves appropriately. Summer research participants will be eligible only if we have received a list from their department. If a student is leaving, graduating, or transferring from the University at the end of the fall semester, they may continue to receive services through December 31st. If a student is leaving, graduating, or transferring at the end of the Spring Semester, they may continue to receive services through June 1st. Counselors should not automatically offer services to students who, though eligible for services, will be leaving town or graduating soon. Counselors should instead weigh the benefits and the possible negative consequences of offering services within such a limited timeframe. Furthermore, if a referral seems appropriate, the counselor should explain to clients the rationale and benefits of the referral as opposed to on-campus services. Students who withdraw involuntarily or are suspended from the University during the semester are not eligible to receive services for the semester unless they receive the approval to do so from the Office of the Vice President for Student Affairs in consultation with the Director of Health or Counseling Services. Students who withdraw voluntarily from the University during the semester may continue to receive services for the remainder of the semester upon the approval of the Director of Health or Counseling Services. This approval is based on the Director’s assessment of the appropriateness of continuing care here at the University. Students currently affiliated with Counseling Services in any work or training capacity (WorkStudy, Field-Work, Intern, Research Assistant, Independent study, etc.) will not be seen by Counseling Services’ staff for counseling. They may be referred to Psychological Services (6453650) or an appropriate resource in the community. Students who have previously been affiliated with UBCS in a training capacity, who are otherwise eligible for services at UBCS, will not automatically be ineligible for services at UBCS because of their former trainee status. However, they will be encouraged to seek services from other community providers when possible. If seen at UBCS, former trainees may only be seen by a staff member who was not involved in the training experience so that there is minimization of dual role conflicts with providers who may have been involved in their training. In that situation, the clinical issues cannot be related to other trainees or faculty of the academic department or UBCS staff. In situations in which a clinician knows or suspects a student is not eligible for services, the clinician is to communicate this to the student. Professional ethics require an appropriate referral be given to the student for continuity of care. If there are lethality or safety concerns for the student, consult with your supervisor or senior staff to provide a safety plan for the student. Academic Dismissals: Students who have been academically dismissed and involuntarily withdraw for academic reasons may receive services at the discretion of the Director of Health or the Director of Counseling Services. Disciplinary Suspensions: Students on disciplinary suspension are generally not allowed on campus and not allowed access to services, including Counseling Services. If the suspended student is in crisis, the VP for Student Affairs, in consultation with the Director of Health or the Director of Counseling Services, will arrange appropriate care, which may or may not include services provided by Counseling Services. Medical Withdrawal: This is a voluntary withdrawal in which the student is no longer registered and, therefore, not eligible for services. Limitations of Services 1. All eligible students will be allowed a maximum of 14 sessions per academic year. Clients should be informed of session limits at the initial assessment. 8 2. Senior Staff and psychology interns will be able to have 2 clients on their caseloads with treatment exceeding the 14-session limit. 3. Case audits will be performed at least once per semester verifying the session limits (see Appendix B and Appendix C). 4. Part-time trainees will be required to follow this policy. Their appropriate coordinator and/or supervisor, in consultation with CS Director or Associate Director, will determine if more sessions are appropriate. 5. Clients are not permitted to participate in a process group and individual therapy simultaneously. Initial Assessment Procedures 1. Students request services either in person or via telephone and are scheduled for the earliest available initial assessment appointment. Students are instructed to arrive 30 minutes early for their appointment to complete paperwork (see H: drive under Forms). The paperwork should be reviewed prior to the initial assessment, taking special notice of issues of lethality and other risk factors (e.g., substance abuse). 2. Students who present in person (“walk-ins”) will be asked to review the “Same Day Emergency Consultation” form whether they indicate that they are in an emergency or not. If they indicate that they need to speak with a counselor that day, they will be seen by a crisis counselor. If after reviewing the form the student indicates that their need to see a counselor is not urgent they can be offered an available same-day initial assessment appointment (if available). Support staff must ensure there is enough time for the student to fill out paperwork. 3. It is standard policy for Initial Assessment paperwork to be completed in the office. However, it is within the counselor’s discretion to allow completion of the paperwork outside the office if s/he determines it appropriate. All students read and sign the Rights and Responsibilities sheet detailing rights and expectations, the original signature sheet is placed in the file and the carbon copy given to the client. (See Appendix D). 4. Designated staff members (senior staff and psychology interns) are “on duty” each day to provide assistance to crisis clients, consultation to trainees, and phone consultations. 5. If a student received services at UBCS in the past, it is important for the currently assigned clinician to review the previous file. If treatment was prior to 2000, all counseling information will be in a paper file. 6. If a student is late for his/her initial assessment, the counselor should make his/her best effort to complete the initial assessment, possibly suggesting the client fill out minimal paperwork prior to the interview and complete the remaining after the initial assessment. A general rule is that if there is at least 30 minutes to conduct the initial assessment, it should be attempted. It is the counselor’s responsibility to inform the client if the initial assessment needs to be rescheduled and assist the client in doing so. This allows the counselor to complete a lethality/risk assessment prior to rescheduling. It is important to inform the client of crisis hours and the counselor-on-call. 7. During initial assessments conducted at the end of each semester, clients should be asked if they will be at UB the following semester. If clients are leaving or graduating at the end of the current semester, consider the following treatment options: a. The initial assessment counselor sees the client for one or two sessions. 9 b. Trainees who will be completing their clinical work at Counseling Services during the same time frame can see the client for one or two sessions. 8. During initial assessments or crisis appointments, specific details about a student’s situation are obtained and a recommendation made about an appropriate course of action. At the beginning of the initial assessment, clients should be told, “Currently enrolled students are eligible for an assessment at Counseling Services at the end of which one or more of the following recommendations will be made: counseling on campus, referral to other services on campus, or referral to a mental health provider in the community. If necessary, students may receive up to 14 sessions of individual or couples counseling per academic year.” 9. All students should be asked about their preference for taping of future sessions during the initial assessment using the following script: “We are staffed by social workers, psychologists and graduate students in both of these professions. We are a training center and value supervision at all levels. Your assigned counselor may ask your permission to video-record your sessions. That allows us to do good supervision and ensure that you’re getting the best services. Do you have any questions or concerns about that? Is that okay with you?” 10. Clinical judgment should be utilized in asking a student about any strong preferences for treatment (i.e. counselor gender); this should be avoided as a regularly asked question during initial assessments. A standard response to stated preferences should be that we will try to honor the preference, but note that it could mean a longer wait for services. 11. Trainees who are considering referring a student to off-campus services must consult with their supervisor. 12. Ideally, initial assessment summaries should be completed by the next clinical meeting, but should take no longer than 5 work days. The Risk Assessment, Crisis Plan, and Recommendations/Plan sections must be written on the day of the initial assessment. 13. If issues of lethality or risk are present, all part-time trainees must consult with a staff person during the initial assessment. It is also recommended that senior staff consider consultations in response to issues of lethality or risk. The consultant should review and append the case note, documenting the consultation. Consultation paperwork should be completed and submitted to the staff person consulted with on the same day of the consultation. 14. If a student is not picked up for counseling by the initial assessment counselor then the counselor needs to inform the student that she/he will be assigned to a counselor at the next clinical meeting and that the new counselor will contact her/him. The student is the responsibility of the initial assessment counselor until she/he has been assigned. It is important to make sure that the student knows how to contact the initial assessment counselor in case an emergency occurs. An exception applies in the event that the counselor is a part-time trainee and the client is in need of immediate assignment due to crisis or lethality, in which case the part-time trainee is to notify her/his supervisor and the client becomes the responsibility of the supervisor. 15. At the end of the initial assessment, all students should be given a copy of the “What Happens Next form” (see H drive under Forms). 16. At the end of the initial assessment, all students should be informed of the availability and appropriate use of our crisis services. 10 17. All cases should be assigned during the clinical meeting at which they are presented. If the case does not get assigned, it should be discussed at that day’s staff meeting. Supervisors are responsible for assisting trainees in getting cases assigned. 18. When designating whom to assign cases to, use the following designations: a. Beginning Level b. Middle Level c. Advanced Level d. Not on this scale is a “Senior Staff Only” designation which would be appropriate for clients who refuse taping or some other special circumstance. These labels will be used in the Recommendations section for the Initial Assessment report and on the Waitlist forms to indicate the level of counselor appropriate for working with that particular client. Please note: a. All supervisors and supervisees should discuss these levels with each other so that every supervisee knows where they are on this scale. This information will be important when knowing the type of clients with whom supervisees can work. b. Supervisees’ level will change during the course of their time here, so they should periodically check in with their supervisor to assess their current level. c. This scale is a guideline, not a set-in-stone rule, so there may be some flexibility around some of the characteristics belonging to each severity level. What is most important is that each counselor knows his/her own level. d. See Appendix E - Guideline for Case Disposition and Counselor Assignments for specific guidelines. 19. When referring a student to group, the initial assessment counselor needs to fill out a Group Referral form (see H drive under Forms) and place it in the mailbox of the appropriate group leader(s). After the screening and assuming the client is accepted into the group, the group co-leaders should reassign the case to the appropriate group in Titanium. 20. If a trainee completes an initial assessment of a client that needs immediate assignment (crisis situation), the case should be discussed directly with his/her supervisor or a senior staff person while the student is still in the office. The part-time trainee’s supervisor will be responsible for making sure the case gets picked up in a timely manner if it is determined that the client requires immediate assignment. 21. After the initial assessment, return the case file to the support staff for data entry before the end of day. Attach a note to the file directing support staff where to place the file after data entry. 22. We will endeavor to respect students’ requests for specific counselors. The request should be discussed with the student and documented. Note: A client should not have a trainee from his or her academic department as a counselor. Referral Guidelines and Procedures 1. Guidelines for Referrals a. After the initial assessment, a recommendation for use of our services (as well as other campus and community resources) will be made in light of the client’s presenting problem, eligibility considerations, counselor assessment/conceptualization, staff clinical expertise, and how we believe other outside resources can best help. 11 b. In some cases, none of our services will be recommended and only outside referrals will be made. c. It is important to remember that providing an initial assessment, forming a clinical decision, and making a referral is the provision of service, not the refusal of service. d. Students will not be denied campus services as they may need emergency services. However, if a client presents with one or more of the factors below, careful assessment of potential benefit from Counseling Service’s services should be completed before on-going therapy is offered. e. If a student is being referred off-campus, a Referral Process form should be filled out and given to the student with the carbon placed in the student’s file. The form provides information to help in facilitating a successful link with a community provider (See Appendix F – Referral Form) 2. Criteria for Referral to Community Service Providers: a. Client’s needs are beyond the scope of practice available at Counseling Services (e.g. issues or problems for which our staff lacks experience or training). b. Client needs more frequent sessions than Counseling Services can provide or has exceeded Counseling Services session limits for the academic year. c. Client is likely to have or prone to frequent crises (e.g. other professional staff frequently involved in emergency care and/or case management of client, client likely to require 24 hour monitoring). d. Client refuses to provide information necessary for an assessment/initial assessment. e. Client refuses to sign informed consent form. f. Client is seeking an evaluation for legal or other purposes (e.g. documentation or support of psychological disabilities, forensic evaluation, and child custody evaluation). g. Court ordered treatment. h. Situations in which Counseling Services and/or its staff would be in conflicting or dual roles by providing treatment (e.g. student is a trainee at Counseling Services). i. Client needs a service that we do not provide or that another office specializes in (e.g. hypnosis, academic advising, job search, study skills). j. Client does not appear motivated to change or, if motivated, is unwilling to pursue counselor’s professional recommendation for treatment (non-compliance). k. Client and therapist are unable to arrive at mutual therapeutic expectations. l. Multiple diagnoses or severe problems that require more comprehensive response and continued follow-up than we are able to provide. m. A client for whom short-term therapy could be anti-therapeutic and/or unethical (e.g. triggers abandonment issues, unable to provide continuity of care because of academic status changes). n. Client is likely to have a significantly shorter wait for services if an off-campus provider is utilized. Wait List Policy 1. Wait List Forms a) The Wait List Form is to be completed for all initial assessments regardless of whether they are picked up by the IA counselor or put on waitlist. This form should be placed in chronological order in either the “Cases to be assigned” folder or “Cases picked up” folder, located in the file cabinet in the front office (see H drive under Forms). b) The client file should also be put in the file cabinet, behind the wait list folder, with a copy of the initial assessment placed in the file. c) The Clinical Director will inform staff and trainees when there is a wait list and when the wait list is no longer in place. 2. Clinical Meeting (Tuesdays at 8:30 am) a. The Clinical Director will distribute Wait List Forms and charts to clinical team leaders prior to the Tuesday clinical meeting. 12 b. Clinical Team leaders will prioritize the assigning of wait-list clients at the Tuesday meeting. Urgent clients should be given priority, followed by clients who have been waiting for services the longest. “Urgent” refers to clients who should be picked up soon, but are not an imminent danger to self or others. c. Once a counselor is assigned, the Wait List Forms should be placed in alphabetical order in the “Cases picked up” folder by the team leaders immediately after the clinical meeting. d. Clients in crisis should not be placed on the wait list. Appropriate arrangements should be made immediately. Trainees should first discuss the case with their supervisor. “Crisis” refers to clients experiencing lethality concerns that place them at imminent risk of harm to self or others. e. To ensure fairness, staff and trainees should refrain from picking up their initial assessments when there is a wait list. Instead, priority should be given to cases on the wait list. Any exceptions to this policy should be discussed with the Clinical Director or your supervisor. f. At the clinical meeting, staff members will rotate presenting wait-list cases, focusing primarily on Presenting Problem and Lethality/Crisis concerns. Brevity is encouraged to allow time for all cases to be assigned. g. The priority for clinical meeting is as follows: i. Present/Assign urgent cases ii. Assign wait-list cases iii. Case consultation 3. Wait List Clean up: During end-of-semester periods there may be clients still on the wait list who will likely not be picked up until the next semester. It is important to make contact with these clients to determine their availability for the next semester since this information is needed to assign someone for counseling. a. Contact the clients you are responsible for on the wait list via a method s/he has approved (e.g., letter, email, or phone). b. Ask the client to send you his or her appointment availability for the next semester. c. Instruct the client to respond within two weeks. d. Explain to the client that his/her file will be closed if we do not hear back by the specified date. e. Document all client contacts in Titanium. f. Remove the client from the wait list if they indicate they are no longer interested in counseling or if they fail to respond by the deadline. Group Therapy Policies and Procedures 1. Group counseling is a significant modality of treatment at Counseling Services. During initial assessment, consideration should be given to referring the client to group. 2. A Group Referral form should be completed when a client is referred to group (see H drive under Forms). Put the Group Referral Form in the mailbox of one of the co-leaders. Have support staff file the case unless it needs to be given to support staff for data entry. Referral forms are not filled out for clients referred to any drop-in group. 3. A listing of groups, times, and current openings can be found on the desktop of all computers. Short-cuts can be found in the short-cuts folder on the H drive: H/Counseling Services/Desktop short-cuts. Go to the folder, right click on the short-cut, and click on “send to desktop.” This will allow easy access to the information. 4. The case should be transferred to the appropriate group on the computer system and the case should be filed. a. Specific information regarding how to refer and schedule clients for a group screen/orientation can be found on the Group Opening icon on the desktop or in the Group file on the H drive. 13 b. All groups (excluding drop-in groups) are videotaped. Group leaders will have group members sign the Consent to Record Form at orientation, which should be placed in the client’s file (see Appendix G - Consent to Record Form). c. At orientation, group members also sign a Group Confidentiality Agreement, which is also placed in their file (see H drive under Forms). d. If a client does not show for group orientation, follow-up contact should be made with the client by the group co-leaders. e. Satisfaction Surveys are given to all group members at the end of each semester. If a student leaves group prematurely, co-leaders should make attempts to have the student complete a Satisfaction Survey (see H drive under Forms). f. A cover letter from the group coordinator (see H drive under Forms) is available at H:\Counseling Services\Groups and should be sent with the satisfaction survey to clients who leave group prematurely. Clients should also be provided with a self-addressed, stamped envelope in which to return the survey to the group coordinator. Couples Counseling 1. Non-student spouses or significant others of currently enrolled students may receive services only when they are seen jointly with the student. 2. If a counselor determines that the non-student in the couple needs crisis or other forms of treatment, the non-student will be given referrals to mental health providers in the community. 3. If the student in a couple decides to terminate treatment, the non-student will be given referrals to mental health providers in the community. 4. Prior to receiving services, the non-student in the couple will be given a copy of this policy and will be asked to sign it (see Appendix H – Couples Counseling Policy for Non-Student Partner). 5. An initial assessment summary and session notes must be completed for both participants in couples counseling. Support staff will need to create a file for the non-student in the couple. To protect confidentiality, identifying information about the partner should not be found in either participant’s file. Psychiatric Services and Procedures 1. Initial appointments with a psychiatrist or psychiatric resident are to be scheduled for one hour. 2. All follow up appointments with “psychiatrists” are to be scheduled for 20 minutes. All follow up appointments with “psychiatric residents” are to be scheduled for 30 minutes. Note that an appointment code with a 30 minute default, labeled “Psychiatric resident follow up, 30 mins.,” is to be used for follow up appointments with “psychiatric residents” only. 3. If finding time in the schedule is difficult and it is urgent that a client be seen, please consult the psychiatrist regarding scheduling. 4. All documentation should be current on the computer prior to the psychiatric appointment ensuring the psychiatrist has all pertinent information. To ensure time for pertinent documentation, psychiatric appointments should be scheduled no earlier than three days following the initial assessment. 4. In general, psychiatric appointments are not to be scheduled from 8:30 AM to 9:30 AM on Tuesdays as the psychiatrists attend the weekly clinical meeting. However, appointments may be scheduled 14 during that time period if the client would have to wait more than TWO weeks for a psychiatric evaluation and during this time is likely to decompensate to the extent that it would negatively impact her/his functioning (e.g., ability to care for self, increased lethality risk, severe and negative impact to academic functioning) a. This time slot is not to be used for follow-up appointments unless it is of an urgent nature (e.g., severe side effects of the medication, increase in lethality risk) b. Externs, advanced pracs, social work interns, and clinical grad assistants should consult with their supervisor prior to scheduling an appointment during this time. c. Support staff should not schedule appointments during this time without prior approval of a senior staff counselor, psych intern, or the supervisor of the part-time trainee. 5. Unless specifically instructed to do so by the psychiatrist, please do not schedule appointments during the psychiatrists’ lunch hour (12-1). Support staff is to block out the 12-1 PM hour as lunch time. 6. Students are required to be in counseling in order to be seen by a Counseling Services’ psychiatrist. In most cases, students who are insistent on medication only are to be referred off-campus for psychiatric services. Exceptions to this policy need to be carefully considered and discussed with the psychiatrist. 7. In most cases, the psychiatrist will not be the primary provider of counseling services. The psychiatrists’ primary functions are to evaluate students and to prescribe and monitor medications. 8. For students receiving both counseling and psychiatric services at Counseling Services, it is the counselor’s responsibility to communicate with the psychiatrist whenever active lethality concerns emerge or hospitalizations, medical issues, and/or major disruptions occur. Contact with psychiatrists may occur via phone or email; clinicians need not wait to consult or communicate with the psychiatrists when they are in Counseling Services. The psychiatrists do not have access to Titanium or person numbers outside of Counseling Services so use client initials and a brief description of the clinical presentation to discuss clients. 9. All requests from clients for medication refills should take place during scheduled appointments with the psychiatrist. If a student calls in to request a medication refill, the front desk will direct the call to the student’s counselor who will make the decision how to proceed. 10. Some things to keep in mind for students on medication: a. Students should make an appointment at least three weeks in advance for prescription refills or arrange this ahead of time when meeting with the psychiatrist/resident. b. The Sub-Board I Pharmacy, located in the basement of Michael Hall, South Campus, fills prescriptions very inexpensively. It is open during the academic year, closing during breaks and in the summer. 10. Psychiatrists requesting services from the Sub-Board I, Inc. Laboratory can write lab orders on ECMC prescription pads but must include the following information: a. The address where the lab results are to be mailed (Counseling Services, 120 Richmond Quad) b. The ICD-9 diagnostic code 11. Information most relevant for front desk staff: a. Front desk are to make sure that psychiatrists’ schedules get blocked out during times UBCS is not open (holidays, Winter Break reduced hours) to ensure that clients do not get scheduled during these times and have to be inconvenienced by being rescheduled. b. Front desk are not to schedule a client with the psychiatrists unless there is a note directing them to do so in Titanium, which the counselor must write. 15 12. Information most relevant for Counselors: a. UBCS requires clients to be engaged in counseling to qualify for psychiatric services. Any exceptions to this policy must be discussed with your supervisor; the treating psychiatrist must be consulted as well. This should be documented in Titanium. b. Since clients need to be engaged in counseling to utilize psychiatric services at UBCS, clients should not be scheduled for a psychiatric intake by the crisis counselor or the IA person, unless there is risk to the client if they were denied a psychiatrist appt. P/T trainees should consult with their supervisor prior to making this decision. The reason behind this is client safety, as we do not want a client that has not been fully assessed (by IA) and who is not engaged with a counselor who can follow up and monitor side-effects, to start medication and then not follow through with counseling and risk not being able to continue their medication. c. If a crisis counselor schedules a client with the psychiatrist, the client’s primary counselor should be informed, although if the client already has a counselor, it is best practice to consult with the counselor prior to scheduling the appointment. d. Counselors must review and have clients sign the Psychiatric Consent form, placing the carbon copy in the file. Counselors must review the “Psychiatric Services Informed Consent Form” (see Appendix I) with the client and both the client and the counselor must sign the form, placing the carbon copy in the file. It is the responsibility of the counselor to ensure the policy is maintained. e. Counselors have the responsibility for adding or removing the psychiatrist’s name on the client security tab on Titanium. f. Front desk will not schedule a client with a psychiatrist unless there is a note directing them to do so in the client’s file in Titanium, which the counselor must write. g. Counselors must inform psychiatrists (preferably thru email) when a case if closed. This will prompt the psychiatrist to then lock the medication log. 13. Information most relevant for Psychiatrists: a. While front desk “checks in” clients, it is the responsibility for the psychiatrists to document (on the appt) if a client no shows, this is done by right clicking on the appt and checking attendance, no show. b. Counselors must inform psychiatrists (preferably thru email) when a case if closed, this will prompt the psychiatrist to then lock the medication log. Crisis Intervention When clients walk in for a crisis intervention session or utilize the after-hours on-call crisis service, it is vital that all staff members share a consistent philosophy and attitude, and expectations about crisis intervention that will be clearly communicated to clients. It is also important that staff members clearly communicate the purpose, function, goals and proper utilization of UBCS’s crisis intervention services to their counseling clients, new UBCS staff, UBCS trainees, and the UB community. Such clarity and consistency is beneficial for both staff and clients in minimizing confusion, frustration, and disappointment for everyone involved. UBCS Philosophy on Crisis Intervention Crisis intervention services are designed to assist students who are confronting life-threatening circumstances, current or recent traumatic experiences, serious mental illness, and concerns about the safety of self or others (e.g. suicidal thoughts, thoughts of harming others, recent or anticipated assault or abuse toward self or someone else, hallucinations, recent death of a loved one, etc.). 16 1) Goals of Crisis Intervention a) Containment b) Stabilization c) Immediate safety d) Plan for further treatment or follow-up as necessary 2) What Crisis Intervention is NOT a) Therapy b) Substitute for therapy contact with regular counselor c) Emotional support or an avenue for venting frustration, in the absence of lethality or real crisis d) A means for client to get access to a counselor other than his/her assigned counselor e) A bridge between therapy sessions with their regular counselor – if client truly needs more frequent contact, this should be arranged within the therapy relationship/process 3) Crisis Situations a) Crisis situations include, but are not limited to the following: i. The situation has high potential for the client to either hurt him or herself or someone else. ii. Client’s ego functioning has deteriorated to the point of active psychosis. iii. The client is so profoundly depressed that assessment for hospitalization should be considered either because of suicide potential or until the profoundly dysfunctional nature of the disorder is clearly determined. iv. The client is unable to resolve the crisis or contract for safety without further intervention, such as assessment at a local psychiatric emergency room or another acceptable supervisory and remedial environment. Supervision by an RA is NOT considered an adequate solution. 4) Recommendations for Crisis Intervention a) Establish a clear contract, agreement, or understanding about the nature of and goals for the crisis contact; set clear boundaries for the crisis contact (e.g. this is not counseling, focus on the immediate crisis at hand, attend to physical safety concerns) b) UBCS does not use “No Suicide Contracts” with clients. This is a non-legal client agreement with a counselor to not complete suicide. Such contracts have not been demonstrated to reduce suicide. Reliance on a contract may reduce vigilance or lead to unwarranted comfort about a person without reducing his or her suicide risk. A client’s referral for a psychiatric evaluation at a hospital should not be based on the person’s willingness or reluctance to enter into a no suicide contract. Furthermore, since suicide prevention planning is favorably impacted by having an established client-counselor relationship, no suicide contracts are not recommended for use with new clients, in crisis situations or with psychotic or impulsive individuals. However, after a thorough risk assessment and consultation (if needed), counselors may use a safety plan which list of warning signs, coping responses, and support sources that an individual may use to avert or manage a suicide crisis. This plan is typically used after it has been determined that the client does not need further evaluation at a hospital. c) Assist client to problem solve around self-care, decreasing immediate distress, and developing a viable plan for safety d) Assist client to expand and utilize existing potential support resources e) Negotiate the “next step,” setting up a clear plan for ongoing or future treatment, and/or follow-up as necessary, including: i) a plan to contact current counselor ii) make an appointment for an initial assessment at UBCS or community mental health provider iii) follow-up check-in with crisis counselor specifically around safety and immediate crisis concern iv) arranging for transport to ECMC CPEP (see Appendix J – CPEP Evaluation Referral Procedures) for further evaluation of safety and functioning v) obtain consultation or assistance from other UBCS staff during crisis intervention process as needed 17 f) Following crisis intervention, counselors should: i) debrief as necessary with other staff ii) communicate necessary information about the crisis contact and disposition to relevant UBCS persons or other professionals as appropriate iii) document crisis contact content, process, and disposition, especially any lethality issues as soon as possible (i.e. before leaving work, or next morning following an after-hours on-call crisis phone contact) iv) if the contact is an after-hours on-call crisis intervention, you should also make entry in the oncall log v) follow through on any follow-up arrangements made with the client 5) Procedure a) In the event a student presents in crisis, the following procedures should be followed: i) The student will be scheduled for the first available initial assessment appointment available that day. If there are no same day initial assessment appointments available and the student appears to be in crisis or too distressed to wait for an initial assessment that may be days or weeks away, the following steps should take place: (1) Front desk staff will ask the student to review the “Same-day emergency consultations” form (see Appendix K). If the student identifies being in crisis after reviewing the form, they will be asked to fill out the Harm to Self Questionnaire and the first page of the initial assessment paperwork. (2) Support staff is not responsible for determining who can or cannot wait to be seen. (3) The student will see the counselor covering the crisis hour at that time. If the counselor covering crisis during that time is currently with someone, support staff will inform the student that the counselor will be with them shortly. (4) If the crisis counselor is in with a student, the support staff will phone the counselor to inform her/him that a second student is waiting. This informs the counselor that a decision needs to be made about whether he or she will have time to see the second student. If the crisis counselor determines that s/he will not have time to see the second student, s/he will direct the support staff to find another counselor to see the second student and our established protocol (decision making tree) for obtaining another counselor will be put into action. (5) If the student is in such obvious distress or insists they are not able to wait, support staff will use previously established protocol should be followed to determine which counselor should be interrupted. 6) Guidelines for Interventions (See Appendix L - Guidelines for Assessing Suicidality) a) It is recommended that staff consult regarding appropriate steps to take in crisis intervention. b) Consultation with any available senior staff person is required of part-time trainees. c) After obtaining written consent, it may be appropriate to involve other relevant parties who can assist in the intervention. d) If a psychiatric assessment for hospitalization is required, the student needs to be transported to CPEP (Comprehensive Psychiatric Emergency Program), located at the Erie County Medical Center (see Appendix J - CPEP Evaluation Procedures). Buffalo General Hospital also has a psychiatric emergency room (see Appendix M – NYS Mental Hygiene Law – Hospital Committals). e) Students should refer to their health insurance policy for information concerning coverage and cost of ambulance transportation. The international student health insurance plan may waive a deductible charge if the student is referred for transport by Student Health Services. In this event, a Health Insurance Claim Form may need to be completed (see Appendix N – Health Insurance Claim Form for International Students Transported by Ambulance). f) All crisis intervention activities need to be documented immediately. g) The Director and/or the Associate Director are to be informed immediately when a student is transported to the hospital. h) The Hospital Transport Log must be updated (H:\Counseling Services\Hospital Transport Log). 18 i) If a student off campus is in imminent crisis, UBCS staff may make a referral to Crisis Services Mobile Outreach Unit. The Mobile Unit is able to do on-site crisis/lethality assessments and arrange for transport to a CPEP, if appropriate. There will be a charge to the student that may or may not be covered by his/her health insurance. 7) Guidelines for UBCS Interactions with CPEP a) In emergency situations, Counseling Services staff can speak to CPEP staff without obtaining a written release first. Please be aware that secretarial staff is not empowered to share any client information. Secretarial staff will relay any request from CPEP to a counselor. To protect client confidentiality, the counselor may elect to call the CPEP nursing station (898-3465 or 898-3289) to verify that this is a legitimate call. b) At discharge, CPEP will do the following: i) Fax UBCS information about the student’s recent visit to CPEP and the discharge needs prior to calling to schedule an appointment for the student. After the faxed information has been reviewed, Counseling Services will contact CPEP regarding the student’s appropriateness for services at UBCS. The student need not be present when the CPEP discharge planner makes the appointment. ii) Contact University Police by calling 645-2227 or 645-2222 (for emergencies); if the student is a client at Counseling Services, CPEP will inform UBCS by calling 645-2720. 8) Duty to Warn a) Counselors’ duty to warn refers to the responsibility of a counselor to breach confidentiality if a client or other identifiable person is in clear or imminent danger. This duty applies when there is clear evidence of danger to the client or other persons. The counselor must determine the degree of seriousness of the threat and notify the person in danger and others who are in a position to protect that person from harm. b) Criteria: How serious is the intent? Is there a specific plan? Is the plan feasible? Does the client have means to carry out the plan? Is there a past history of harm or threat of harm to others? c) When duty to warn is necessary: i) Express your concern and commitment to prevent harm to others. ii) Get the intended victim’s name. iii) Pursue the following steps whether the student gives you the name or not: (1) Consult with a supervisor while the student is in the office. (2) Consult with Counseling Services’ Director or Associate Director. (3) Come to a joint decision about a course of action. (4) Implement decision - If it is to warn intended victim(s), do so. (5) Document all consultation, discussions, decisions and steps taken. (6) Director will contact all appropriate parties. (7) Never implement “duty to warn” without the above steps. 9) Counselor-on-Call a) Senior Staff and Psychology Interns rotate being on-call and carrying Counseling Services’ cell phone. The Associate Director develops a schedule at the beginning of each semester. On-call responsibility begins at 8:30 am Tuesday mornings and ends the following Tuesday at 8:30 am. b) The schedule for Counselor-on-Call is faxed to University Police (UPD). If a call is made to University Police by a student who is in crisis, or UPD believes intervention is needed by a counselor, they will call the counselor-on-call and request that the counselor call the student. Consultations with other staff members should be made as needed. All interventions should be documented appropriately in both a progress note and in the on-call log on the desktop, and followup arranged as needed. c) If the student in crisis is a current client, use your clinical judgment to decide if the student’s counselor needs to be consulted. It is the responsibility of the counselor-on-call to make sure the 19 counselor is available and able to respond by phone immediately or in person within a reasonable amount of time. d) Any changes to the on-call schedule should be communicated to staff and changes faxed (not emailed) to UPD. The staff person making the change should also email the updated schedule to all staff and ensure the updated schedule is placed in the on-call folder. e) Please see Appendix O – Crisis Client Procedures for more information. 10) Responding to the Death of a Campus Member a) In most cases, the Director will be notified by another office that the death of a student, faculty, or staff member has occurred. If you are the first to be notified, you must immediately contact the Director. If the Director is not available, contact the Associate Director. If neither is available, and you are not certain that the Office of the Vice President for Student Affairs has been notified, you should contact that office. b) The Director or a Counseling Services designee will coordinate the provision of services from Counseling Services. c) The Office of the Vice President for Student Affairs will coordinate the overall university response. d) As soon as is possible after notification of the death, the Director will call a staff meeting to inform the staff of the event and determine the staff resources available to deal with proceeding events. e) The Director or a Counseling Services designee will contact affected offices and groups at the university to offer assistance and determine the need for service. f) The Director will assign duties as required. g) Some of the responses that Counseling Services might make would include: i) Provision of individual crisis counseling to students directly involved with the person or those who witnessed the death. ii) Group meetings/counseling to those close to the person, (e.g. residence hall floor, student organization, academic class). iii) Crisis support to parents/family of a deceased student when/if they arrive on campus. iv) Backup services to the Vice President for Student Affairs including answering special phone lines to counsel students or answer questions/control rumors, consultation with residential life staff or other groups. v) Extended initial assessment hours in the days following the death to accommodate any need for crisis/grief counseling by students. vi) Depending on the circumstances, some regular Counseling Services activities will be suspended to accommodate the need for crisis counseling services. vii) Always document any intervention provided and update the Director of Counseling Services’ of interventions made. Crisis Hours 1. It is the designated crisis counselor’s responsibility to find coverage when s/he is unable to be here for a crisis hour. 2. The counselor assuming coverage must put the crisis hour in his/her schedule immediately. The originally designated crisis counselor is responsible for ensuring that the crisis hour has been placed in the schedule of the counselor that is taking on the crisis hour. 3. It is suggested that the person getting coverage note on his/her schedule the counselor that is covering the crisis hour. 4. At times, a request may be made for coverage but no one is available. In those instances, the decision tree, which can be found in Appendix O – Client Crisis Procedures, will be used, thus eliminating the need for the front desk staff to send emails regarding who is covering a crisis hour. 20 5. Counselors and front desk staff should refrain from informing clients of the specific hours during which we schedule a staff member to be the “crisis counselor.” Clients do not need to know that we have a staff member dedicated to crisis situations at 10, 12, 2 & 4 – this pertains to our internal scheduling needs. Instead, students should be told that if they need to speak with someone urgently, they should come to the Richmond office and will be seen by a crisis counselor as soon as one is available. In practice, this means that some students will likely have to wait from just a few minutes to up to an hour to be seen by a counselor. The vast majority of students will be able to wait, and will be seen in a timely way. If a student in crisis appears to be in significant distress and does not seem able to wait, front desk will employ the crisis decision tree to find a counselor who can meet with the student immediately. 6. Front desk staff should not schedule a crisis appointment in Titanium until a student has arrived in the Richmond office and has reviewed the Same Day Emergency Consultations form, and then indicates that they do feel they need to see a counselor urgently. At that time, the client information is to be entered in the next-available crisis hour, and the counselor assigned to that hour should be contacted by phone to inform them that a student has checked in for a crisis appointment. 7. If we have multiple students who need to be seen during a crisis hour, front desk will inform the originally-scheduled crisis counselor, who then needs to respond and make some decision about whether they will be able to see the next student in a timely manner. If the crisis counselor does not feel that they can adequately meet the needs of the current student in a timely way to meet with the next-waiting student, the counselor should report to the front desk that they are tied up and will need front desk to find an alternate staff member to meet with the waiting student. The front desk then needs to use the crisis decision tree (and review schedules on Titanium) to find another staff member who can respond to the waiting student. Front desk should proactively find another counselor who can assist, realizing that staff may not be regularly checking emails and may not read and respond to an email requesting assistance in a timely way. It is expected that all staff members participate equally in responding to emergency situations, including stepping up to help out in the case of multiple students arriving for crisis services around the same time. Mandated Assessments 1. If a student calls Counseling Services stating “I have to make an appointment” or refers to being told to make an appointment, they will be asked by front desk staff if they have been mandated by University Residence Hall, Judicial Affairs, and Office of the Vice President for Student Affairs or Athletics. These are the only offices that may mandate students for an assessment at Counseling Services. 2. A mandated assessment will include a thorough psycho/social evaluation, recommendations, and/or referrals for further treatment. Front desk staff are to inform students of the following and the counselors will do the same: “This assessment involves attending a minimum of two sessions. The second session should be scheduled at the conclusion of the first session, so you will need to have your schedule available. Ideally, the second session should be within 1 to 2 weeks after the first session. If the second session has not been completed within one month of the first session, the assessment will have to be completed by an off campus provider at your own expense.” 3. Counselors should complete a regular initial assessment as part of the mandated assessment, paying special attention to issues connected to the reason for the referral (i.e. substance use/abuse, conflict). 21 4. Information about treatment recommendations and referrals are provided only to the student. When students are referred for alcohol-related violations treatment recommendations can be shared with the referring party with written consent of the student. 5. In accordance with NYS law, Counseling Services will notify relevant others. Typically, confidentiality is broken in situations where the student is in imminent danger to harm self or others, incidences of child abuse, and upon a subpoena from a judge for copies of clinical records. Refer to the Mandated Reporting section of this manual for more information. 6. A Referral Form to mandate services at Counseling Services can be completed by Judicial Affairs, Residence Life or Athletics (see Appendix P – Referral Form for Mandated Assessments). A copy of this form is given to the student being mandated for assessment and a copy is faxed to Counseling Services, along with a brief description of the circumstances that prompted the referral. The same form also provides space for referrals to UB-SAFER or a community mental health provider. 7. The Assessment Verification form will be filled out at Counseling Services upon completion of the assessment (see Appendix Q - Assessment Verification Form). 8. Assessments are completed by senior staff or doctoral level psychology interns only. 9. It is the student’s responsibility to submit the completed paperwork to the office/person that mandated the referral. 10. A copy of the completed form will also be kept in the student’s file at Counseling Services. Use of Assessment Instruments 1. A full range of psychological assessment instruments are available for staff and trainees to use. 2. All trainees must discuss and obtain permission from their supervisor prior to utilizing psychological assessment instruments. 3. Policies and Guidelines for Use of Psychological Assessments, Consent for Psychological Assessment, and Assessment Instruments Available at UBCS can be found in Appendix R, S, and T, respectively. Mandated Reporting Counselors are required by law to report suspected child abuse or maltreatment to the New York State Central Register (SCR) of Child Abuse and Maltreatment. The law also assigns civil and criminal liability to those professionals who do not comply with their mandated reporter responsibilities. When reporting, please note the following: 1. The white and yellow copies of the mandated report are mailed to the county in which the abuse occurred. 2. When reporting via phone (Mandated Reporter Hotline: 1-800-635-1522), note that your oral report must be followed within 48 hours by a written report to the local CPS office. Request an address for the paperwork to be mailed to during your phone call. 3. See Appendix U – Mandated Reporting of Child Abuse for additional information. 22 Multilingual Counselors as Translators UB Counseling Services provides counseling, mental health consultation, mental health education, and crisis intervention to the campus community. Each semester we post information about the languages other than English spoken at Counseling Services. This information is provided so that UB students who prefer to engage in counseling in their native language know that they can do so. Typically, counselors are providing services directly to UB students. However, in assisting a student we may be interacting with others who are concerned about a student such as parents, friends, and other campus personnel. Upon occasion, there may be a situation with a non-student in the larger Buffalo community that requires some type of mental health assistance. If staff is able to assist during these occasions they will make arrangements to do so. However, their role both on and off campus is to assist with the mental health response to a crisis situation. Counselors do not typically serve in the role as translators for non-mental health matters whether the situation involves students or non-students. Furthermore, the ethical codes of most the counseling professions explicitly state that counselors should refrain from entering into a multiple relationship if the multiple relationship could reasonably be expected to impair the counselors objectivity, competence, or effectiveness in performing his or her functions as counselor. For example, if a counselor serves as a translator during a police investigation, this could negatively impact the student’s belief that he or she could receive confidential or unbiased treatment at Counseling Services. Whether true or not, the counselor might be perceived as working on behalf of the police not the student and the student may opt not to make use of our services to his or her own detriment. In situations where translation services are the primary need, the Office of International Students and Scholars Services or the International Institute of Buffalo may be better resources for identifying translators. Counseling Services staff should only be contacted about such matters as a last resort after all other avenues for assistance have been explored. Paperwork Guidelines 1) Initial Assessment a) The Risk Assessment, Crisis Plan, and Recommendations/Plan sections must be written on the day of the initial assessment. b) When a client fails to show for an initial assessment, the clinician must review the client’s record to assess whether there is any indication of lethality risk. If so, follow-up contact is required to attempt to reschedule or otherwise link the client to appropriate care/resources. c) All Master’s level trainees are required to consult when lethality is present either during an initial assessment or during a session. d) Consultation with another staff member about lethality must be written by the person who consulted and submitted to the consultant on the same day. e) There is a consultation template on Titanium that must be used, the consultation note should be a stand alone documents, see the P/t trainee manual for content specifics. f) Initial assessments must be written within one week. g) For clients who have received prior mental health treatment, an effort is to be made to obtain a signed Authorization to Release/Exchange Confidential Information (see H drive under Forms) from the client, after which the completed form should be sent to the previous provider for the client’s treatment records. If the client is unable to complete the Release/Exchange Confidential Information because s/he lacks contact information, please instruct the client to bring that information to her/his first appointment so the assigned counselor can contact the previous provider. The Release/Exchange Confidential Information is to be made for “UBCS,” not the individual counselor. Only one Release/Exchange Confidential Information will be included in each initial assessment folder. If more are needed, they are available with the other forms. h) Supervisors must review and lock the initial assessment note within two weeks of the initial assessment date. i) The initial assessments of all trainees and unlicensed counselors must be reviewed and locked by a designated, licensed locker. 23 j) If someone tries to create a New Client note with the Non-Client Note feature found in the “Open” drop down menu, the following text will automatically appear: DO NOT USE!! IMPORTANT: You are attempting to use the Non-Client Note feature. We do NOT use the Non-client feature in Titanium. We record non-client contacts in the same place we record client contacts. See the handout titled "Non-Client notes.doc" located in H:\Titanium for instructions, or ask your supervisor. Click on CANCEL (above), and then on EXIT to cancel this note. 2) Session Notes a) Session notes should be written within three business days. b) Supervisors have the discretion to negotiate if and how frequently session notes will be reviewed (this may vary depending on trainee level). c) Lethality plans must be documented the same day. d) When comments/feedback are made to notes in Titanium, it is the responsibility of the licensed, designated locker to delete all comments before the note is locked. Trainees are not authorized to delete comments/feedback in Titanium. 3) Lethality Consultation Notes a) Consultations with anyone at any time (not just initial assessments) where lethality is a concern should be documented by the consultee and submitted for review by the consultant the same day and all trainees except psychology interns are required to consult with senior staff. b) The consultee (part-time trainee) will forward their consultation note to the person with whom they consulted. If the consultant is licensed, they will then be the final signature on the note. If the consultant is NOT licensed (either an unlicensed staff member or a psychology intern), then the consultant’s supervisor would be the final signature on the note. Example 1: Tanisha consults with Carissa. Carissa is licensed, so she is the final signature. Example 2: Caralynn consults with Brad. Brad is not licensed so he signs the note after reviewing it and then forwards it to his supervisors for the final signature. c) The consultant must lock the consultation note within one week on the initial lethality consultation. d) All part-time trainees are required to complete the consultation template on Titanium. 4) Other Consultation Notes, Phone calls, & Email a) Out of session client contact or contacts concerning others should be documented within three business days. b) After hours crisis contacts should be noted in the desk top on-call log and in Titanium on the next business day. c) Consultations with someone who is not a UB student are documented the same way as done for students, you would create a client file including all information you have gathered. You would document the activity using the Non-client template. When sufficient student information is given (i.e. name, current or former counselor, age, date of birth, etc.) the consultation should be documented under the student’s name in Titanium. You will need to create a Titanium client record if one does not already exist. d) If you have a consultation about a student and you do not know the name of the student we have a special “client” record with the last name: “NoName”. If you do not know the name of the person of concern, you should enter your notes under this “person’s” record. This already exists, you just need to open this “person’s” record and add the note. The rest of the instructions above will still apply to this special case. e) Lethality/Safety plans must be documented on the same day. UBCS does not use “No Suicide Contracts” with clients. This is a non-legal client agreement with a counselor to not complete 24 suicide. Such contracts have not been demonstrated to reduce suicide. Reliance on a contract may reduce vigilance or lead to unwarranted comfort about a person without reducing his or her suicide risk. A client’s referral for a psychiatric evaluation at a hospital should not be based on the person’s willingness or reluctance to enter into a no suicide contract. Furthermore, since suicide prevention planning is favorably impacted by having an established client-counselor relationship, no suicide contracts are not recommended for use with new clients, in crisis situations or with psychotic or impulsive individuals. However, after a thorough risk assessment and consultation (if needed), counselors may use a safety plan which list of warning signs, coping responses, and support sources that an individual may use to avert or manage a suicide crisis. This plan is typically used after it has been determined that the client does not need further evaluation at a hospital. 5) Termination/Transfer Summary a) Termination and transfer summaries must be written within one month of the last client session. b) A termination summary must be written for each ‘service’ (individual, group, couples) a client receives, even if s/he drop out. c) Termination summaries should be written for all students that have been seen for an initial assessment, regardless of whether they attend subsequent sessions. For clients who fail to show for any appointments/sessions, a termination summary must be written documenting the steps taken to engage the client, such as number of phone calls, emails and all other attempts to contact. For such clients with lethality concerns, due diligence must be made to engage them in services and/or resources and those efforts must be reflected in the termination summary. d) If a termination summary is not written because a counselor plans to see the client on an “as needed basis,” this should be documented in a treatment plan in Titanium. e) For “as needed basis” clients, after a three month time lapse between sessions, a termination summary must be written or a rationale for not doing so needs to be provided. f) If clients will be away for the semester but plan to continue counseling when they return, a termination summary must be written. g) Two weeks into each semester, if there has been no contact between a “returning” client and counselor, the case must be closed and the client will need to schedule another initial assessment to recommence services. h) Whenever a client transfers to a new counselor or a different type of service within our agency, a transfer summary must be written. The only possible exception is when a transfer is temporary due to a short-term counselor illness or absence. i) It is recommended that a termination note be created and saved on the same day as your last session with a client. Until this note is written, do NOT remove the person from your active client list. j) Termination summaries should be written for group clients at the end of each semester even if the client will be continuing with the same group or group leaders in the following semester. k) The termination and transfer summaries of all trainees and unlicensed counselors must be reviewed and locked by a designated, licensed locker. 6) Follow up contact with clients a) When a client fails to show for an appointment, the counselor is to contact the client, clearly stating that the client has two weeks to reschedule the appointment or his/her file will be closed. b) If there are clinical reasons for not abiding by the two-week limit on rescheduling, these should be documented in the treatment plan. 7) Treatment Plans a) Treatment plans need to be completed prior to the fourth session for all counseling clients, noting the focus of treatment, as well as goals and any other significant clinical information. b) As treatment shifts, either a new treatment plan or an update to the prior plan should be documented. c) Treatment plans of all trainees and unlicensed counselors must be reviewed and locked by a designated, licensed locker. 25 8) Case Audits a) Case audits are conducted several times per year at the discretion of the Director. The audits apply to Senior Staff, Interns, Trainees and Support Staff. b) Please refer to the Case Audit Forms (see Appendices W and X) for a listing of what is reviewed during audits. c) Quality Assurance Committee members conduct the audits. 9) It is the responsibility of each counselor to monitor their status on client files in Titanium. Counselors should check their name on cases they are listed active and uncheck their name for cases where they are no longer active. Counselors should be monitoring who is on their caseload and remove clients that are not currently active with them. Other counselors are not responsible to do this task for other counselors, even if the counselor knows that this person is no longer active with this client. The exception to this is un-checking the psychiatrist name if you are sure the client is not active with them. We established this rule to ensure individual responsibility for maintaining caseloads, since each counselor should know best who is or is not supposed to be out their caseload. GENERAL OFFICE PROCEDURES AND POLICIES Ethics The Counseling Services staff and trainees adhere to the ethical principles of the American Psychological Association, the National Association of Social Workers, the American Medical Association and/or the American Psychiatric Association depending upon professional discipline. The Web addresses for the ethics codes for these associations are: American Psychological Association National Association of Social Workers American Psychiatric Association American Medical Association http://www.apa.org/ethics http://www.nasw.org/ethics http://www.psych.org/ http://www.ama-assn.org/ama/pub/category/2512.html Confidentiality 1. All contact with clients and potential clients is treated as confidential. This includes a student’s status as a client and attendance at counseling sessions. 2. In accordance with NYS Mental Hygiene Law, no confidential information may be released to anyone without the written consent of the client unless one of the following conditions occurs: a. the client is in imminent danger of harm to self or others; b. the counselor has reason to suspect child abuse; or c. a judicial subpoena of records is issued. 3. At the start of the initial assessment or crisis appointment, the counselor should remind the client of the counselor’s mandatory child abuse reporter status. a. Trainees should consult with their supervisor or other senior staff member before reporting child abuse. b. If a decision to report is made, the counselor must complete the New York State Mandatory Report Form. This form is located in the forms bin in the front office. See Appendix U – Mandated Reporting of Child Abuse for appropriate hotline numbers and procedures. 4. All legal requests from attorneys or the courts received by individual staff members should be brought immediately to the attention of the Director prior to releasing any information. In the absence of the Director, notify the Associate Director. 26 5. Counseling Services staff, including trainees and support staff, should not discuss clients in the hallway or front office. 6. Trainees utilizing the computers are never to leave a workstation with client information accessible. 7. Titanium is not to be installed on or accessed from home computers. Counseling Services does not have a license for Titanium for home computers so it is illegal to install Titanium at home. Additionally, home installation is in violation of Counseling Services’ Policy, which states, “No confidential materials (client records, video or audio tapes) should be removed from the Counseling Services’ offices.” Since Titanium records are in effect client records it is not appropriate to be accessing them outside of Counseling Services. This policy is designed to protect the confidentiality of clients and reduce the risk/liability to individual counselors and to University at Buffalo Counseling Services. 8. Counselors and clients should be aware that email communication is not confidential (see Appendix V – Website Information about Email Confidentiality and Online Services). Maintaining Client Files 1. Contents of Student Records a. A separate client record is generated for any student who has contact with a counselor. b. A client record is not generated for a community member who calls or comes in for a consultation (e.g., concerned about another student, wants a referral, etc.). c. Client records typically contain: i. The forms that clients complete at initial assessment and/or crisis ii. Initial assessment summaries iii. Release of information and other consent forms iv. Copies of any letters sent to other professionals requesting or releasing such information v. Session notes vi. Miscellaneous notes (e.g. copies of email, phone contacts, consultations with or about the client) vii. Termination and/or transfer summary 2. File Storage a. All client initial assessment summaries, session notes, miscellaneous notes, letters, and termination summaries are stored in an electronic record-keeping database. b. Forms completed by clients at initial assessment, signed release forms, handwritten notes and letters, are kept in a paper file. c. When counselors pick up cases, they are to shred any unnecessary paperwork left in the file, such as printed or hand-written intake notes, notes already documented electronically, etc.. With few exceptions, the only paperwork that should be in the paper file is the initial assessment paperwork completed by the client, signed releases, and paperwork obtained from other service providers. c. Counselors and support staff must lock client folders in the appropriate front office file cabinets at the end of EVERY day. d. Consent for video and audio taping must be obtained prior to taping and the signed form placed in the client’s record. e. Video and audiotapes contain confidential material and must be stored in a locked cabinet. The tapes should not be kept in counselor mailboxes. f. All recordings made on the web cameras are stored on a password protected, encrypted data base and are erased frequently 27 g. No confidential materials (client records, video or audio tapes) should be removed from Counseling Services’ offices. h. Complete client folders are kept for seven years in our locked files. Summaries are then kept for an additional three years. i. The file room door and front office door are closed and locked when Counseling Services is officially closed for business. j. Counselors are not to re-file client files. Returned files are to be placed in the file basket so the front desk staff can re-file. It is critical that the files are put back in alphabetical order. The front desk staff is responsible for re-filing client charts. k. When removing a file from the front office, a red “out guide” must be filled out and put in the space the file previously occupied in the cabinet. Transferring Client Cases 1. If a client requests to be transferred to another counselor, the new counselor should discuss the reasons for the transfer to ascertain how the client believes a different counselor will better meet his or her needs. The client should be encouraged to discuss the reasons for the transfer with the previous counselor. If the client refuses to do so, this choice should be respected. The previous counselor should be informed that another counselor is now seeing the former client. 2. Client reassignment (due to schedule change, counselor leaving, etc.) should occur in weekly staff meeting. The client should be presented by the counselor as a reassignment with current availability and current therapeutic goals. Client reassignment should not be attempted via email with the staff. 3. Session limits should be discussed with transferred clients. 4. If a counselor is leaving the agency and, therefore, transferring clients to other counselors: a. This should be shared with clients with enough notice to allow clients to thoroughly discuss the impact and significance of this development. b. The departing counselor should discuss with each client her/his wants and needs regarding counseling in the future. Based on this discussion it may be determined that: (1) the client will terminate treatment now and return for additional counseling at a later time if necessary, or (2) the client needs to be seen without interruption, in which case it is the departing counselor’s responsibility to arrange for a smooth continuation of service. If the client is transferred to another counselor, the client will be given the name of a contact person who can facilitate the process of the transfer. The contact person will not necessarily assign him or herself as the new counselor. For trainees, in most cases their supervisor should serve as the contact person. c. All transfers not picked up by the departing counselor’s supervisor are to be presented at the clinical team meeting for reassignment. No Show/Cancellation Policy 1. When a student fails to show for two consecutive appointments or displays a tendency to fail to show after rescheduling appointments, the counselor should contact the student in a manner that the student has approved (email/letter/phone). The student will be asked to reschedule and keep the next appointment. The student is to be advised that if the counselor receives no response within one week of the date of contact or if the student fails to keep the next appointment, the counselor will close the student’s file, in which case the student must seek another initial assessment appointment in order to be re-established as a client and may be reassigned to another counselor. 28 2. If a student cancels a counseling appointment and indicates that he/she no longer intends to continue with counseling, the therapist should follow up to determine if a psychiatric appointment is scheduled and needs to be cancelled. Future psychiatric appointments should be cancelled if the student is no longer seeking concurrent counseling and the student should be reminded of our policy that they are eligible for psychiatric services only if they are concurrently engaged in counseling at Counseling Services. 3. When a prior client returns to treatment and more than three months have passed since her/his last appointment, s/he is not automatically assigned to her/his previous counselor. The previous counselor has the discretion to resume services or have the student complete another initial assessment and be reassigned. Support staff is to check Titanium before scheduling appointments to ensure the counselor allows the student to be scheduled with her/him. Termination or Transfer Summaries 1. Termination summaries should be written within one month of a student’s last appointment at Counseling Services. 2. Termination summaries should be written for all students that have been seen for an initial assessment, regardless of whether they attend subsequent sessions. For clients who fail to show for any appointments/sessions, a termination summary must be written documenting the steps taken to engage the client, such as number of phone calls, emails and all other attempts to contact. For such clients with lethality concerns, due diligence must be made to engage them in services and/or resources and those efforts must be reflected in the termination summary. 3. Transfer summaries should be written before the actual transfer, if at all possible. 4. It is recommended that a termination summary be created and saved on the same day as the last session. This will provide a visual reminder on your open notes section that the summary needs to be completed. Request for Release of Information 1. A release of information request must be submitted in writing by the client to his/her counselor requesting specific information be released and to whom. Information is never to be released without consent (see H drive under Forms). The signed release form must be an original; photocopies are not acceptable. 2. If the treating counselor no longer works at Counseling Services, the request for release of information should be given to the Director or Associate Director. 3. We release only initial assessments and termination summaries, not session (progress) notes. 4. A release does not need to be obtained to communicate relevant client information to Health Services Staff. When a student signs our consent form he or she is agreeing to allow us to contact HS on an as needed basis. Clinical judgment should be used to determine what should be shared to best assist the student. As a courtesy, the student should be informed of any intent to share information. Mailing Records and Communications of Confidential Information When we have a valid request for information accompanied by a signed release of information form, the following procedure is used to send (via campus mail or U.S. postal service) the requested information: 29 1. The name of the specific intended recipient should be written on the front of the envelope. 2. The envelope should be sealed. Interdepartmental envelopes are not to be used when sending confidential information to another campus recipient as these are easily opened without the recipient or sender knowing that the contents may have been viewed. 3. Write or stamp “CONFIDENTIAL” on the front of the envelope. Client Requests for His/Her Records 1. The Family Educational Rights and Privacy Act of 1974 gives students the right to see their “educational records,” which includes counseling records. 2. A release of information to self must be signed (see H drive under Forms). 3. Such requests will be responded to within 72 hours. 4. The counselor should discuss the request with the Director or Associate Director to get input on the course of action to be taken, to seek consultation, and to compile or summarize the necessary records. Request for Excuse From Class The UB Student Wellness Team (Health Services, Counseling Services, and Wellness Education Services) will not issue notes or excuses on a routine basis. To do so creates an undesirable climate for health care and disempowers students. Responsibility for class attendance and for completion of assignments rests primarily with the student, who assumes this responsibility by communicating directly with faculty. Health Services and Counseling Services will, with a release of information form signed by the student, verify the nature and extent of illness if a faculty member inquires. Request for Letters Supporting a Leave of Absence or Course Withdrawal 1. If at initial assessment, a student requests a letter supporting his or her withdrawal from class, the initial assessment counselor may verify the date of the appointment and current functioning only. The initial assessment counselor is not in a position to determine a student’s past ability to complete his or her schoolwork. 2. For a student who has been or is a client at Counseling Services, the counselor may write a letter commenting on the student’s ability to perform academic responsibilities based on actual knowledge of the student’s concerns and functioning. 3. If the counselor does not believe the student’s concerns are severe enough to impair academic functioning, this is to be discussed with the student prior to writing the requested letter and the student may elect not to request the letter from Counseling Services. 4. Trainees must always consult with their supervisors before releasing any information about a client. 5. Prior to releasing any information, the student must give written consent. Client Evaluation of Services 30 1. All students, excluding those receiving initial assessment, who come to counseling services in the 6th and 12th week of each semester will be asked to complete an anonymous client satisfaction survey (see H drive under Forms). The actual date of survey dissemination will be determined by the support staff and communicated to the Assistant Clinical Director. Only data collected within the data collection period will be included in the results. It is not acceptable to ask clients to complete the Satisfaction Survey after the data collection period. 2. The purpose of the survey is to identify trends, areas of strength, and issues to be worked on in the coming year. Clients will also be given a form letter by support staff that explains the purpose of the survey and gives completion instructions (see H drive under Forms). 3. One week prior to survey being distributed, support staff should ensure copies of surveys are available. One to two weeks prior to survey being distributed, counseling staff and trainees should discuss survey process with clients and allow for time prior to session for surveys to be completed. Signage will be posted in the waiting room one to two weeks prior to survey being distributed to alert clients to the upcoming survey week. 4. Students will return the surveys to the support staff prior to the day’s session. Support staff will then forward the surveys to the Director. At the end of each semester, the Director provides a written summary of client feedback to each counselor and to support staff. 5. During yearly evaluations with the Director, senior staff and support staff will review client evaluation forms. 6. Surveys will not be given to group clients; a separate survey will be made available. 7. At the end of each semester, group members will be given a group evaluation, which should be completed after the last session (see H drive under Forms). If a group member leaves a group prior to the end of the semester, the group leader will give the evaluation either immediately after the client’s last session or will send the evaluation via mail or email with the student’s permission. Supervision 1. All unlicensed psychologists, psychology interns, and social workers must be supervised by an appropriate licensed staff member. 2. Social work interns must be supervised by a licensed social worker. 3. Practicum students can be supervised by psychology interns, licensed social workers, unlicensed psychologists, or licensed psychologists. 4. When trainees facilitate a group alone or with another trainee, a senior staff member must be assigned as the supervisor. Senior Staff Peer Supervision Consultation Regular peer consultation can provide participants with important opportunities to obtain critical feedback on their work, to apply ethical standards to professional practice, to orient new professionals to the Counseling Services and to gain different perspectives on clinical and professional issues. Ideally, peer consultation involves relationships in which participants have neither the power nor the purpose to evaluate one another's performance. In reality, people including current supervisors and administrators may be members of the peer consultation group. So care should be taken to minimize power differences and cultivate a safe environment for all members to share. While it is acceptable to discuss ethical issues in peer 31 consultation, those ethical issues or potential legal issues that place the center at risk should be shared with the Director as well. Furthermore, policies and procedures of Counseling Services should guide professional behaviors and decisions at all times. New senior staff members are required to participate in a weekly peer consultation meeting their first year of employment. After the first year, senior staff can choose to participate or not participate in peer consultation. The peer consultation meetings may be preempted at the discretion of the Director in response to clinical services demands or other needs of the Center. Private Practice Guidelines 1. Counseling Services’ offices may not be used for private practice clients, consulting work, or any other efforts that are not part of the job description as a Counseling Services professional at the University. 2. Please do not give private practice clients Counseling Services’ telephone number. Make other arrangements to respond to private practice clients. 3. To avoid a conflict of interest, University at Buffalo students should not be seen privately by any staff member. Current students should be referred to community agencies or other private practitioners, if appropriate. 4. Case conference, small group supervision, and/or any other supervision at Counseling Services are for Counseling Services’ client concerns only. Private practice client concerns require consultation or supervision outside the agency. 5. There is an expectation that counselors and psychiatrists, while actually engaged in their private practice, may need to respond to emergencies concerning UB students. It is also understood that UB counselors and psychiatrists, while engaged in Counseling Services services, may need to respond to emergencies concerning private practice clients. 6. Advertising and public statements about a private practice should clearly distinguish it from the practitioner’s employment at UB. 7. Counselors and psychiatrists should make every effort to avoid dual relationships, which could impair their professional judgment or increase the risk of exploitation. Thus, hiring a current trainee to work in one’s private practice is a violation of this ethical principle. Research Policy 1. All research conducted here must be in keeping with Counseling Services’ policies. 2. To obtain approval to use Counseling Services staff, trainees, or clients as research participants, a potential researcher must submit a research proposal to the director that outlines the specific research questions, the sample, procedures, a consent form which includes possible negative effects of participating in the study, a rationale for the importance of the project, and evidence of approval by the UB Human Subjects Review Board or a similar board at another institution. 3. Please use this policy as a guideline when you email, post or distribute requests to any staff member, intern, and/or trainee. Any request that involves the following should be given to the director for review: a. Requests for operational procedures and service statistics. b. Requests to post and/or advertise questionnaires regarding students’ receipt of services at Counseling Services. 32 c. Requests that may jeopardize the integrity or anonymity of Counseling Services, staff, interns, trainees, and/or clients. 4. The director will use the following criteria to decide if the research can be conducted at Counseling Services: a. Will the research add to the body of knowledge in the field, especially in the area of working with college students or counselor training? b. Is the research well-designed and does it safeguard participants’ rights? c. Can the research be executed without causing undue burden or inconvenience to Counseling Services staff, trainees and clients? 5. The director has the right to suggest modifications to proposals and procedures to ensure a better fit with the agency and/or to enhance scholarship. 6. Approval by the director indicates that the research proposal meets agency policies. Each client and staff member has the right to decline to participate or to withdraw consent to participate at any time. However, the entire staff is expected to participate when data collection is a part of on-going internal assessment of service delivery and quality assurance. 7. Senior staff members may request from the director up to four hours per week each semester to engage in research and other scholarly activities. The requests should be a proposal which outlines how the time will be spent and how the data will be used (e.g. professional publication, presentations, improve agency clinical services delivery, or evaluation). The staff member will also be expected to present the results of their scholarly activities to the agency as a whole. Internal Use of Email 1. All staff and trainees must use the standard disclaimer about the nature of confidentiality of email communications. It is recommended that the disclaimer be attached to your automatic email signature. 2. Never use identifying client information (names) in internal emails. Always use students’ electronic record number. 3. All staff and trainees should follow the general recommendation of using email with clients primarily for scheduling/rescheduling purposes, and not for engaging in therapeutic exchanges. Trainees should consult with supervisors about how to best respond to emails from clients that relate to therapeutic issues. 4. All part-time trainees are required to set up a temporary email account to be used exclusively for their communication with UBCS clients, and which is to be closed at the conclusion of the training experience at UBCS. 5. Mass mailings should not be sent out to UBCS staff and trainees unless it is related to services or training issues. 6. Internal emails should not be forwarded to other staff and/or trainees without first consulting with the author of the original email as there may be important reasons emails are not widely distributed to everyone affiliated with UBCS. Staff Library 1. UBCS has a lending library with over 135 titles for staff and trainees to borrow. 33 2. A complete list of publications can be found on at H:\Counseling Services/Staff Development, which is updated annually. 3. To borrow a resource, use the same system in place for borrowing files: complete the File Removal card, place the card in the red “withdrawal” placeholder, and insert the placeholder where the book was previously located. 4. Books should be returned within a few days. 5. Books are never to be lent to students. Rather, chapters or exercises from books may be copied or information about books may be provided to students. 6. Suggestions for the purchase of other books or resources should be submitted to the Director. If you would like to donate books to the library, they must be approved by the Director prior to donation. Outreach Services 1. Counseling Services has an outreach program that brings psycho-educational information and interpersonal skill development opportunities to the student population. We have a particular commitment to bringing such services to those students who might not otherwise utilize Counseling Services. Currently, Counseling Services’ staff and trainees present on a broad spectrum of topics. 2. An archive of previous programs (e.g., outlines and handouts) is available as resource material for these seminars. These materials are available in hardcopy in the file cabinet drawers of the Outreach Materials locker in the back hall of 120 Richmond. They are also available online at: http://www.studentaffairs.buffalo.edu/shs/ccenter/materials.shtml. 3. When the campus community requests an outreach program, the Outreach Coordinator will bring the request to the attention of staff and trainees, usually via an email requesting coverage. Each staff member is then expected to indicate whether or not he or she can accommodate the request. A nonresponse is not acceptable. 4. Occasionally, a request for outreach services is made to a staff member other than the Outreach Coordinator. In these instances, the request should be forwarded to the Outreach Coordinator if the originally solicited staff member is unable to fulfill the request. Furthermore, the person making the request should be informed that the request has been forwarded and that the Outreach Coordinator is now the contact person. If the originally solicited staff member is able to provide the program, they need to inform the Outreach Coordinator of the date, time and location for his/her records. 5. All requests must go through the Outreach Coordinator so they may be tracked for statistical purposes and so staff members may receive credit for their participation. 6. Staff and trainees who are approached individually and contract to perform programming outside of the Coordinator’s knowledge are expected to inform the Coordinator so their program can be tracked. 7. Expectations for Provision of Outreach Programming: a) Senior staff and psychology interns are expected to facilitate a minimum of one outreach program per month. However, the actual number of programs may be higher or lower depending upon the needs of the campus. Staff and trainees may also be asked to have a consultative relationship with a campus office, department, or student group based on recommendations made by the Director of UBCS or the Outreach Coordinator, acting on behalf of the Director. 34 b) Staff members preparing to table an event (represent Counseling Services and provide Student Wellness Materials—no formal presentation required) are expected to gather their own materials (a variety of brochures reflecting the full range of UBCS services, including topic pamphlets, current group offerings, promotional items, the designated UBCS table drape and SWT team materials) prior to the day of the event. If assistance is needed, the staff member must make arrangements with the Outreach Coordinator or the Outreach Graduate Assistant, most preferably a minimum of three days prior to the event. Same day or “night before” requests for help may be denied based on the unavailability of the Outreach Coordinator or Outreach Graduate Assistant. c) If two staff members are sharing a workshop, event, or table hour, the more senior staff person is responsible for scheduling the outreach for both in Titanium. This is done by selecting the second drop-down box in the grid and adding the second person to the same hour. d) A variety of plastic tubs, crates, and boxes are available for use when transporting materials. A luggage dolly for assisting with cumbersome or heavy boxes is also available for use. The dolly is located next to the Outreach locker and crates are located under the student work stations. Please see the Outreach Coordinator or Outreach Grad Assistant if you need help locating materials. e) No formal evaluations are done for table or informational events. An approximate head count of participants is due to the Outreach Coordinator the next business day. f) Staff members also participate in numerous committees on campus and within Counseling Services. A complete list of committees can be found in Appendix W – List of Committees. g) Trainees attending an outreach as an observer should note the event as a “meeting” in Titanium, rather than as “outreach” or “training.” 8. Program Evaluations a) After an outreach program, it is MANDATORY that an evaluation form is given to all participants. These forms are submitted to the Outreach Coordinator who will compile this data. b) For ‘Food for Thought’ presentations, have participants complete copies of the Life and Learning Workshops Participant Evaluation Form and the Supplemental Program Evaluation Form. c) For other outreach presentations, have participants complete copies of the Program Evaluation Form. d) All forms are available on the H drive (Counseling Services, Outreach and Consultation Folder, Forms Folder) and in hardcopy form in the bottom drawer of the outreach files. e) Staff is expected to turn in evaluations the day of their program or the first day they return to 120 Richmond following their program. Staff is responsible for procuring the correct type of evaluation form for their program. If questions arise or assistance is needed with acquiring forms, please see the Outreach Coordinator or the Outreach Graduate Assistant, preferably three days prior to the program. f) Evaluations for all non-orientation programming is mandatory and failure to turn in completed evaluations will be reported to the Director for integration into performance appraisals. g) Senior staff or part-time staff members who perform an Outreach activity with a trainee are expected to complete the Evaluation of Competency in Outreach Programming. These forms are mandatory. h) Senior staff members conducting an outreach with a trainee complete the form evaluating the trainee’s performance and briefly meet after the program to process how the entire process went from planning to execution. Both parties sign the form. The form is due to the Outreach Coordinator within one week of the program. Failure to submit form impacts the ability of the Outreach Coordinator to effectively evaluate performance and will be noted on Performance Appraisals as neglect of training responsibilities. Consultation 1. Counseling Services’ staff is frequently called upon to provide consultation to campus groups, faculty, staff, and parents on a variety of issues. These conversations should be documented in the electronic database by clicking Open and selecting Crisis Intervention. This provides the option to 35 create a document for a general or non-client specific clinical consultation by creating a new record or allows clinicians to record the consultation note in a current or former client's record by selecting an existing client. a) At a minimum, the following information should be documented whenever possible: the name of the consultee, contact information for the consultee, the nature of the concerns discussed, actions recommended and/or taken, and any other individuals involved in responding to the consultee’s concerns. If the consultation is in regards to a third party, the name of this person of concern should also be noted if the consultee is willing to provide. b) If someone requests a consultation outside of crisis hours, they will be informed that a counselor will get back to them later that day (during a crisis hour). If they indicate more urgency and cannot wait for a return call, the call will be forwarded to a counselor who is available. A typical mental health consultation involves an individual requesting mental health/counseling related information for themselves or for someone else that they are concerned about. This may happen through phone or in-person contacts. Callers who are interested in things such as interviewing someone for a class or learning about training opportunities at UBCS, etc. are not urgent. It is the responsibility of the crisis counselor who received the call to follow-up with the caller. Such calls should not be passed along to the next crisis counselor. Only urgent matters should be passed along to the next crisis counselor to respond. 2. When providing a consultation, please keep in mind the following: a) Think of the consultee as a client: you need to accurately assess their needs (e.g. information, reassurance, support, referral) and provide appropriate responses to best meet their needs within the bounds of what we can ethically and responsibly offer. Consider what you can do to help him/her feel better about the situation and what steps can be identified to help him/her or the person they are concerned about. b) Make clear to the consultee that you cannot give out information about a specific student without a signed release of information due to the legal mandate for confidentiality. However, you can listen to any information the consultee wishes to convey, and talk to him/her generally about how one could go about addressing similar concerns, whether it be about themselves or someone else that they are worried about. It is also appropriate to sympathize with the consultee’s frustration about the limits of what we can disclose. c) If the consultee is concerned about the immediate safety of a UB student, consultation should occur with a supervisor or the Counseling Services’ Director before taking steps that might breach the student’s right to confidentiality. In the case of phone consultations, it is acceptable to take the consultee’s number and call back after consulting with others on staff. If the consultation is in person, it is appropriate to ask the consultee to wait in your office while you consult with the Director or another senior staff member. d) If appropriate, review with the consultee how a UB student accesses counseling services through either an initial assessment appointment or crisis appointment, as appropriate. If the student is going to come to Counseling Services’ immediately, inform the support staff. The support staff will inform the current crisis or initial assessment counselor. e) Whenever possible, pertinent information related to a student should be communicated to the crisis counselor verbally or in a note, so that s/he has the information before the student arrives. i) If the consultee is concerned about the imminent safety of a student who resides off campus, Crisis Services ((716) 834-3131) can provide immediate in-home mental health and lethality assessments. Crisis Services can also facilitate a student’s transportation to CPEP for evaluation. ii) Counseling Services does not contact students to encourage them to engage in counseling or “check-in” with students to make sure they are okay. If a parent or faculty member is concerned that the student is at imminent risk of harm, recommend that they call Campus Police at 645-2222 (on campus students) or 911 (off campus students). iii) If a student presents to a counselor as having been the victim of a crime on campus, but wishes to remain anonymous, a Proxy Report should be completed and submitted to 36 University Police. This report can be found at http://www.studentaffairs.buffalo.edu/public-safety/silentwitness.shtml. iv) If a student is a victim of a sexual assault on campus, Counseling Services has specific procedures that are to be followed (see Appendix X – Sexual Assault Response Guidelines). 3) Counseling Services adheres to the University at Buffalo Sexual Harassment Policy and all staff and trainees are expected to abide by this and all policies (see Appendix Y – UB’s Sexual Harassment Policy). Training Programs There are minimum expectations of all trainees based on agency policy and trainee status within the agency. Levels of Trainees First-Year Practicum Students These are first year students in the Counseling Psychology program. They may choose to complete a practicum at UBCS, which entails attending a 90-minute seminar for 3-4 weeks at the end of the Fall semester and a 12-hour weekly clinical commitment during the Spring semester. The Practicum Coordinator oversees their training activities. Advanced Psychology Practicum Students/Externs These are Counseling or Clinical Psychology students who, after their first year of graduate school or another clinically oriented practicum experience, elect to train at a site that focuses on working within a university setting. Hours are determined in conjunction with their department and Counseling Services, but are typically 16-20 hours per week for both fall & spring semesters. The Practicum Coordinator oversees their training activities. Predoctoral Psychology Interns The APA-accredited pre-doctoral internship in professional psychology (APA Office of Program Consultation and Accreditation, 750 First St. NE, Washington, DC 200002-4242, 202-236-5979, http://www.apa.org/ed/accredidation/homepag.html) is a full-time, year-long, 2000 hour training placement for doctoral level graduate students in Counseling or Clinical Psychology. There are three interns positions each year. All psychology interns are supervised by licensed psychologists. The training program adheres to APA accreditation standards. Intern selection procedures are in concordance with APPIC policy and procedures, and the program participates in the APPIC internship match process. The Training Director oversees the internship training program, the overall progress of interns, and intern selection processes. More information about the internship can be accessed on the web: http://ub-counseling.buffalo.edu/internship.shtml. Social Work Interns These are social work students in their last year of the Masters in Social Work program. They spend either 16 or 24 hours per week at Counseling Services. The Social Work Internship Coordinator oversees their training activities. Requirements Specific training requirements and experiences are coordinated by the Training Director for predoctoral interns, by the Social Work Internship Coordinator for Social Work interns, and by the Practicum 37 Coordinator for first year and advanced practicum students. Such requirements and experiences include, but are not limited to, staff meetings, clinical meetings, case presentations, group co-facilitation, individual counseling, supervision, initial assessment, record keeping, outreach, and programming. Trainee Eligibility Students are expected to be in “good academic standing” as defined by their department during their affiliation with Counseling Services. If a student is no longer in good standing in his/her program, the affiliation is terminated. Graduate students interested in obtaining a clinical training placement or clinical graduate assistantship at UBCS are not eligible if they have previously utilized services at UBCS as this may have implications for the provision of training and supervision, and may contribute to a difficult dual relationship experience for such students. These students would be encouraged to explore alternate training and/or assistantship experiences as arranged by their graduate department. Evaluation of Trainees Counseling Services maintains on-going evaluations of all trainees. Copies of evaluation forms are located on the Counseling Services server or in the relevant training manuals. Coordination of Training The Training Director and coordinators of the Social Work, First Year Practicum, Advanced Practicum/ Extern programs are standing members of the Training Committee. The chair and members of this committee are assigned by the Director at the beginning of each semester. The Training Director and coordinators work together to ensure efficient service delivery by trainees and trainee orientation to the agency, and serve as liaisons with academic departments and advocate for trainees. This type of collaboration among the coordinators models inclusiveness with regard to differing counseling disciplines and cooperation among the training groups. OFFICE OPERATIONS Office Hours During the academic year, Counseling Services’ hours are Monday, Tuesday, and Friday from 8:30 a.m. to 5:00 p.m., and Wednesday and Thursday from 8:30 a.m. to 7:00 p.m. The main office for Counseling Services is 120 Richmond Quad on the North Campus. There is a satellite office in Michael Hall (Health Services) on the South Campus. There are always at least two counselors scheduled to work when the office is open. One of these counselors must be a senior staff member. At Michael Hall, a trainee must never be scheduled to work alone. We do not see clients at the office during hours when the office is not officially open. If a client is unavailable during our business hours, then s/he has two options: the person can adjust his/her schedule to accommodate an appointment during business hours or the person can be referred to a resource in the community. Minimum Workload Expectations 1. Rarely will two staff members have an identical work schedule due to different administrative and supervisory responsibilities (see Appendix Z – UBCS Organizational Chart). 38 2. Each semester counselors submit a contract for work that must be approved by the Director. Trainees submit contracts which are approved by their respective program coordinator. 3. All senior staff and psychology interns are expected to attend the clinical meeting, the staff meeting, and professional development training. 4. All senior staff is expected to work one evening a week. Staff Meetings 1. Clinical Meetings take place every Tuesday from 8:30-9:30 a.m. All staff and trainees are expected to attend this meeting. At Clinical Meetings, cases that need to be assigned are presented first. Among those cases, students who need to be seen immediately, followed by those who have been waiting the longest for service, are to be presented first. Trainee consultation/case presentation is the second highest priority, followed by staff consultation. 2. Staff meetings are on Tuesdays from 9:30-10:30 a.m. Senior staff-only meetings alternate with Open-staff meetings (staff plus psychology interns). 3. Once a month, the Staff Meeting is cancelled and there is a 1.5 hour Professional Development Meeting. 4. Group supervision for psychology interns takes place weekly for 1.5 hours. The Group Coordinator facilitates this meeting. 5. Staff and trainees’ who miss a meeting are responsible for obtaining the information that was presented. 6. Trainees’ level of training is shared with the clinical team in clinical meetings. Trainees’ level of training is determined with the supervisor using the Client Severity Scale (see Appendix E – Guidelines for Case Disposition and Counselor Assignments). This informs decisions about case assignment. It is the expectation that ongoing discussions take place between supervisor/supervisee regarding the types of cases that the supervisee can pick up. It is assumed this level will change as appropriate. Staff Schedules 1. Senior staff counselors are expected to work 35 hours per week. 2. At the beginning of each semester, the Associate Director will ask staff members to complete a weekly master schedule on which counselors and trainees’ work hours, standing meetings, counseling groups, initial assessments, crisis and supervision times are recorded. If additional coverage is needed on certain days, the Associate Director may ask the staff to adjust their proposed schedule accordingly. 3. Once the Associate Director approves a work schedule, the staff and trainees are expected to maintain an up-to-date schedule on the computer scheduling system. Please include all days that you will not be in the office and times when you are not normally scheduled to be in the office though the office is open. Because of the expanded hours on Wednesdays and Thursdays, not everyone will work from 8:30-5:00 each day. The Associate Director will also create Michael Hall schedules. 39 4. Practicum students and social work interns do not have assigned offices. It is the trainees’ responsibility to reserve a room when scheduling clients. A room should not be reserved to complete paperwork; computers are available for paperwork. Senior Staff and psychology interns will be asked to provide the Practicum Coordinator and Social Work Coordinator with times when their offices will be available for practicum students and social work interns to use as well. Staff and trainees scheduled at Michael Hall will have assigned offices. 5. If you are going to leave the office during a time that you are scheduled to work, the following must occur: the Director or Assistant Director must approve and the counselor must have checked to ensure there are at least two other counselors (one of them senior staff) scheduled to work. Counselors must inform co-workers of their absence so co-workers know who is available for backup. Do not assume that because others are in their office that it is “safe” to leave. Vacation and Sick Leave 1. Requests for vacation and anticipated sick leave (for example, an operation) should be made in writing to the Director, preferably two weeks in advance (see H drive under Forms). 2. Vacation and sick leave can only be requested for a minimum of 0.25 days or two hours. 3. A sick leave request of more than 4 hours must be accompanied by an explanation of why so much time is needed. A doctor’s note may be requested if sick leave must exceed 4 hours. Sick leave may not be used in lieu of vacation time. 4. If counselors need to be out of the office for an hour or less, they do not need to complete a Request for Leave form. In such cases, permission must be obtained from the Director or Associate Director. Counselors must ensure that there is adequate coverage, notify staff of their absence, and make the appropriate notation in Titanium to show they are out of the office. 5. During Winter Break (usually the week before and the week of December 25), regular staff will be required to work 30 hours per week (six hours per day). If requesting time off during this period, each work day is the equivalent of one regular work day. For example, a request of one vacation day during this period (one six-hour day) will count as one used vacation day (one eight-hour day); a request of three compensatory hours off during this period (one-half of a six-hour day) will count as one half-day or four hours of compensatory time used, and so on. 6. A Request for Leave form must be submitted for absences of more than one hour, including unplanned illness. This includes arriving to work more than one hour late or any other unapproved absences of more than one hour. 7. Practicum students/externs and Social Work interns receive time off in accordance with the University at Buffalo academic calendar. 8. When calling to notify Counseling Services of the need to arrive to work late, please provide the Director with a reason for the tardiness. This may be done via the front desk staff or directly through phone, email, or voicemail. Others will not be informed of the reason for your tardiness unless you explicitly direct that the information be shared. 9. Early departures or absences from the office for an extended period of time during the work day need to be reflected in Titanium and, in most cases, will require approval by the Director. This ensures that others know who is available for consultation, to provide back up, or to respond to a crisis, and applies regardless of work location (Richmond or Michael Hall). 40 10. Counselors who are unexpectedly absent due to illness or other unforeseeable circumstances are responsible for determining who covered the initial assessment appointments during his/her absence and then re-assigning a corresponding number of that counselor’s future initial assessments to his/her schedule. If the counselor cannot do the assessment on the same day and time as the person who covered does his/her initial assessments, the counselor can instead remove unfilled initial assessments from the other counselor’s schedule and add the corresponding number of initial assessments to his/her schedule. The counselor who was out must alert the counselor who covered the initial assessments of these changes to his/her schedule. Compensatory Time Senior staff and psychology interns may accrue compensatory time under the following conditions: 1. Eight hours of compensatory time will be given for every week spent on call, whether you have responded to a crisis situation or not. 2. Compensatory time may be given when a counselor has facilitated a number of programs above and beyond that expected (including weekends and evenings). 3. Compensatory time will not be given for staying late to complete paperwork. 4. Compensatory time will not be given for working extra hours in a given week so you can work fewer hours in a subsequent week. 5. From time to time, counselors and psychology interns may be asked to come in early or leave late because of some staff event that affects us all, such a staff training day or a candidate interviewing. In general, you will not be given comp time for such schedule changes, nor should you be making adjustments in your Titanium schedule to make up the difference. It is the nature of this job that sometimes you will work more than 40 hours per week. Similarly, there may be occasions when the office closes early or we have a shorter work week, in which case employees are not penalized for hours not worked so essentially get some of this time back (for example, the Wednesday before Thanksgiving or during winter break time). 6. Procedures for requesting and using compensatory time: a. Requests for compensatory time must be made to the director in writing. Please use the Request for Leave Form (see H drive under Forms). b. Requests for compensatory time must be submitted two weeks prior to the dates you wish to take off. c. The counselor must submit the dates, times, and reasons the extra work incurred. d. Compensatory time must be taken in increments of half or full days (four [4] or eight [8] hours, respectively). e. Compensatory time must be taken by May 31st of the academic year in which it was accrued. f. You may not request compensatory time in anticipation of an on-call week or program. You may only request compensatory time after you have had an on-call week or worked above and beyond normal hours. g. For attendance purposes, the staff member will be considered present for work on the days that compensatory time is taken. h. The Director reserves the right to grant requests based on the needs of the office and/or the perception that the counselor has in fact performed “extra work.” Requests for “One Time” Schedule Adjustments To request a one-time schedule adjustment, please follow the following process and guidelines: 41 1. First, check to see if there will be enough coverage if you were to be granted the request for an adjustment to your schedule. This includes a visual check of Titanium, as well as emailing the clinicians who are scheduled to be in the office that day to ensure they will be in the office and that trainees are not left alone at Michael Hall. There must always be a senior staff person and at least one other counselor/trainee in the building. 2. Then, submit a request for leave to the Director in which you inform her/him that coverage is adequate at the time you are requesting off. It is crucial that you assess coverage as the Director and/or Associate Director will rely on your assessment. 3. Minor changes to schedule, such as leaving late or coming in early, do not constitute justification for a schedule adjustment. As professional employees, such minor deviations are within the scope of your work. 4. Compensatory time is intended to address situations in which you have worked an excessive amount of overtime. You may request compensatory time in such circumstances, noting the additional hours worked and why. Recognition may not equate to a one-for-one credit for hours worked. Please refer to the Compensatory Time section of this manual for more details. 5. If you frequently need to make minor adjustments to your schedule, Counseling Services and you may be best served by contacting the Director to discuss work contract changes or the Associate Director to discuss work schedule changes. Time Sheets 1. Staff receives vacation and sick time benefits in accordance with University policy, which is printed on the back of time sheets. 2. The amount of time off counted against benefit time (e.g., vacation, sick and compensatory time) is calculated as follows: If an employee is scheduled to work 4 hours on Monday and requests Monday off for vacation, one full day of vacation time will be counted against the employee’s vacation time accrual. Likewise, if an employee is scheduled to work 10 hours on Thursday and calls in sick on Thursday, one full day of sick time will be counted against the employee’s sick time accrual. 3. It is preferred that staff request time off that has already been earned. For example, asking for October 1st off in anticipation of getting the floating holiday for Columbus Day on October 16 is not the preferred scenario. 4. Senior staff and predoctoral psychology interns submit time sheets monthly to the support staff. The Director will then sign off on them. 5. Social Work interns submit time sheets weekly to their individual supervisors. 6. Advanced Practicum Students/Externs submit timesheets weekly to their coordinator. 7. When taking an unplanned leave, the time must be recorded accurately. For example, if a counselor calls in sick, the time must be recorded as “sick time” on the time sheet. Changes to how time is charged (e.g., in the event the counselor has run out of sick time) must be requested at the time the leave is taken and must be approved by the Director or Associate Director. 42 8. Both the top and bottom portions of the timesheet must be completed each pay period. 9. If you are granted compensatory time, which must have been formally requested via a Request for Leave form, you must enter this as “Vacation Time” in Titanium and add a note indicting it is “Compensatory Time.” Note that compensatory time is not recorded on the time sheet. 10. Jury duty is to be recorded on the time sheet and a copy of the subpoena for jury duty must be attached to the time sheet. 11. Please check the math on your time sheet before submitting for approval. Staff Initial Assessment and Walk-In Crisis Coverage Responsibilities 1. The staff will sign up for initial assessments and walk-in crisis hours at the start of each semester. 2. There will be at least one initial assessment offered hourly from 9 a.m. to 4 p.m. on Monday, Tuesday and Friday and from 9 a.m. to 6 p.m. on Wednesday and Thursday. Initial Assessments are also offered at Michael Hall by staff who are housed there. 3. Psychologists, social workers, and predoctoral interns are expected to do three initial assessments per week. Social work interns and advance practicum students/externs do two initial assessments per week. The clinically-focused Graduate Assistants do one initial assessment per week. Other trainees do initial assessments based on an assessment of their readiness to do so. 4. During times of high service demand, the Associate Director may ask that additional initial assessment hours be offered at specific times. The Associate Director is responsible for having these times added to the electronic scheduling system. 5. A staff member must find someone to cover crisis hours when he or she will be away from the office during scheduled times. a. If the designated crisis counselor arranges for another counselor to cover his/her crisis hour, the originally designated crisis counselor must ensure the crisis hour is entered into the other counselor’s schedule. b. In the event that there appears to be no crisis coverage, the front desk staff will first email the person who normally covers the crisis hour at that time. If s/he is out of the office or not reachable, the decision tree (see Appendix O – Crisis Client Procedures) will be used, thus eliminating the need for the front desk staff to send emails regarding who is covering a crisis hour. Staff Grievance Procedures Due process procedures are outlined in Appendix AA – Due Process Procedures for Addressing Staff Grievances. Addressing Staff Member Impairment The procedures established in Appendix BB – Due Process Procedures for Addressing Staff Impairment should be followed when all traditional supervision practices have been utilized. Extended Counselor Absence Coverage When a staff member will be out of the office for an extended period of time, such as for family leave or convalescence, arrangements must be made for coverage of clinical and supervisory responsibilities. 43 Professional Development 1. Each year, full time staff (senior staff, support staff, and psychology interns) will be allowed up to six days of professional development during the fiscal year (July 1- June 30). Half-time senior staff employees will be allowed up to three days of professional development. Typically, professional development takes the form of attending conferences, workshops, seminars, taking job-relevant academic coursework, or other types of formalized training activities. You cannot “rollover” days into the new fiscal year. Therefore any days used after June 30th will be subtracted from the new fiscal year. Exception: Psych interns are exempt since they are not here for most of the new fiscal year. 2. Counselors serving in a leadership role in a professional organization related to psychology, social work or student affairs will be granted an extra two days for a total of eight professional development days. Counselors presenting at a professional conference or helping to organize a professional conference are granted one extra professional development day. 3. Three of the six days of professional development time can be used for the following: dissertation proposals/defenses (senior staff and interns), studying for and/or taking licensing or certification exams (senior staff), or job interviews (interns). 4. Each year, funds for professional development will be based on budget considerations. Staff members who present at a professional conference or serve in a leadership role during a professional conference/annual meeting will be given $100. 5. If a senior staff member must attend a particular conference due to his or her administrative role or as required by the director, the expenses will not be deducted from his or her travel allowance. Occasionally the director may provide additional pay and time for staff to attend special professional events; these events will not deduct time from the individual staff member’s allowance. 6. Professional development money must be spent during the fiscal year ending June 30th or else these funds will be forfeited. 7. A request for leave form (see H drive under Forms) must be submitted to request time away from the office to attend professional development training or conferences. 8. If additional professional development time beyond the six days is requested, vacation or comp time must be used to cover the time. Sick leave cannot be used as professional development time. 9. Airline ticket purchases for professional development activities must be purchased through the University travel agent. Snow Days 1. According to University policy, “When winter conditions become so severe that the University cannot operate effectively, an announcement to that effect will be made over local radio stations.” The initial announcement will be made by 6 a.m. if at all possible and will be repeated frequently. 2. The University will inform staff if they are to be given time off for a snow day or if benefit time must be used. Office Equipment 44 1. Furniture and equipment should not be removed from any office without approval. Each item is inventoried and accurate records must be kept of its location. 2. Staff must always consult with the Director prior to discarding any furniture or equipment. Support staff will arrange for proper disposal. 3. The laptop and projector must be signed out. Please check the sign out sheet in the “Bird” drawer in the file room for the availability of this equipment. Dealing with the Media All requests for interviews or “expert opinion” that come from non-UB media outlets should be referred to the Office of the Vice President of Student Affairs. The Vice President typically serves as the media spokesperson for Student Affairs. Counseling Services staff and any trainee who claims affiliation with Counseling Services must have the Vice President’s permission before speaking to non-UB media. Requests for Informational Interviews Counseling Services generally honors requests for informational interviews by UB students. This may be suspended if the demand becomes burdensome during a given semester. Requests for informational interviews received while acting as the crisis counselor should be addressed at that time. However, a bona fide crisis situation takes precedence over such requests or calls. Professional Behavior Dress Code Counseling Services has a high degree of visibility in the community by virtue of our mission. It is expected that all staff and trainees dress appropriately in casual business attire. Keep in mind that at times you may be in the office solely to complete paper work. However, visitors to the office will perceive you as a member of the staff. Therefore, always dress appropriately for a professional setting. Appropriate Use of Email University email accounts are not to be used for personal reasons. If you receive junk mail, chain letters, jokes, etc., delete them and do not reply or forward. Non-authorized “mass emails” are prohibited. Appropriate Use of Cell Phones Cell phones are to be put in silence/vibrate mode upon entering Counseling Services (Richmond and Michael Hall). Please direct personal contacts (e.g., family, significant others) to call Counseling Services at 716-645-2720 to reach you in the event of an emergency. During lunch, cell phones may be used. However, to avoid disrupting others such conversations should be held in an interview room or outside. Cell phones should not be used in any public areas, only behind closed doors. Front Desk Protocol 1. If you leave a client file at the front desk, place the file front side down so people standing near the desk cannot read it. 45 2. If you escort a client to the desk to schedule an appointment, please have him/her stand in front of the window in the waiting room area. This prevents the client from having a view of any confidential information. 3. Please do not discuss the details of clients’ cases or mention names when students are at the desk or in the waiting area. 4. Front desk staff may not always be able to provide you with information about a client over the phone, as another student may be standing nearby. If client information is needed immediately, this should be conveyed to front desk staff so they may accommodate. Computer Shortcuts Short cuts to important documents, such as the Hospital Transport log, the On-call log, the Cleary Act log and Group Openings, are available at H:\Counseling Services\Shortcuts. When setting up your computer, it is recommended that you include these shortcuts and shortcuts to any documents you will access regularly (such as the P&P Manual) to aid in finding these items readily. Duress Alarm Procedures Duress alarms are located in each counselor’s office, the group room, and the interview rooms, in a location easily accessed during appointments. It is important you familiarize yourself with the location of the alarm whenever using a new office. If the alarm is pressed Campus Police will be immediately notified and will respond. IMPORTANT: Under no circumstances should anyone working at CS attempt to physically intervene with a student who might be dangerous. We are not trained for such actions, and we are likely to make the situation worse if we do try to intervene. The Duress Alarm notifies the police; it is their responsibility to make the direct intervention. 1. When to use the Duress Alarm: whenever you believe immediate police intervention is necessary a) your physical safety is in danger b) your client has already harmed himself c) you overhear or otherwise learn that someone else on site is in danger/at risk d) in the event of a medical emergency (e.g., collapse, heart attack, seizure, etc) e) a potentially dangerous person takes flight 2. Roles and Responsibilities When An Alarm Is Triggered a) Front Desk i) Once the duress alarm is triggered, the Police will be on their way. You must be ready for their arrival with the following information: (1) Which room? (2) Name of Client? (3) Make sure that the entry to the unit is clear (instruct people to move out of the doorway etc.) ii) Contact University Police by phone to verify that the Duress Alarm has been received and inform the Dispatcher of any pertinent information: Screams or other noises coming from the area, Gunshots, Injuries, Direction of Flight etc. iii) Notify all of the following, whether or not they are on-site: Sharon, David, Sung, Liz. Inform them which office/who has sounded the alarm. iv) If the above people are not available, use flow chart to notify available staff member. Carry out any other instructions given to you by the staff. 46 b) Staff i) The senior-most staff person who is on-site, or his/her on-site designee, will be in charge of the incident, until arrival of the Police. ii) Someone must contact the office in question by phone to assess the situation, if possible. Please be aware that it is possible that the counselor will not be able to answer the phone. Yes/No questions to ask: (1) “Is there a weapon involved?” (2) “Is anyone injured” (3) “Do you want a staff member to enter now” (4) “Should we wait for police.” (5) Entering the room? (a) The senior-most staff person who is on-site will make the decision to enter or not to enter based on the totality of the situation, remembering that CS staff members are not trained for intervention with potentially violent individuals, and they may make the situation worse if they do try to intervene in those circumstances. If there is no contact made with the counselor in the room NO ONE WILL ENTER THE ROOM UNTIL THE POLICE ARRIVE. If there are any indications of violence occurring in the room then the rest of the unit will be evacuated. iii) A staff member should look up the client in Titanium to see if there is any instructions or crisis plans in place. If there are specific instructions or crisis plans in place, that information must be available to the Police officers responding. iv) Someone needs to be at the front door to direct the police, and provide additional information if we have any. Must have basic information for the arriving police officers: Which room? Name of Client? Also the Front Desk Personnel should make sure that the entry to the unit is clear (instruct people to move out of the doorway etc.) v) Two staff members should stand by the door of the office in distress in case they are needed. c) Trainees and others i) Be aware of the location of the duress alarm in the office/interview room you are using. The duress alarms in the interview rooms are in the same spot: clipped to the tray on the table. ii) Trainees should not be expected to intervene in these situations. iii) The hallways should be kept clear. 3. After the Event a) Debriefing with all those involved should occur as needed as soon as possible following the event. Additional debriefing with entire CS staff should also be considered. University Police Supervisory staff from the incident should probably be included in this de-briefing. (Consider having UB’s EAP or Buff State Counseling Center do the debriefing rather than doing it ourselves since we were involved). b) Accurate information should be distributed to all CS personnel as soon as possible. Control of rumor and misinformation is important. c) An incident review should be conducted by the Administrative Team (Sharon, David, Sung, Liz). 4. Additional Things To Consider a) Keep your office door UNLOCKED when with a client. Police officers need to be able to gain access to your room. b) There is a 2-second delay before the duress alarm is activated. This is to minimize accidental presses of the button. You need to hold the button down for two seconds before it is activated. c) If you are using an interview room, or someone’s office other than your own, it is critical that you familiarize yourself with the office you will be using and the location of the duress alarm. d) Tips for dealing with potentially dangerous person: i) put or keep something between you and the individual ii) try to position yourself closest to the door 47 iii) if the potentially violent person attempts to flee, do not put yourself in harm’s way; get a description and direction of travel and inform the Police. Building Evacuation Plan A building evacuation plan is in place. Please see Appendix CC - Building Evacuation Plan for details Web Cams Web cams will be used to record sessions for those counselors required to do so. See H:\Counseling Services\WebCams for the following instructional documents: Updated First Time Webcam Setup (2), Setting Permissions, Recording Video, and Watching Recorded Videos. 48 APPENDICES 49 APPENDIX A: TREATMENT OF MINORS POLICY STATEMENT AND GUIDELINES New York State law requires us to obtain parental consent for mental health treatment of a MINOR student when parental consent is readily available and not deemed to be detrimental to the student's well being. I. Definition: Minor = student under the age of 18, not married, not the parent of a child not legally emancipated not on voluntary status as defined in Section 9.13 of the mental Hygiene Law II. The Mental Health Hygiene Law of New York authorizes the provision of outpatient mental health services to a minor under the following circumstances: A. Minor is knowing and voluntarily seeking the counseling services; B. Provision of the services is clinically indicated and necessary to the minor's well being; and one or more of the following pertains: 1. Parent or guardian is not reasonably available. 2. Seeking parental or guardian consent or involvement would have a detrimental effect on the course of outpatient treatment. 3. Parental consent has been denied and treatment is necessary and in the best interests of the minor. III. Procedure for Service Provision: A. At the time of the initial assessment/consultation the CS staff must verify the student's age. A person under the age of eighteen, who is voluntarily seeking outpatient services, may be provided with an initial consultation (in contrast to ongoing therapy) without parental or guardian consent, as the law pertains to treatment, not assessment. B. Following the initial assessment/consultation, the initial assessment counselor must either 1. Initiate a process of obtaining parental or guardian consent, or 2. Determine that the student may receive services without parental/guardian consent. If this determination is made, the treating staff member shall fully document his or her determinations in the minor's clinical record, along with the minor's written, signed statement that s/he is seeking services voluntarily. C. The Director of Counseling Services is to be notified by the initial assessment counselor of any students below the age of eighteen who has received an initial assessment session. D. Students who are legal minors may be referred to a consulting staff psychiatrist for further assessment or evaluation. However, psychotropic medication will not be prescribed to legal minors without written consent of a parent or legal guardian. In an emergency, we assume that we have the permission of parents to treat as necessary. However, every effort to reach parents of a minor as soon as possible must be made. (Guidelines are derived from the University Counseling Center at SUNY/Stony Brook, who in turn utilized the Mental Health Hygiene Law Section 33.21 regarding non-emergency outpatient treatment and advice of University Counsel dated March 9, 1995.) 50 APPENDIX B: CASE AUDIT FORM – SENIOR STAFF FORM UB Counseling Services Quality Improvement Program Case Audit Form: Senior Staff Version number: Instructions: Check each box as: Adequate Inadequate Not Applicable N/A Date: Titanium Provider: A) Consent for treatment signed by client and witnessed. B) Initial assessment summary written within a week. C) Lethality section completed on the initial assessment summary. D) Initial assessment reviewed & locked within two weeks of assessment date. E) Conceptualization and treatment plan documented by 3rd session F) All session notes are written within 3 business days G) Consultations are appropriately documented. H) Out-of-session contact documented I) Hard copy of forms is in chart and appropriately signed: release of information, couples policy, group policy, verification of mandated assessment, consent for taping etc… J) Termination summary completed within one month of last contact K) Termination summary locked by the supervisor within two weeks of being completed by the supervisee. L) Has not exceeded session limits Comments (use other side of paper if necessary): Evaluator: 51 APPENDIX C: CASE AUDIT FORM – SUPPORT STAFF UB Counseling Services Quality Improvement Committee Case Audit Form: Support Staff Procedures for completing Support Staff Audits Pull 10 files randomly and complete general support staff audit on the reverse side of this form. All support staff will get a copy of the general support staff audit. It makes sense to do this side first, make copies for all support staff and then complete individual audits on reverse side. Go to front desk log to identify 5 clients with data entry from each support staff (including each student worker). For each client, review that the purple sheet has been entered correctly. Information from the purple sheet will be found in Ti in contact information and the client information data form. Document any specific problematic issues as they are identified. Instructions: Check each box as: Complete Incomplete Not Applicable N/A Client #: Name on chart is accurate (No typos) Records are in the appropriate section of the file cabinet and in alphabetical order Previous HARD COPY treatment record/ chart has been combined with new record Consent for treatment signed by client and witnessed No loose papers such as phone messages or sticky notes placed in chart by support staff Unused forms removed from file before filing Comments: Audit Date: Auditor: 52 Name of Support Staff: Client # Contact Information is accurate and complete Client Information Data Form is accurate and complete Comments: 53 APPENDIX D: RIGHTS, PRIVACY, RESPONSIBILITIES AND CONSENT TO TREATMENT COUNSELING SERVICE Rights, Privacy, Responsibilities Student Wellness Team 120 Richmond Quad 716.645.2720 http://ub-counseling.buffalo.edu and Consent to Treatment I. YOUR RIGHTS II. YOUR PRIVACY 1. Eligibility Counseling services are available to currently enrolled, full- and part-time UB students. A non-UB student may only be seen in the context of couples therapy with a UB student. 1. Privacy Information shared by you will be kept in strict confidence. Counseling Services creates and maintains records describing your physical and mental health history, symptoms, diagnoses, treatment, and plans for future care or treatment. Most disclosures of your private information would require your written permission. Because the professional staff of the Student Wellness Team (Counseling Services, Health Services, Wellness Education Services) operate as a team, we may confer with each other as professionally necessary to provide the best possible service to you. If your counselor audio or video tapes sessions, your written consent will be obtained. Taping is done so that your counselor can review sessions to aid the counseling process. The tapes are confidential and erased after use. You have the right to refuse to be taped. 2. Services Available At the end of your initial assessment if further services are indicated, the counselor may recommend group, individual, or couples counseling, suggest further evaluation, or refer you to other services on- or off-campus. Occasionally, some students find that this initial consultation meets their needs and require no further services. We offer a range of services, including group counseling, short-term individual and couples counseling, and psychiatric care. You have the right to refuse diagnostic or treatment services. Your counselor may be a social worker, a psychologist, a psychiatrist, or a graduate student under the supervision of the professional staff. 3. Prompt Service You will be seen for services in a timely manner. At busy times during the semester, Counseling Services may have a waiting list. Our waiting list is generally managed on a first come, first served basis. If, however, you experience a crisis before you are assigned to a counselor, please contact your intake counselor so that crisis services can be arranged. 4. Respect Counseling Services staff will respect you as an individual and convey this respect by providing you with quality care, keeping appointments or contacting you if a change in time is necessary, and giving you complete attention during sessions. 2. Disclosures that do not require your permission Child Abuse: If, in our professional capacity, it comes to our attention that a child is abused/maltreated, we must report such abuse/maltreatment to Child Protective Services. Emergency Situations: We may use or disclose information about you if we are unable to obtain your consent yet you need emergency treatment. If this happens, we will try to obtain your consent as soon as we reasonably can after providing or arranging for treatment. To Avoid Harm: We may disclose information about you to protect you or others from a serious threat of harm by you. National Security: We may be required, by federal law, to disclose information about you to federal officials for intelligence and national security activities. Release of Information to Parents or Guardians: Parents/Guardians can request counseling information on a student minor (under 18 years of age). In non-emergency situations, consent for treatment must be provided by a parent/guardian for an unemancipated minor to receive treatment at Counseling Services unless to do so would be detrimental. Lawsuits and Disputes: We may disclose information about you if we are ordered to do so by a court or administrative tribunal. III. YOUR RESPONSIBILITIES 1. Participation Your active participation in the counseling process is necessary for progress to be made. It is important that you notify your counselor if your problem worsens. 2. Cancellations It is your responsibility to keep scheduled appointments, unless rescheduled or cancelled at least 24 hours in advance. If we do not hear from you within a week of your missed appointment, we may not be able to keep an appointment time open for you. If you repeatedly no-show for appointments we may no longer be able to provide you with services and may need to refer you to a provider in the community. 3. Feedback The Counseling Services staff is interested in any positive or negative feedback you may have regarding the services you receive. We may ask you to complete an anonymous evaluation asking you for feedback about our services. If for any reason you are not satisfied with the counseling process, we encourage you to discuss this first with your counselor. If your concerns are not resolved to your satisfaction, you may request an appointment with the Director or Associate Director of Counseling Services to discuss possible reassignment or other counseling options. if they are an unemancipated CONSENT TO TREATMENT I hereby agree to counseling/treatment/assessment/consultation at Counseling Services. I have read the information contained in the above “Counseling Services: Rights, Privacy, Responsibilities and Consent to Treatment” and understand these provisions and policies; a copy of this document has also been provided to me. I understand I may address any questions regarding this consent with a counselor. I also understand that this consent will remain in effect until I am no longer a UB student, and that I have the right to later revoke my consent. If I do not sign this consent, or later revoke it, Counseling Services may decline to provide services to me. ________________________________ Student Signature _____________ ________________________________ _____________ Date Staff Signature Date 54 APPENDIX E: GUIDELINE FOR CASE DISPOSITION AND COUNSELOR ASSIGNMENTS Client Severity Scale: Guideline for Case Disposition University at Buffalo Counseling Services 1 Severity Rating Skill Learner / Information Seeker None to Minimal Psychological Distress None to Minimal Behavioral Functioning 2 3 4 Distressed Moderately Impaired Severely Impaired Transient to Mild Mild mood concerns Mild anxiety / rumination Able to contain affect Difficulty with motivation, procrastination Sleep and/or appetite largely maintained Limited somatic complaints Some fatigue or energy loss Suicidal ideation largely absent Minimal to Slight Academic work slightly impacted Attends class, work Maintains personal hygiene Maintains leisure activities Daily routine largely maintained Functions largely independently Moderate Moderate mood disruption Moderate anxiety / rumination Affect less contained Diminished concentration Some disruption with sleep and/or appetite somatic complaints Fatigue or energy loss Sporadic suicidal ideation Moderate Marked impact on academic work Sporadic class, work attendance Decline in physical appearance Leisure activities impacted Daily routine disrupted Some difficulty functioning independently Severe Depressed and/or anxious mood almost daily Overwhelming anxiety / panic / worry Affect labile / constricted / blunted / flat Impaired memory / concentration / attention Sleep and/or appetite disturbance Somatization / depersonalization Severe fatigue or energy loss Recurrent suicidal ideation w/ often intent and/or plan Threat to self / others Impaired reality testing Severe Unable to maintain academic work Doesn’t attend class, work Disintegrated personal appearance Leisure activities largely absent Unable to maintain daily routine Unable to function independently Social Support Adequate Adequate Problematic Insufficient GAF Range 100 – 81 80 – 61 60 – 51 50 or lower Beginning Level Trainee Group Tx Can wait to be seen Disposition Beginning Level Trainee Group Tx Can wait to be seen Provide info or refer to other resources (e.g., career, workshop, Wellness Education) Middle Level Trainee Group Tx, if no lethality Psychiatric evaluation, if appropriate Preferably seen within two weeks Advanced Level Trainee 24-48 hour follow up Psychiatric evaluation, if necessary Possible hospitalization considerations 55 APPENDIX F: REFERRAL FORM Referral Process The following steps are intended to help you find an off-campus mental health provider. The term mental health provider includes psychologist, psychiatrist, social worker and counselor. Please be aware this is a general guideline and may not include all that you will need to do. 1. If you plan to use your health insurance to help pay for services, you should refer to your insurance card to help you access a list of providers. There is usually an 800 number to call. Call the number and obtain a list of providers. Do not assume that all providers in private practice are mental health providers covered by your insurance company. 2. If you do not have health insurance or you are deciding not to use your insurance, the process will still require research and work on your part. Paying for counseling can be very expensive with fees ranging from $40 $120 session. Some providers have sliding scales where they will provide services at a reduced fee. You will need to talk to the provider regarding the reduced fee. There are also some agencies, which provide counseling services at a lower cost. 3. If you were given the name(s) of mental health provider(s) it is important to call as soon as you can. There may be a period of waiting time to get on someone’s schedule. The more flexible you are with your schedule, the greater the likelihood of being seen sooner. 4. Many providers have answering machines/services. Be prepared to leave your name, number, referral source, and a good time for the person to return your call. It will not be unusual to play phone tag. Be patient. 5. If you were given a referral by a Counseling Services staff member and you are encountering difficulty with the referral process, please call the staff member to discuss additional options. REFERRALS 1. Name: _____________________________ Phone: __________________________ 2. Name: _____________________________ Phone: __________________________ 3. Name: _____________________________ Phone: __________________________ 4. Name: _____________________________ Phone: __________________________ Staff Member: _________________________________________ Date: ______________ 56 APPENDIX G: CONSENT TO RECORD FORM Counseling Services CONSENT TO RECORD COUNSELING SESSIONS I, ________________________________________________, hereby give consent to my assigned (client's name) counselor, __________________________________________, at Counseling Services at the State University of New York at Buffalo to: videotape__________ (initial if Yes) audiotape__________ (initial if Yes) video-recording__________ (initial if Yes) our counseling sessions. These recordings will be used to aid the counseling process and to gain further understanding of important aspects of the treatment. I have discussed this procedure with the counselor, including the Counseling Center's policy on confidentiality. Recordings will be maintained on a secure server and are erased periodically and not later than the end of the academic year of contact with Counseling Services. I understand that refusal to sign this form will not affect my eligibility for receiving services at this agency. I understand that I may withdraw my permission at any time. Signed ___________________________________ Date____/____/______ Counselor__________________________________ Date____/____/______ 57 APPENDIX H: COUPLES COUNSELING POLICY FOR NON-STUDENT PARTNERS COUPLES COUNSELING POLICY FOR NON-STUDENT PARTNERS 1. 2. 3. Non-student spouses or significant others of currently enrolled students may receive services only when they are seen jointly with the student. If a counselor determines that the non-student in the couple needs crisis or other forms of treatment, the nonstudent will be given referrals to mental health providers in the community. If the student in a couple decides to terminate treatment, the non-student will be given referrals to mental health providers in the community. I have read and agreed to the abovementioned policy. _________________________ Client Signature & Date ________________ Date of Birth or ID# _________________________ Client Signature & Date ________________ Date of Birth or ID# _______________________ Witness Signature 58 APPENDIX I: PSYCHIATRIC SERVICES INFORMED CONSENT FORM Psychiatric Services Informed Consent The following policies are in place because psychiatric services at UBCS are a limited resource given the number of UB students being served. In order to schedule an appointment with the psychiatrist I must first meet with a counselor who will decide on the appropriateness of the referral. To receive psychiatric services here I must currently be an active client of Counseling Services and see a counselor at least once a month. If I am prescribed medication(s), it is my responsibility to take it as prescribed and follow-up with the psychiatrist as recommended. If I have any questions or concerns about side effects or other issues regarding my medication, I will contact Counseling Services and ask to consult with my psychiatrist. I agree not to give or share any of my medication(s) with others. If I require medication for a learning disability or ADD/ADHD, I must first provide outside documentation of that disability before the psychiatrist will be able to write a prescription. If I schedule an appointment with the psychiatrist, I will give at least a 48-hour notice if I have to change it. If I do not show up for a scheduled appointment and had not notified Counseling Services, I understand that it may jeopardize my eligibility for future appointments with the psychiatrist. If I am prescribed medication(s), it is my responsibility to ensure that I have enough to cover school breaks, holidays, and summer vacation. All prescription refills are done at time of my appointment with my psychiatrist. Emergency refills may be acquired at: - ECMC Medication and Prescription Clinic: 898-4245, 462 Grider Street - Buffalo General Med Clinic: 859-5600, 100 High Street - Any hospital Emergency Room - My Primary Care doctor _________________________________ Student’s Signature ________________________________ Date _________________________________ Printed Name _________________________________ Counselor _________________________________ Printed Name ______________________________ Date 59 APPENDIX J: CPEP EVALUATION REFERRAL PROCEDURES Whenever you think a client is in need of evaluation by the Comprehensive Psychiatric Emergency Program (CPEP) at Erie County Medical Center CPEP, CONSULT WITH YOUR SUPERVISOR, ANOTHER COLLEAGUE, AND/OR DIRECTOR. IF YOU DECIDE THAT AN EVALUATION IS NECESSARY: 1. Call University Police at x2222 a. Identify yourself by name and University at Buffalo Counseling Services b. Give the student’s name to University Police c. Request a transport to escort the student to CPEP Request that they do NOT bring a stretcher They should come to 120 Richmond Quad 2. Let the front desk know you called University Police, and give the secretary the client’s name 3. Arrange for your supervisor or colleague to assist you with this process (e.g. let you know when University Police arrives, inform them of the situation while you work with the client) 4. If the student is an international student, request a signed release/exchange of information form from the student to communicate with the International Student & Scholars Services office (ISSS). ISSS can assist the student in contacting family members overseas and can assist the student upon release from the hospital if admitted. 5. Request signed release/exchange of information form from the student for CPEP 6. Request signed release for Residence Life (if they live in the residence halls) 7. If student has provided release for contact with CPEP, call 898-3465 immediately to: a. Let them know a student is en route b. Provide them with information regarding the student c. If other people (e.g. friends, RA, HD) are involved, they should also be encouraged to call CPEP and provide additional information d. Request that CPEP call you back with disposition information following the evaluation 8. Follow up with CPEP to determine the disposition of the evaluation, and to make an after-care plan. 9. Provide updates as appropriate to the people for whom the student has provided releases for disclosure of information. 10. Follow up with the student directly to discuss after-care plans. 60 APPENDIX K: GUIDELINES FOR SAME DAY EMERGENCY CONSULTATIONS (Client Handout) The staff of Counseling Services is aware that emergencies requiring immediate attention can exist for students seeking our services. Because of the demand on our services, however, we are not able to see most students the same day they contact us. This handout has been prepared to help you decide whether our same-day crisis services are right for you. Our same-day crisis services are designed to assist students who are confronting life-threatening circumstances, current or recent traumatic crises, or serious mental illness. Examples of such issues include: · · · · · · · · · · suicidal thoughts the need to be hospitalized thoughts about harming another person recent assault or abuse concern about your own safety knowledge of another person being abused or assaulted the safety of someone else hallucinations recent death of a loved one witnessing or experiencing a traumatic event A counselor is available to meet with students in crisis when not being seen immediately could lead to serious consequences or seriously intensify their existing condition. If you believe your situation is a crisis that cannot wait for a regularly scheduled appointment, please let the secretary know. A counselor will meet with you today to do a brief assessment and make recommendations on how to proceed. 61 APPENDIX L: GUIDELINES FOR ASSESSING SUICIDALITY I. Current Assessment of Suicidality Risk A. Assess current ideation: Content of thoughts? B. Assess current intent: What would stop you? Do you have future goals? C. Assess current plan: Method? Details vague or planned? (Final acts) Is time planned? Availability of means? Chance of intervention? Precautions against intervention? II. Current Situational Factors A. Living situation (alone vs. with other(s) B. Interpersonal isolation C. Availability of social supports D. Current stressors school/work failure family problems sexual assault medical condition holidays/anniversary reactions losses (e.g. deaths, end of relationship, recent abortion, etc.) E. Single vs. married/in relationship III. History A. Past Suicide Attempts: How many previous attempts? When (age)? Why? Medical attention? Did you tell anyone before attempt? After? Did you expect/want to die? Did you act to obtain help? What was your reaction after the attempt? Were you in counseling when you attempted? Did you seek counseling after attempt? How do you feel about the attempt now? B. Other Factors: Recent/Past significant losses Suicide attempts by family members/friends Suicide completions by family members/friends Long-standing psychological disorder Evidence of personality disorder 62 Religious beliefs Past physical/sexual abuse Existing medical conditions (cancer, AIDS) IV. Emotional Factors A. B. C. D. E. F. G. V. Behavioral Factors A. B. C. D. E. VI. Level of depression Level of hopelessness Level of agitation Level of rage/anger Evidence of a thought disorder Level of self-regard Coping style (denial? impulsivity?) Level of self-control (impulsivity/ability to delay) Recent changes in behavior Recent changes in appearance Changes in daily functioning Substance Abuse Alcohol Drug use Combination use Planning A. Contracting: verbal/written reliability of contract B. Suicide Rating 1 - 10 (Self-Report) C. Plan for leaving session Accessing social supports Managing emotions Contact with a counselor Future appt (ext. initial assessment) Referral contacts D. Call for consult -- possible CPEP transport 63 APPENDIX M: NYS MENTAL HYGIENE LAW – HOSPITAL COMMITTALS (University at Buffalo Police Department Policy) Hospital Committals – Mental Hygiene 9.41 and/or Alcohol/Substances 22.09 These guidelines will be followed for all student, faculty, staff and visitors when members of this department are requesting hospital committals and the examination of a person who is a danger to themselves or others. Two hospitals which will accept these committals are the Erie County Medical Center (ECMC) Comprehensive Psychiatric Emergency Program (CPEP) and Buffalo General Hospital. All police officers with hospital committals will complete the 9.41 paperwork. Situations have arisen in the past where patients taken to the hospital as voluntary committals have left the hospital after the police have cleared and the hospital has no authority to keep the patient unless the police have filed a request for examination of the person. In addition, officers committing intoxicated persons to the hospital under 22.09 (alcohol admission) where the person has exhibited violent behavior towards themselves, will notify the hospital staff of this behavior. This is requested so that the hospital will have the patient examined by a psychiatrist to determine if they may be a danger to themselves or others. A 22.09 admission is not normally seen by a psychiatrist. In the event we have a homeless person with issues of mental illness or addiction problems and we know that they will not be taken to the hospital under the 9.41 or 22.09 hospital admissions protocol, they may be taken to the City Mission located at 100 East Tupper Street, phone number 894-2800 or Harbor House located at 130 Genesee Street (corner of Oak), phone number 842-4184 and their hours of operation are from 11:00 PM to 9:00 AM, seven days a week. For all 9.41 committals, an officer will go to the hospital in the ambulance or follow closely in a patrol vehicle. For a voluntary committal where there is no police involvement requested, our role will only be to coordinate ambulance transport and complete a CD Report indicating the requestor’s name. This is based on the UB counseling personnel determining that the person is not an imminent danger to themselves or others. At times, UB counseling personnel may request a police presence in addition to the ambulance even though it is a voluntary transport. 64 APPENDIX N: HEALTH INSURANCE CLAIM FORM FOR INTERNATIONAL STUDENTS TRANSPORTED VIA AMBULANCE 65 66 APPENDIX O: CRISIS CLIENT PROCEDURES [See next page] COUNSELING SERVICES CRISIS CLIENT PROCEDURES Crisis or other emergency occurs Available IA? YES NO Can client wait for next IA? YES NO Schedule in open same-day IA Crisis Counselor available? YES NO Contact the Crisis Counselor Crisis Counselor will take client Crisis Counselor cannot take client Counselors should be contacted in this order: 1. Available senior staff counselor 2. Available psychology intern 3. Interrupt staff meeting 4. Interrupt committee meeting 5. Interrupt training 6. Interrupt supervision 7. Interrupt co-therapy session (e.g., group) [“co-therapy” = when there is more than one therapist conducting a session] 8. Interrupt individual therapy 67 APPENDIX P: REFERRAL FORM FOR MANDATED ASSESSMENTS REFERRAL FORM FOR MANDATED ASSESSMENTS Name of Student:____________________________ Student ID:______________ Referred By (check one): _____Athletics _____Judicial Affairs/Student Wide Judiciary _____Wellness Education Services _____University Residence Halls & Apartments Contact Person________________________________________________________ Dept/Office______________________________________________________________ Phone Number___________________________________________________________ Referred To: (Please check) _____ Counseling Services 120 Richmond Quadrangle North Campus, Ellicott Complex Phone: 645-2720, Fax 645-2175 Student should call and request an Intake Appointment and inform secretary that this is a mandated appointment A copy of this form should be given to the student and a copy must be faxed to Counseling Services at 645-2175. The referring person should attach a brief description of the incident that is prompting the referral. The appointment must be made within 5 days of today’s date and the assessment must be completed within 30 days _____ UB SAFER Session:___________________ Contact person: Marla McBride Wellness Education Services 114 Student Union Phone: 645-2837, Fax 645-6234 _____ Off-Campus Mental Health Provider Contact Information: ____________________________________ ____________________________________ ____________________________________ ____________________________________ I have freely chosen this option and will contact the above office within 5 days of my signature on this form. __________________________________ Student Signature __________________________________ Date 68 APPENDIX Q: ASSESSMENT VERIFICATION FORM ASSESSMENT VERIFICATION FORM Student Name__________________________________ ID#____________ Date of Birth_______________________________ This is to verify that _______________________________________________ Student’s name has completed an assessment as mandated by __________________________________ Referring person/office on _____________________________________________________________________ Date _______________________________________________________________________ Signature of Mental Health Provider To be filled out at time of Assessment Form to be returned BY STUDENT to referring person/office RETURN FORM TO REFERRING OFFICE/AGENCY BY STUDENT 69 APPENDIX R: POLICY AND GUIDELINES FOR USE OF PSYCHOLOGICAL ASSESSMENTS **** Violation of the rules stated below may result in disciplinary action. **** For Part-Time Trainees (Beg/Adv Pracs, SW Interns, GA’s) Psychological assessment training is not typically part of part-time training programs. However, if you are interested in this, you should consult with your individual supervisor. The supervisor will assess his/her level of competency in overseeing test administration and interpretation. S/he will also determine the appropriateness of psychological assessment for specific clients. Your individual supervisor will also determine your training needs in utilizing particular instruments. S/he might need to assist you in identifying a senior staff person who is trained in the particular psychological assessment instrument(s). The Assessment Coordinator is available to assist in this process. She is also available for consultation on when testing is appropriate/inappropriate and information about specific instruments. All assessment instruments are kept locked in the far right rotating file cabinet in Room 118. A list of the psychological assessments available for you to use is posted on the computer: H:\Counseling Services\Testing and Assessment\Description of Instruments (Revised Jan 08).doc. The list is also provided in Appendix T. Do not forget to obtain consent from your client to conduct psychological testing. Both the test administrator and client need to sign the Consent to Psychological Assessment Form (see Appendix S). The top copy should be given to the client and the bottom copy should be placed in the client’s file. Procedure to obtain testing materials: Ask your individual supervisor or the designed trained senior staff person for the specific testing materials. S/he will have to sign it out. Do not take instruments out of UBCS. Do not allow your clients to take data sheet or forms home to complete. Testing should occur in the office. Procedure to return testing materials: Simply return the materials to your individual supervisor or the designed trained senior staff person by the next business day. Permission to keep instruments for an extended period may be granted upon consultation with your individual supervisor or the designed trained senior staff person. S/he needs to consult with the Assessment Coordinator. Procedure to obtain laptop for computer scoring: Computer scoring is available for some instruments. Ask your individual supervisor or the designed trained senior staff person for the Dell Latitude D600 laptop (CNSL-LPTOPXP-1). S/he will have to sign it out. Do not take the laptop out of UBCS. Do not save client data on public computers. The client’s id number (not name) should be used on computer-scoring programs. Enter the raw data and generate an interpretive report. Since the laptop gets poor wireless connectivity, you will not be able to print the report directly. You will need to save the report on a jump drive and print it from an office/workstation computer. Do not forget to delete the report from the jump drive after printing. Consult with your individual supervisor or the designated trained senior staff person for accurate test interpretation. S/he needs to sign off on your work. Testing sessions and results should be documented in a Titanium note (“Testing”). Audio/videotaped responses need to be transcribed into a Titanium note and then the tape should be erased. Hand-written responses also need to be transcribed if they are illegible. All raw test data should be stored in the client’s file. Instruments should be used solely for the purpose of professional (clinical, training, research) activities at UBCS, never for personal, academic, or other business use. Please comply with the UBCS confidentiality policy/regulation, Ethical Guidelines put forth by the American Psychological Association and National Association of Social Workers, and New York State Law. Do not copy or duplicate instruments. Do not destroy or damage instruments. Do not steal or sell instruments. 70 For Staff & Psychology Interns All assessment instruments are kept locked in the far right rotating file cabinet in Room 118. A list of the psychological assessments available for you to use is posted on the computer: H:\Counseling Services\Testing and Assessment\Description of Instruments (Revised Jan 08).doc. The list is also provided in Appendix T. Do not forget to obtain consent from your client to conduct psychological testing. Both the test administrator and client need to sign the Consent to Psychological Assessment Form (see Appendix S). The top copy should be given to the client and the bottom copy should be placed in the client’s file. Procedure to obtain testing materials: Unlock the far right rotating file cabinet using key #1353 from the lockbox. Use the sign-out sheet to indicate what instruments you are using. Note: You are required to sign out instruments under your name when signing materials out for trainees. Please let the Assessment Coordinator know if supplies are getting low. Do not take instruments out of UBCS. Do not allow your clients to take data sheet or forms home to complete. Testing should occur in the office. Procedure to return testing materials: Return the materials to the file cabinet by the next business day. Permission to keep instruments for an extended period may be granted upon consultation with the Assessment Coordinator. Procedure to obtain laptop for computer scoring: Computer scoring is available for some instruments. Software is maintained on the Dell Latitude D600 laptop (CNSL-LPTOP-XP-1). It is stored in the far right rotating file cabinet in Room 118. Unlock this cabinet using key #1353 from the lockbox. Be sure to complete the Sign-Out Sheet for Laptop or Projector. Do not take the laptop out of UBCS. Do not save client data on public computers. The client’s id number (not name) should be used on computer-scoring programs. Enter the raw data and generate an interpretive report. Since the laptop gets poor wireless connectivity, you will not be able to print the report directly. You will need to save the report on a jump drive and print it from an office/workstation computer. Do not forget to delete the report from the jump drive after printing. If you are not trained in a particular psychological assessment instrument, then consult with the Assessment Coordinator or another senior staff person for accurate test interpretation. Testing sessions and results should be documented in a Titanium note (“Testing”). Audio/videotaped responses need to be transcribed into a Titanium note and then the tape should be erased. Hand-written responses also need to be transcribed if they are illegible. All raw test data should be stored in the client’s file. Instruments should be used solely for the purpose of professional (clinical, training, research) activities at UBCS, never for personal, academic, or other business use. Please comply with the UBCS confidentiality policy/regulation, Ethical Guidelines put forth by the American Psychological Association and National Association of Social Workers, and New York State Law. Do not copy or duplicate instruments. Do not destroy or damage instruments. Do not steal or sell instruments. 71 APPENDIX S: CONSENT TO PSYCHOLOGICAL ASSESSMENT Counseling Services CONSENT TO PSYCHOLOGICAL ASSESSMENT Psychological assessment, also referred to as testing, is a process in which formal procedures are used to gather information about a person’s personality, mood, thoughts, and/or behaviors. The findings from psychological assessment are often used to compare the participant’s responses to the responses of other people of similar demographic backgrounds. Psychological assessment is frequently used as a supplement to counseling, as way to help gather more information about a person, track changes over time, or plan treatment. By my signature, I acknowledge that: 1. The potential benefits and risks of the assessment process have been explained to me. I agree to discuss with the test administrator any concerns I have before, during, or after the assessment. 2. I fully and freely give consent to participate in the assessment process; or, if I have been mandated to participate in this assessment, I give my assent to participate in the process. If I have been mandated to this assessment, I understand that I retain the right to refuse to participate, and that the test administrator does not have control over how the referral source will respond to this refusal. 3. I understand that if I give consent to the release of my assessment records, no part of the assessment record can be omitted. I understand that the general confidentiality guidelines to which I have consented apply to the assessment process. 4. I understand that an important part of the assessment process is to have my results reviewed with me and get the opportunity to have my questions answered. _____________________________ __________ Client Signature Date ________________________________ Client Name (please print) _____________________________ __________ Test Administrator Signature Date ________________________________ Test Administrator Name (please print) 72 APPENDIX T: AVAILABLE PSYCHOLOGICAL ASSESSMENT INSTRUMENTS COGNITIVE TESTING Bender Visual-Motor Gestalt Test It’s used to evaluate visual-motor functioning & visual perception skills in children & adults. It’s usually part of neuropsychological assessment. The client is asked to reproduce geometric designs. Administration takes 5-10 minutes. Hand scoring is available. Mini Mental Status Exam This is a screening tool. It’s used to evaluate cognitive functioning along five dimensions: (1) orientation, (2) registration, (3) attention/calculation, (4) recall, (5) language. Administration takes 5-10 minutes. Hand scoring is available. Wechsler Adult Intelligence Scale – Fourth Edition (WAIS-IV) The WAIS measures different components of intelligence. There are 10 core subtests and 5 supplemental subtests. Administration takes 60-90 minutes. Hand scoring is available. VOCATIONAL TESTING Campbell Interests and Skills Survey (CISS) It measures vocational interest & skills. It compares this against various occupations & also provides an estimate of the individual’s confidence in his/her ability to perform various occupational activities. Internet self-administration takes 20-25 minutes (Assessment Coordinator must assign a username & password). Computer scoring & interpretation is available. PERSONALITY TESTING Objective: Millon College Counseling Inventory (MCCI) This is an objective personality test. It’s a new test designed to measure personality & pathology specifically in college students. Self-administration takes 20-25 minutes. Hand scoring is available. Minnesota Multiphasic Personality Inventory – Restructured Form (MMPI-2-RF) This is a revised and shortened version of the MMPI-2, containing 338 true-false questions. It is a very thorough assessment of personality and psychopathology. Self-administration takes 40-50 minutes. Hand scoring is available. Myers-Briggs Type Indicator (MBTI) This is an objective personality test. It assesses personality types along four dichotomies: (1) extraversion vs. introversion, (2) sensing vs. intuition, (3) thinking vs. feeling, (4) judging vs. perceiving. Self-administration takes 1525 minutes. Hand scoring is available. NEO PI-R This is a 240-item objective personality test based on the Five Factor Model of normal personality development, assessing the 5 global personality domains, and specific facets of each domain. Self-administration takes about 3040 minutes. Hand scoring is available. Personality Assessment Inventory (PAI) This is an objective personality test. It assesses personality & pathology. Self-administration takes 40-50 minutes. Computer scoring is available. 73 Projective: Projective Drawings: House-Tree-Person & Draw-A-Person These are projective measures of relationship to self, others, and world. Administration takes 50-60 minutes. You only need paper and pencil. Information about hand scoring and interpretation is available. Rorschach Inkblot Test This is a projective measure of personality and psychopathology. Administration takes 60-90 minutes. The examiner records responses verbatim and codes responses for scoring and interpretation. We have the RIAP-5 computerized interpretation assistance program, which assists with scoring and interpreting Rorschach results. Rotter Incomplete Sentences Blank This is a projective measure of adjustment/maladjustment & personality traits. Self-administration takes 20-40 minutes. To score, conduct an informal review of responses and look for themes. We are looking into purchasing a manual, with current norms & scoring criteria, for this test. Thematic Apperception Test (TAT) This is a projective measure of thought patterns, attitudes, & emotional responses to ambiguous stimuli. The examiner decides how many picture cards to show (out of 31). Administration takes 60-90 minutes. The examiner records responses verbatim. Hand scoring is available. CONTENT-SPECIFIC TESTING / SCREENING TOOLS Beck Anxiety Inventory (BAI) This is a screening tool. It measures the presence & degree of anxiety. Self-administration takes 5-10 minutes. Hand scoring is available. Beck Depression Inventory (BDI) This is a screening tool. It measures the presence & degree of depression. Self-administration takes 5-10 minutes. Hand scoring is available. Brief Symptom Inventory (BSI) It assesses symptomatology and its intensity at a specific point in time. Self-administration takes 8-10 minutes. Hand scoring is available. College Adjustment Scales (CAS) It assesses nine areas of adjustment difficulties: (1) anxiety, (2) depression, (3) suicidal ideation, (4) substance abuse, (5) self-esteem, (6) interpersonal problems, (7) family problems, (8) academic problems, (9) career problems. Selfadministration takes 15-20 minutes. Hand scoring is available. Conners Adult ADHD Rating Scales (CAARS) It assesses adult ADHD symptoms & emotional lability. Self-administration takes less than 20-30 minutes. Hand scoring is available. Eating Disorders Inventory (EDI-3) This test assesses for psychological traits that are relevant to eating disorders, to aid in case conceptualization, treatment planning, and evaluation of treatment outcome. The test contains 91 items and self-administration typically takes 20-30 minutes. We also have the EDI-3 RF, which is a brief version of the test (25 items) and the EDI-3 SC, which is a symptom checklist that is used to determine whether a person meets the diagnostic criteria for an eating disorder. Each of these should take 10-15 minutes for self-administration. HCR-20 74 This is a 20-item checklist designed to assess the risk for future violent behavior in criminal and psychiatric populations. The HCR-20 includes variables which capture relevant past, present, and future factors. The checklist is completed by a clinician after interviewing the client and reviewing any supporting materials (e.g., notes & reports from the client’s file). Items should be coded based on the information gathered in your assessment of the person. Learning and Study Strategies Inventory (LASSI) It measures students’ awareness & use of learning & study strategies related to skill, will, & self-regulation components of strategic learning. Self-administration takes 30 minutes. Hand scoring is available. OCD Screener/Screening Test for OCD These are two very brief self-administered OCD screening tools to assess the severity of OCD symptoms. Each can be completed in 5-10 minutes. Outcome Questionnaire (OQ-45.2) It measures therapy progress along three dimensions: (1) subjective discomfort, (2) interpersonal relations, (3) social role. Self-administration takes 15-20 minutes. Hand scoring is available. Questionnaire for Eating Disorder Diagnoses (Q-EDD) This is a comprehensive questionnaire identifying disordered eating behaviors to aid in diagnosis. Administration takes 20-30 minutes. Hand scoring is available. Sexual Violence Risk – 20 (SVR-20) This is a 20-item checklist of risk factors for sexual violence that were identified by a review of the literature on sex offenders. The checklist was developed to improve the accuracy of assessments for the risk of future sexual violence. The checklist is completed by a clinician after a detailed lethality assessment has been conducted. Items should be coded based on the information gathered in your assessment of the client. Social Anxiety Scale It evaluates a range of social & performance situations that individuals with social phobia may fear and/or avoid. Self-administration takes 15-20 minutes. Hand scoring is available. Substance Abuse Subtle Screening Inventory (SASSI-3) This is a screening tool for substance abuse. It’s comprised of obvious and subtle items. Self-administration takes 1015 minutes. Hand scoring is available. “Connecting Clinician & Client” DVD is available. It provides information on SASSI interpretation & feedback. Thomas-Kilman Instrument (TKI) This is a brief assessment tool that measures conflict management style. The test consists of 30 forced choice items. Self-administration takes 10-15 minutes. Trauma Symptom Inventory (TSI) This is a 100 question test that assesses for symptoms of Posttraumatic Stress Disorder (PTSD) and Acute Stress Disorder (ACD), as well as interpersonal difficulties associated with more chronic psychological trauma. Selfadministration takes 20-30 minutes. Yale-Brown Obsessive Compulsive Scale (Y-BOCS) It assesses the severity and type of obsessive-compulsive symptoms. Self-administration takes 15-20 minutes. Hand scoring is available. Zung Self-Rating Depression Scale This is a screening tool for depression. Self-administration takes 5-10 minutes. Hand scoring is available. 75 APPENDIX U: MANDATED REPORTING OF CHILD ABUSE When a client discloses information giving the counselor reason to believe that a child under the age of 18 may be under threat of continued physical or sexual abuse or severe neglect, the counselor is obligated to report this situation to the State Registry in Albany. Procedures for reporting follow state-mandated laws, which include provisions for clinical discretion in protecting the confidentiality of the client and the therapeutic relationship. If at all possible, have the client call the New York State Child Abuse and Maltreatment Register him/herself (800-342-7472) from your office. Or the counselor may make the call (mandated reporters, such as mental health professionals, call 800-635-1522) with the client present. We are required to report, and may maintain client anonymity. Information reported includes family composition and how the information was obtained so as to protect the child. HOTLINES: NYS Child Abuse Hotline (Mandated Reporters) 800-635-1522 NYS Child Abuse Hotline (General Public) 800-342-7472 Suicide Prevention 800-333-4444 76 APPENDIX V: WEBSITE INFORMATION ABOUT EMAIL CONFIDENTIALITY AND ONLINE SERVICES E-mail Policy Counseling Center, SUNY Buffalo Counseling Center e-mail address: couns-ctr@acsu.buffalo.edu A hyper-text version of this policy can be found at: http://ub-counseling.buffalo.edu/email.html The following policy is on the website: The staff of the Counseling Center welcomes your contact. We also value your privacy and time and therefore offer the following information to help you decide on the best method for reaching us. We hope that these guidelines are helpful to you as you decide how best to reach our staff. We take your time and confidentiality very seriously and therefore consider it imperative that you understand the limitations of our use of e-mail technology. 1. If You Are Looking For On-line Counseling or Advice Unfortunately, e-mail is not an appropriate medium for personal counseling. Therefore, we do not offer on-line counseling. If you are a UB student seeking counseling or assistance with a problem, please visit our office or call to make an appointment with one of our counselors. If you need immediate assistance, please stop by our offices or contact us by phone. Please contact us at: Counseling Center 120 Richmond, North Campus 645-2720 HOURS: M, T, F 8:30 a.m. -5 00 p.m. Wed. and Thurs. 8:30 a.m.-7:00 p.m. Alternatively, you can call the Crisis Services telephone hotline at 834-3131 -- they are open 24 hours a day, 365 days a year. 2. Important Information about Email Confidentiality We cannot guarantee that your e-mail will remain confidential. We will do our best to keep your communications private. However, our university administration, like many other employers, reserves the right to monitor our e-mail usage and might therefore see the text of your message. If you are in any way concerned about the contents of your email being read by someone other than the person you are contacting, you should consider alternate ways of contacting us. When we respond to your e-mail, we will respond to the address from which it is sent. If you do not wish others who may have access to the e-mail account you are using to also have access to our response, please consider another means of communication. 1. How quickly you can expect a reply While we try to check our e-mail regularly, you have no way of knowing if one of us is unavailable due to illness, vacation, or other reasons, or if there are problems with the network itself. This means that your message may not be received immediately. If time is of particular concern for you, you should consider calling our office at 645-2720 or calling Crisis Services, a 24 hr hotline, at 834-3131. 4. If you are not a University at Buffalo student Due to conflicting demands on our time, we have had to develop priorities to help us determine how to best spend our resources. 77 First and foremost, since we are funded by UB student fees, we place the highest priority on responding to e-mail from UB students. While we welcome e-mail from others, at times of high demand we may not be able to respond to those not affiliated with UB. Likewise, we can not promise to respond to requests for assistance with a class project, homework assignment, or other academic pursuit. 5. Referral Suggestions Buffalo area: http://ub-counseling.buffalo.edu/Referrals/referrals.html Elsewhere in the U.S.A.: http://www.apa.org/practice/state.html Counseling Service, Division of Student Affairs, State University of New York at Buffalo December 1, 1997. Portions of this Email Policy were adapted from the policy developed by Career and Counseling Services at the University of Houston-Clear Lake This is an automatic reply to the message you sent to couns-ctr@acsu.buffalo.edu UB COUNSELING SERVICES EMAIL POLICY: A more detailed version of this Email Policy can be read at: http://ub-counseling.buffalo.edu/email.shtml University at Buffalo Admissions information can be found at: http://www.buffalo.edu/admissions There are several ways you may have come upon our email address. Every once in a while we receive an email message seeking services we do not provide. We therefore send this automatic reply to everyone who emails us to clarify our services. WHAT WE ARE: The Counseling Services office at the University at Buffalo provides mental health counseling for UB students. We also offer extensive outreach and consultation services for the UB community, as well as provide training for graduate students in our Practicum and Externship placements and our MSW and Psychology (APA-accredited) Internship Programs. Our office is staffed by doctoral level psychologists, certified social workers, a psychiatrist, and graduate level trainees. To make an appointment, call our office at 645-2720 or stop by 120 Richmond Quad, and ask to be scheduled for an appointment with one of our counselors. Appointments must be arranged by phone or in person, we do not use email for this purpose. We maintain a web site at http://ub-counseling.buffalo.edu where you can learn more about our services and find other helpful information. IF YOU ARE LOOKING FOR ON-LINE COUNSELING OR ADVICE: Unfortunately, e-mail is not an appropriate medium for personal counseling. Therefore, we do not offer on-line counseling. If you are a UB student seeking counseling or assistance with a problem, please visit our office or call to make an appointment with one of our counselors. While we try to check our e-mail regularly, you have no way of knowing if one of us is unavailable due to illness, vacation, or other reasons, or if there are problems with the network itself. This means that your email message may not be received immediately. If you need immediate assistance, please stop by our offices or contact us by phone, 645-2720. If your call is after regular business hours, call Campus Police, 645-2222, and ask to speak to the counselor on call. 78 Alternatively, you can call the Crisis Services telephone hotline at 834-3131 – they are open 24 hours a day, 365 days a year. Or visit our on-line referral directory at: http://ub-counseling.buffalo.edu/referral .shtml IF YOU ARE NOT A UNIVERSITY AT BUFFALO STUDENT: Due to conflicting demands on our time, we have had to develop priorities to help us determine how to best spend our resources. Since we are funded by UB student fees, we place the highest priority on responding to e-mail from UB students. While we welcome e-mail from others, at times of high demand, we may not be able to respond to those not affiliated with UB. For referrals in your area, call 800-964-2000 or see http://helping.apa.org/find.html IMPORTANT INFORMATION ABOUT EMAIL CONFIDENTIALITY: We cannot guarantee that your e-mail will remain confidential, although we will do our best to keep your communication private. However, there are many ways that an e-mail message can be intercepted. Therefore, if you are in any way concerned about the contents of your e-mail being read by someone other than the person you are contacting, you should consider alternate ways of contacting us. The staff of the Counseling Service office welcomes your contact. We also value your privacy and time and therefore hope the above information helps you decide on the best method for reaching us. Counseling Services A part of the Student Wellness Team State University of New York at Buffalo 120 Richmond Quad, Buffalo, NY 14261 716-645-2720 (Hours: M, T, F 8:30 a.m.-5:00 p.m. and Wed. and Thurs. 8:30 a.m.-7:00 p.m.) 79 APPENDIX W: LIST OF COMMITTEES Committees and Consultative Relationships UBCS Committees: 1. Professional Development – Task is to look at workplace issues directly associated with on going training, staff self-care, and quality of workplace. 2. Quality Assurance – Task is to maintain and improve clinical services delivery at Counseling Services including reviewing and revising policies and procedures, developing mechanisms for training/informing everyone on policy and procedure, tracking clients' progress thru our system, and identifying and minimizing risk management issues 3. Training – Tasks are to maintain and improve the quality of training for the various trainee groups at Counseling Services, and consists of Training Director, Social Work Internship Coordinator, Practicum Coordinator, Assistant Practicum Coordinator and other staff as deemed necessary by the director 4. Suicide Prevention – Tasks are to address agency policy and procedural issues, staff training needs and campus education and intervention needs with regard to suicide, depression and harm reduction, and implementation of the Garrett-Lee Smith campus suicide prevention grant 5. Outreach Committee – This committee develops innovative, educational, non-clinical ways to assist students particularly those from underrepresented populations. Responsible for updating or creating educational materials on paper and web-based. Responsible for developing policy and procedures related to consultation with the campus community and outreach. 6. Green Committee – Aims to identify, advance and promote strategies, policies and practices within the Department’s operations aimed at minimizing negative environmental impact and maximizing benefits to the environment. Campus/External Committees: Alcohol Review Board Campus Life and Student Development Team (CLSD) Community Standards Team Diversity Committee Eating Disorders Treatment Team Green Team International Student Committee Personal Safety Residential Life Team Safe Zone & Allies Program Students of Concern Student Health Advisory Student Medical Insurance Social Work Field Education Board SWT Outreach Advisory Group Social Work SWT Leadership Group Student Affairs Alcohol Committee Student Affairs Marketing Committee Students of Concern Student Affairs Web Committee Suicide Prevention Committee Violence Prevention Team Student Affairs Work Life Student Wellness Athletic Team SWT (Large Group) Violence Prevention Committee 80 APPENDIX X: SEXUAL ASSAULT RESPONSE GUIDELINES General procedures: Encourage the student to go to a local hospital Emergency Room for medical services and the collection of evidence. Emphasize that this does not obligate the student to press charges, but gives them the option of doing so, if they later wish to. If they prefer to go to the Student Health Center, please make clear that they are not able to collect evidence admissible in court; by going there, the student may be weakening their legal position. An anonymous proxy report (http://www.student-affairs.buffalo.edu/judicial/proxy.shtml) which contains no identifying information about the student, can be filed with Public Safety by the Counseling Services staff, unless the student specifically requests this not be done. Encourage the student to file a report with University Police. If the assault occurred off campus, the student is advised to go to the local police with jurisdiction. Clearly explain that filing a report does not obligate the student to press charges. Explain that reports to University Police of sexual assault are voluntary and confidential. In an emergency situation that presents a threat to others on campus, University Police may alert the Dean of Students and/or the Ombudsman, who may take necessary action to protect the community while respecting the student's anonymity. Encourage the student to meet with the Ombudsman, who offers support, understanding and identification of the services and legal and judicial options available to the student. Inform the student that the University has a disciplinary hearing process for incidents of sexual assault. Details of this process can be confidentially discussed with the Ombudsman without filing charges. The Ombudsman can offer other supports to the student including possible changes in living arrangements and help in managing academic demands. Ask if the student has a safe place to go; help the student locate such a place, if needed. II. The student has the following options: Formal Option: The student reports the incident to University Police. Females may ask for a female officer. There is a squad of specially trained officers who are the Sexual Assault Team; they will investigate the report. The student may also meet with the Ombudsman, who offers support, understanding and identification of the services and legal and judicial options available to the student. All discussions are voluntary and confidential, although information may be shared with the Sexual Assault Team of University Police in cases when an incident presents a danger to the community. Any and all actions taken by the Team, including the possible release of a warning to the community, are designed to protect the reporting student's anonymity. If Counseling Service’s staff is to have contact with the Ombudsman that requires the student's identity or other confidential information is disclosed, the staff member obtains the student's written permission for that specific information to be released to the Ombudsman. Emphasize that the student may choose to stop participation in the process at ANY time. Informal Option: The student's identity is not disclosed to anyone without the student's permission, unless a danger exists for the student or others by the student's actions. Full legal and judicial services are not available to the student without disclosure of the student's identity. Treatment services (Counseling Services, Student Health Center, emergency room of local hospitals) are available and are explained to the student with encouragement to use the services. Based on the proxy report, the Sexual Assault Team (University Police) may identify a need to take action in order to protect the larger community; for example, from other information they have, University Police may recognize a pattern of rapes/sexual assaults and want to alert the residence hall/neighborhood involved. In such cases, the actions are designed to protect the student's anonymity. 81 If the informal option is initially chosen and the student later decides to take formal action, the formal option may be initiated. However, the student needs to be informed that the formal option may be more limited at a later time due to the lack of evidence and the passage of time. The choice of the formal or informal option is up to the student. For either option, an anonymous proxy report can be filed immediately with University Police by you, the counselor. III. Medical Services/Evidence Collection: Recommend medical care whether or not the student wishes to prosecute. Encourage the student to go to a local hospital Emergency Room for the collection of evidence and medical services or the Student Health Center for medical services only. If the student is not certain they want to prosecute, they should still go. They may be injured, and even if they are not (and they might not realize they are injured), they need to be checked for possible injuries, venereal disease, pregnancy, etc. Procedures: Student should not bathe, shower, douche, change clothing or even urinate (if possible). If oral sex was involved, no brushing of teeth, drinking or smoking should occur, as these activities will damage evidence. They will need a change of clothing since the hospital will keep clothing as part of the evidence. Evidence is held by the hospital for 30 days so that they have time to decide to press charges, or not. Police prefer a victim to report an incident within 24 hours to maximize the possibility of apprehending the perpetrator. If evidence is gathered by the appropriate medical personnel at the medical facility, University Police or the police with jurisdiction over the incident, they will take possession of the evidence until the student makes a decision about pursuing charges or not. It is important for the student to understand that the gathering of evidence does not commit them to filing charges. The student's name is placed on the evidence kit at the time of the examination and the evidence held in a confidential manner until the student decides. If they decide to file charges, the evidence is an important part of the case. Inform the student that the use of the Student Health Center or local hospital emergency room is voluntary and confidential. (Note: the Student Health Center may file an anonymous proxy report unless they know we have already done so.) Also, the student should know that their name will be used to identify any evidence collected, and the evidence will be held in a strictly confidential manner. Help the student make arrangements to have a friend (or Residence Hall Director) accompany them to the hospital emergency room. The hospital will call Crisis Services who will provide a Rape Advocate Counselor to meet the student at the hospital. The student may choose to talk with the Rape Advocate Counselor or not. The Rape Advocate Counselor will help them understand the process of the exam, as well as her legal options. Follow-up face-to-face personal counseling is available on a limited basis from Crisis Services, usually with someone other than the Rape Advocate. Crisis Services can also assign a Court Advocate who will accompany the student through all court proceedings, if she wishes. IV. Miscellaneous Information: There is no limit as to when the student may report the crime; the sooner it is reported, the sooner it can be followed up. The police will accept a report weeks or months later. Later reporting makes it harder for the police to get more information or evidence, but it may still help them catch the perpetrator. Most rapists are 82 repeat offenders, and the victim's report (including proxies) might help police have a stronger case against the offender for a previous incident or a later one. V. Other information * Inform the student that New York State has a Crime Victims Board (847-7994) which might pay for wages lost from work because of the rape, and perhaps physical damage (to the room/apartment, stolen wallet, etc.). They must file a report with the police within five days to use the Board. This does NOT mean that they must press charges, however. They can report and not press charges, or decide to press charges. They are free to drop the case at any point. The Crime Board also might pay for the physical exam; there are other means of paying for these charges, too (Medicaid, health insurance, etc.). In the Residence Halls there is the option of having the perpetrator moved to another building, banned from contact with the victim, etc. The Residence Life staff or the University Ombudsman can make these arrangements. Academic advisors can arrange for a student to make up a missed exam, be excused from classes or withdraw from (drop) a class. With written permission from the student, you may contact the advisor for her or him (if she/he wishes), and make these arrangements. For students who wish it, we can facilitate withdrawal from the University through the Student Health Center. Formal withdrawal enables the student to return more easily (less red tape) in the future; it will also allow any reimbursement of tuition, food services charges, etc. that the student may be entitled to. Check the blue form in the mailroom that lists all the offices a student needs to contact to leave the University; these things can be done later from home, too. Getting an official Leave of Absence from their department will ensure that their place in the department will be held for them and they will not need to re-apply if they return within one year. UB CAMPUS RESOURCES: University Police - Emergencies Counseling Services Student Health Services Anti-Rape Task Force Judicial Affairs & Student Advocacy 645-2222 645-2720 829-3316 829-2584 645-6154 LOCAL COMMUNITY SERVICES FOR SEXUAL ASSAULT: Police 911 Crisis Services 24-hour Hotline 834-3131 Crime Victims Board 847-7992 83 APPENDIX Y: UB’S SEXUAL HARRASSMENT POLICY What is sexual harassment? Any unwelcome sexual advances, requests for sexual favors and other verbal or physical conduct of a sexual nature constitutes sexual harassment when: 1. Submission to such conduct is made either explicitly or implicitly a term or condition of an individual's employment or academic advancement; 2. Submission to or rejection of such conduct by an individual is used as the basis for employment or academic decisions affecting such individual; 3. Such conduct has the purpose or effect of unreasonably interfering with an individual's work or academic performance, or creating an intimidating, hostile, or offensive environment. Who is likely to be harassed? Although harassment of men by women exists, the over-whelming majority of students who encounter sex-related threats, demands, humiliating and intimidating behavior are females. Who is the harasser? The sexual harasser is usually a person who is in a position of authority; someone who could affect your academic or employment status. He/she may be in a position to evaluate your performance, write recommendations or otherwise contribute to academic and/or career enhancement. However, the harasser could well be someone who has no authority to affect your academic or employment status. He or she could be a co-worker, a colleague, a class/dorm-mate, a visitor to the University, or a non-faculty employee of the University. The sexual harasser is anyone whose conduct has the purpose or effect of unreasonably interfering with your academic or work performance or whose conduct has the purpose or effect of creating an intimidating, hostile or offensive working, educational or living environment here at the University. How do you know if you are being harassed? Ask yourself: 1. Are comments made about my clothes, make-up and body more than my work? 2. Am I told intimidate stories about marital problems and sexual escapades? 3. Does the harasser tell dirty little jokes, or show me lewd pictures that seem to imply sex with him or her is fun? 4. Are there attempts to get my sympathy with sad stories about a failing love life? Does the harasser say things about his or her spouse that embarrass me? 5. Is the harasser curious about my happiness, my dates, my sexual and emotional fulfillment? 6. Am I invited into his or her office to talk about nothing? 7. Does the harasser bump into me "accidentally", or try to fondle or kiss any part of my body? 8. Have I been told I'm his or her "type"? 9. Have I been whistled at in a suggestive manner? 10. Has it been suggested, implied, or plainly stated that the status and conditions of my academic standing or student employment depend on granting sexual requests? 11. Does the harasser make obscene gestures, or leer at my body? 84 12. Did my academic or working conditions worsen after rejecting the harasser's sexual advances? 13. Is any of my work area decorated with centerfold-type posters or pictures, printed quotations having a sexual connotation, or other offensive objects or displays of a sexual nature? 14. Does the course material, classroom instruction, classroom environment, or the instructor condone and/or promote sexual harassment? The impact of sexual harassment Common reactions of persons who are subjected to harassment include feelings of anger, guilt, helplessness, frustration, and fear. There are often concerns about personal safety, loss of privacy and the threat of possible retaliation if the situation is reported. Sexual harassment undermines the self confidence, well being and peace of mind of the individual who is offended, and it damages the spirit of trust and collegiality that is central to our University community. The State University of New York at Buffalo does not condone harassment of any kind and is dedicated to eliminating both blatant and subtle forms of sexual harassment within the University community. Persons whose conduct is judged to be offensive or harassing or whose conduct is considered retaliatory towards their accuser may face disciplinary action including expulsion or loss of employment. What can you do? Speak up at the time If the sexual harassment is blatant: say NO. Say it firmly and without smiling. You want the harasser to know you are serious. State clearly that you don't like what was said or done and you want that behavior to stop. Another way to confront the harasser is to write him or her a letter. The letter should detail what the person did, how it made you feel and how it affected your work. The letter should specifically ask him/her to stop the behavior. In some cases, harassers don't realize that their behavior is offensive or unwelcome. The letter is an excellent way of clarifying your objection. A verbal or written objection is helpful but not essential if you decide to file a grievance at a later date. Tell someone about it Even if you are not sure you will report the incident, tell someone what happened. Discuss it openly with others. Find out if others have been harassed by the same person. Keep records Keep a diary or log of what is happening to you. Include dates, places, direct quotes, and names of other people that were present. Save any letters, cards, or notes sent to you. Let someone read your records. Keep everything in a safe place. Get a witness Ask someone to watch you when the harasser is around. Most advances are made when the harasser thinks no one is watching. Seek advice or counseling Students often feel powerless when confronted with situations described in the How Do You Know section, but there are people here on campus who are available and willing to help. You should seek support and advice on stopping sexual 85 harassment. See the section: Where on Campus You Can Get Help. Where on campus can you get help? If the harassment is on-going or if the initial incident is highly disturbing or humiliating or if at any time you feel threatened, it is important for you to discuss the situation with someone who can intervene. Students are encouraged to bring complaints of harassment to the attention of an instructor, an advisor, the chair or unit head or the dean. Request a meeting with the appropriate supervisory or administrative personnel and be prepared to describe clearly and in detail the nature of the sexual harassment and request that the harassment stop. Another source of assistance, advice, or intervention is the staff in the Office of Equity, Diversity, and Affirmative Action Administration, 108 The Commons, (645-2266). You may speak confidentially to the Director or to the Associate Director. Related Policies Regardless of the options you pursue in dealing with harassment, University policy provides for the following: 1. Complaints will be handled with confidentiality. University procedures for investigating and resolving sexual harassment complaints ensure confidentiality for all parties to the extent possible. In each case, the complaint handler will seek the permission of the individual bringing the complaint before disclosing information and will discuss any concerns regarding confidentiality. 2. Complaints will be handled as quickly as possible. If an investigation or longer resolution period is required, the parties involved will be updated regularly on the status of the inquiry. 3. Retaliatory behavior will be addressed. Retaliation for filing a complaint is illegal and violates University policy. Retaliatory behavior can take many forms: discriminatory action that may affect work or grades, ostracism or further objectionable behavior by the person against whom a complaint was made. The fear of such actions may prevent many from reporting harassment. Be assured retaliatory actions related to a sexual harassment complaint will be treated seriously. Sexual Harassment: The Laws Sexual harassment is a form of unlawful discrimination. It is a violation of federal law under Section 203 of Title VII of the 1964 Civil Rights Act, as amended in 1972; under Title IX of the Education Amendment of 1972 and under Executive Order 11246. In addition, New York Executive Order 19 forbids sexual harassment in state agencies. SUNY at Buffalo Policy on Sexual Harassment 4.3 Sexual Harassment Sexual harassment of employees and students, as defined below, is contrary to University policy and is a violation of federal and state laws and regulations. Unwelcome sexual advances, requests for sexual favors, and other verbal or physical conduct of sexual nature constitute sexual harassment when: (1) submission to such conduct is made either explicitly or implicitly a term or condition of an individual's employment or academic advancement; (2) submission to, or rejection of, such conduct by an individual is used as the basis for employment or academic decisions affecting such individual; (3) such conduct has the purpose or effect of unreasonably interfering with an individual's work or academic performance, or creating an intimidating, hostile or offensive environment. No University employee of either sex shall impose a requirement of sexual cooperation as a condition of employment or academic advancement, or in any way contribute to or support unwelcome physical or verbal sexual behavior. Any member of the University community who requires additional information, wishes to make a complaint or to receive a copy of the University procedures to be followed for resolving complaints of sexual harassment should contact the Office of Equity, Diversity, and Affirmative Action Administration, 406 Capen, 645-2266. Sexual harassment of any type is considered unacceptable at the State University of New York at Buffalo. 86 APPENDIX Z: UBCS ORGANIZATIONAL CHART COUNSELING SERVICES ORGANIZATIONAL CHART Sharon Mitchell, Ph.D. Director & SWT Leadership Group Coordinator Liz Snider, LCSW-R Associate Director Clinical Director Group Coordinator Satellite Office Manager Andrea Greenwood, PhD Assistant Director Asst. Clinical Director Support Staff Michelle Olandese, LCSW-R Outreach Coordinator Student office workers Amanda Tyson, Ph.D. Practicum Coordinator Carissa Uschold, LCSW-R Suicide Prevention Coordinator Outreach GA Sung Kim-Kubiak, Ph.D. Assistant Director Training Director Suicide Prevention GAs 1st year, Practicum Students, Advanced Practicum Students, Clinical GAs & Externs Psychologists, Social Workers Thom Neill, LCSW Social Work Internship Coordinator Social Work Interns Predoctoral Psychology Interns Psychiatrists Psychiatric Residents 87 APPENDIX AA: DUE PROCESS PROCEDURES FOR ADDRESSING STAFF GRIEVANCES Whenever staff have problems with other staff or the work environment, informal resolution of staff grievances is always encouraged. When informal attempts have been inadequate in sufficiently addressing this grievance, a more formal procedure will be necessary. Counseling Services expectations for informal and formal processes of addressing staff grievances are outlined below. Potential Grievances may arise from various sources, including: 1. 2. 3. 4. 5. Problem with colleagues Problem with support staff Problem with immediate clinical supervisor Problem with administrative leadership Problem with trainees Informal Process and Chain of Communication: 1. In accordance with APA (American Psychological Association) and NASW (National Association of Social Workers) ethical and professional guidelines, the staff member is to first directly discuss the problem with the individual most directly involved in the conflict or grievance. 2. An attempt should be made to resolve the grievance in-house (i.e. within Counseling Services) before moving to the university level. If an attempt to address the problem with the person most directly involved is unsuccessful in reaching a satisfactory resolution, the staff member should consult with administrative leadership to try other possibilities of for informal resolution. If the problem is with another staff member or support staff, it is appropriate to consult with the Associate Director and/or Director. If the problem is with a trainee, it is appropriate to consult with the designated trainee group coordinator (i.e. Training Director, Social Work Intern Coordinator, or Practicum Coordinator). If resolution has still not been reached, it may also become necessary to consult the Associate Director and/or Director. 3. When this informal process is inadequate to address the problem, a more formal process may be engaged, as outlined below. Formal Process: Please consult the University at Buffalo’s procedures for addressing grievances. 88 APPENDIX BB: DUE PROCESS PROCEDURES FOR ADDRESSING STAFF IMPAIRMENT Staff Impairment Staff impairment will be defined broadly as an interference in professional functioning that includes: an inability to acquire and integrate professional standards into one’s repertoire of professional behavior an inability to control personal stress; psychological dysfunction; and/or excessive emotional reactions that interfere with professional functioning Problems may become identified as impairments when they include most of the following characteristics: 1. 2. 3. 4. 5. the staff member does not acknowledge, understand or address the problem when it is identified, the problem is more than a skill deficit which can be rectified by remediation efforts, the quality of services delivered by the staff member is consistently negatively affected, the problem is not restricted to one area of professional functioning, the staff member’s behavior does not change as a function of feedback, remediation efforts, and/or time Informal Process of Addressing Staff Deficiencies or Problematic Behaviors: 1. The Associate Director and/or Director will discuss the concern with the staff member. If possible, they will come to agreement about the concern and appropriate action to be taken, including specific remedial recommendations. 2. If this is unsuccessful in remediating the problematic behavior, the Director will decide on further steps to be taken, including moving to a more formal process of addressing the concern. Formal Process for Responding to Staff Deficiencies or Impairment: Please consult University at Buffalo’s procedures for addressing staff impairment. 89 APPENDIX CC: BUILDING EVACUATION PLAN BUILDING EVACUATION PLAN As a building occupant, you need to be familiar with this plan. Read it carefully. UNIT COORDINATOR: Sharon Mitchell or the senior administrator on duty FLOOR MONITOR 1: Carissa Uschold (Wing 1) FLOOR MONITOR 2: Andrea Greenwood (Wing 2) ALTERNATE FLOOR MONITOR: Unit Coordinator will designate alternates if necessary EMERGENCY ASSEMBLY AREA: Richmond Parking Lot B (the one closest to Spaulding) EMERGENCY NOTIFICATION PROCEDURES Contact University Police at 645-2222 Call from a safe location and remember to: Stay calm. Be prepared to answer the following questions: Where is the emergency located? What is the emergency? (fire, medical, hazardous material, etc.) How did it happen? When did it happen? Who are you? (your name) Gather any other information that may be useful for the emergency responders (e.g. are there any injuries involved?). Do not hang up until instructed to do so by the dispatcher. You do not need to know all the answers to these questions, but quickly gather as much information as you can. Give a telephone number or safe location where the emergency responders can call or meet you, and wait for the responders at that safe location. Support Staff List On a daily basis, print a staff work schedule and have available a list with phone numbers for each office in the building. Once in the emergency assembly area give both lists to the Unit Coordinator Unit Coordinator Responsibilities Conduct primary "sweep" of the assigned area to ensure evacuation and/or carrying out directive to evacuate buildings. Report to assigned evacuation location immediately after the primary "sweep" Do roll call after receiving the staff work schedule from the support staff Meet with floor monitors to gather information about injuries, people still in buildings, damage to buildings, etc. Try to contact missing people by calling their office phone. Work with the floor monitors to calm people and treat injuries (as appropriate and depending upon training); Provide support to the campus emergency responders in accordance with the nature of the disaster or emergency. Maintain security and assure safety of residents and others present during an emergency. 90 Floor Monitor Responsibilities Carry out orders to evacuate, respond to fire alarm by evacuating occupants Carry out evacuation: pound on doors or stand outside and yell, "You must evacuate this building now!" Instruct people to pick up coats, flashlights, blankets, medication, shoes, keys, ID, as they leave the building. DO NOT GO BACK INTO THE BUILDING. Direct people to the assigned emergency assembly area. Keep people from running, sightseeing, etc. Touch closed doors. Do not open them if they are hot. Note building damages, people trapped inside, and injuries. Move injured people to evacuation area if possible (a monitor stays with an individual with head and/or neck injuries, if in a relatively SAFE location.) Perform emergency first aid/CPR if training, and necessary to do so. Follow people to assigned evacuation location and stay with them unless otherwise instructed by emergency personnel. Gather information from people, calm people, treat injuries, do informal head counts, keep people at evacuation location. Meet with Unit Coordinator to give information, get further instructions. If a Unit Coordinator is not present by the first 10 minutes, delegate a floor monitor to assume the Unit Coordinator’s responsibilities. GENERAL EVACUATION PROCEDURES A building occupant is required by law to evacuate the building when the fire alarm sounds. When evacuating the building: Stay calm, do not rush, and do not panic. Safely stop your work. Gather your personal belongings if it is safe to do so. (Reminder: take prescription medications out with you if at all possible; it may be hours before you are allowed back in the building.) If safe, close your office door but do not lock them. Use the nearest safe stairs and proceed to the nearest exit. On your way out, warn others nearby If trained, able and safe (with a sure and safe exit), use a portable fire extinguisher to extinguish the fire. Evacuate if one extinguisher does not put out the fire. Proceed to the designated Emergency Assembly Area (Richmond Parking Lot B) and report to your roll taker; Sharon Mitchell or the senior most CS administrator on duty. Wait for any instructions from emergency responders. Do not re-enter the building or work area until you have been instructed to do so by the emergency responders. 91 APPENDIX DD: STUDENT ASSISTANT APPOINTMENT CHECKLIST Student Assistant Appointment Checklist & Information Name Person Number Account Number Phone Number Rate of Pay Effective Date Appt End Date Reappointment Ethnicity: Initial Appointment Ethnicity Source: White/Caucasian Black/African American (not of Hispanic Origin) Declared by Employee Asian or Pacific Islander Observed at Interview / Appointment Hispanic Surmised from Name / Other Information Native American Degree & Major Working Towards Expected Graduation Date month/year Forms Attached: I-9 Copy of acceptable forms of Identification (not expired) W-4 IT-2104 or IT-2104E Direct Deposit ERS membership form 92 Additional Documents Required for International Students: Copy of Visa Copy of Passport Copy of I-94 Copy of I-20