HSL
advertisement

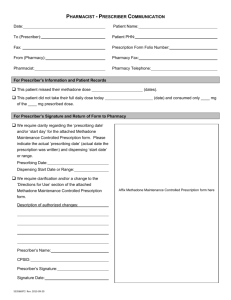
HASTINGS AND ST LEONARDS PRIMARY CARE TRUST Local Enhanced Service Patients suffering from Drug Misuse 1.0 Service outline The following elements of the service would need to be in place for the purpose of this specification: 1. Established links with the GP liaison nurses who will support the practices engaged in the scheme. 2. The maintenance of an accurate register of patients receiving treatment for a substance misuse problem (excluding alcohol), to be developed with the assistance of the PCT 3. A sequential review, as appropriate, (formal GP review every three months for maintenance of patients and monthly for detoxification patients; 4. GP shared care reviews, with GP Liaison Nurses funded separately, every six weeks for maintenance patients and every two weeks for detoxification patients. 5. Safe and secure practices, appropriate for the provision of such services 6. Facilities and administrative support to enable the GP liaison nurses to undertake regular patient reviews within the practice 7. A good knowledge of, and effective liaison with, local drug services and other agencies, including nonstatutory services. 8. Links between local pharmacies, primary care drug support workers, social services (including the Child Protection Service) and local mental and clinical health teams 9. Mechanisms to return patients to secondary care within a five day time scale where their management becomes problematic or more complex. This enhanced service will fund practices to be able to: 1. Develop and co-ordinate of the care of drug users and develop practice guidelines. 2. Practices must have knowledge of local detoxification procedures (attached at Appendices A, B and C). 3. Treat dependent drug users with support. This should be available from, for example, SMS GP liaison nurses, community pharmacists, and lead clinicians in the local specialist providers. It includes the prescribing of substitute (opiate and non-opiate) drugs including antagonists using best practice as outlined in the Department of Health’s drug misuse clinical guidelines. 4. Ensure that prescribing takes place within a context in which the co-existing physical, emotional, social and legal problems are addressed as far as possible. 5. Participate in audit of prescribing practice (appendix F ) 6. Act as a resource to practice colleagues in the care of drug users 7. Demonstrate additional training and continuing professional development. This should be commensurate with the level of service provision expected of a clinician in line with any national or local guidance to meet the requirements of revalidation. This may be achieved by attendance at the appropriate RCGP training course completed within one year of commencement of this service and through routine support of specialist GP liaison nurses. 8. Maintain the safety and training of clinical and non-clinical staff (including reception staff). Funding considered necessary to meet the training requirement in the first year of the scheme will be met by the PCT. Complex and demanding patients will be identified through an agreed protocol and will be returned to management within the secondary care setting. Access to treatment places within this service will be via the arrangements agreed within the Models of Care framework as set out in the proposed local pathway. Patients appropriate for treatment within general practice (see Appendix D) will be required to sign a contract with the practice agreeing acceptable levels of behaviour and the consequences of non-compliance (see Appendices E and C). Where a patient being treated under the scheme remains on the list of their own general practitioner for the provision of primary medical services there must be an effective means of communication between practitioners. 16/02/16 1 Hastings and St Leonards PCT The practice will be required to submit audits on a six-monthly basis in accordance with the protocol included at Appendix F. 2.0 Proposed Local Pathway This service will be a managed access service with one point of entry for assessment. Participating practices will each have an agreed quota of patients allocated to meet the collective target of 59 treatment places across the PCT’s population. The pathway will be as follows: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Screening by all GPs. Referral of appropriate cases to the Substance Misuse Service Full assessment by Addaction and SMS. Care plan agreed. Patients suitable (see Appendix D) for primary care based treatment referred to practices participating in this enhanced service based on availability of treatment places and patient choice. GP Liaison nurses will coordinate the agreement to be jointly signed by the GP, community pharmacist, Addaction, SMS and patient setting out treatment compliance requirements (see Appendix C ). Addaction to deliver structured day care to patients where appropriate and available. SMS to deliver shared care support and structured counseling via the specialist GP Liaison Nurses. Community pharmacists to deliver daily supervised consumption of methadone for the first three months where appropriate. Should a patient become more complex in terms of needs and unsuitable for this enhanced service, the SMS will prioritise a return of the patient to their care within five to ten working days. 3.0 Accreditation Those doctors who have previously provided services similar to this enhanced service and who satisfy at appraisal and revalidation that they have such continuing medical experience, training and competence as is necessary to enable them to contract for the enhanced service shall be deemed professionally qualified to do so. A practitioner providing enhanced services in drug misuse will be supported by a nominated member of the GP Liaison Nursing Team. The practitioner should have the skills to: 1. 2. 3. 4. 5. 6. 7. 8. 9. Identify and treat the common complications of drug misuse Carry out an assessment of a patient’s drug use Provide harm reduction advice to a current drug user or his or her family Test (or refer for testing) for other viruses, including HIV, Hepatitis B and C, liver function tests, and immunisation for hepatitis A and B to at risk individuals Provide drug information to carers and users as to the effects, harms and treatment options for various common drugs of use Assess and refer appropriately, patients for drug misuse substitution treatment Utilise the range of commonly used treatment options available for treatment including pharmacological interventions Be aware of local policy Work in an appropriate multidisciplinary manner. 4.0 Appraisal criteria The appraisal criteria will include both the generalist and special interest aspects of the work. It is expected that the GP providing an enhanced service attends the RCGP course (funding to be made available by the PCT) Arrangements for continuing professional development will be agreed with the PCT including regular monitoring meetings attended by participating practices and specialist service providers 16/02/16 2 Hastings and St Leonards PCT The following protocols in appendices A and B are included as guidelines in good clinical practice. It is anticipated that the initiation of prescribing will be undertaken at the Substance Misuse Service prior to the patient becoming the responsibility of a practitioner within the scheme. Ongoing treatment will then be reviewed regularly in conjunction with the GP liaison nurses. There may however be exceptional circumstances when it is considered necessary to undertake prescribing prior to referral to the Substance Misuse Service. In such circumstances the available guidance should be adhered to and a referral to the Substance Misuse Service continue to be processed as normal. 16/02/16 3 Hastings and St Leonards PCT Appendix A OPIATE PRESCRIBING PROTOCOLS Responsibilities of the prescribing doctor: 1. Substitute prescribing should not be undertaken in isolation. A multidisciplinary approach is essential. 2. Prescribing is the ultimate responsibility of the doctor. The responsibility cannot be delegated. Further advice will be available from GPwSI and the Consultant in Substance Misuse. 3. The doctor prescribing controlled drugs for the management of drug dependence should have an understanding of the basic pharmacology, toxicology, and clinical indications for the use of the drug, dose regime and therapeutic monitoring strategy to prescribe responsibly. 4. To participate in a full assessment of the client, in conjunction with the substance misuse service and treatment goals set. 5. No more that one week’s prescription should be dispensed at one time, except in exceptional circumstances. 6. The client should be advised of safety in storage of medication and advised regarding driving and other risks. A patient information leaflet will be provided for participating practices. 7. Thorough, clearly written computer records of prescribing should be kept. Substitute prescribing should only be considered if: 1. There is convincing evidence of current dependence (including objective signs of withdrawal) i.e. sweating, lachrymation and rhinorrhea, yawning, feeling hot and cold, anorexia and abdominal cramps, nausea, vomiting and diarrhoea, tremor, insomnia and restlessness, generalised aches and pains, tachycardia, hypertension, gooseflesh, dilated pupils, increased bowel sounds. 2. The assessment clearly substantiates the need for treatment i.e. history, urine toxicology. The history would include the clients verbal evidence of illicit drug use, type and amount of drug used, route of administration. Clinical evidence of track marks and recent injection sites. The urine toxicology to reflect illicit drug use (ideally more than one sample) 3. The doctor is satisfied the client will co-operate and demonstrate adequate compliance with the prescribing regime. Do not initiate prescribing if any of the following apply: 1. Drug test screening has not confirmed illicit drug use. One positive urine does not mean that the client is dependent and a full assessment is still necessary. 2. At first contact with the client (unless already prescribed and details have been transferred) Initiating prescribing: The aim is to prescribe a dose of a substitute drug that will prevent withdrawal symptoms and reduce or eliminate illicit drug use. Please note: 1. Some clients may overestimate their usage to obtain a bigger prescription. 2. Some may underestimate their usage in order to please you. 3. Some clients may have unrealistic expectation of the prescription he/she ought to receive. 16/02/16 4 Hastings and St Leonards PCT If in doubt, begin with low doses and titrate subsequent small increases against withdrawals. Drugs To Prescribe For Opiate Dependence: Substitution of heroin for a longer acting oral preparation has proven health and social benefits and is an accepted treatment of opiate dependence. Methadone or subutex are the drug of choice as they are both long acting, straightforward to titrate, less likely to be diverted or injected and is backed by evidence of efficacy. More detailed information on the evidence that underpins these protocols are obtainable from: http://www.nta.nhs.uk/clinical guidelines; http://www.smmgp.co.uk Protocol For Prescribing Methadone 1 Titration from heroin to methadone: At this point a full assessment of the client’s illicit drug use has been obtained and a recommended range of prescribed methadone has been established. It has been explained to the client that: - It is a once daily liquid dose It will not cause euphoria That the initial dose may not be high enough and may need some adjustment It has been explained to the client to abstain from using heroin 6-8 hours prior to commencing methadone Day 1 Methadone should be prescribed in a mixture of 1mg in 1ml. The starting dose should be no more than 40-ml to reduce the risk of overdose. Ideally start at the beginning of the week to ensure that the client will get specialist support in the initial phase of their treatment allow easier titration and stabilisation and prevent overdosing. Advise the client against using on top of methadone due to the high risk of overdose and delayed stabilisation. Explain the methadone effects last for approximately 24 hours, and that the drug builds up over several days. Day 2 Discuss any withdrawal symptoms or over medication. If continued withdrawal symptoms the methadone may be increased 5-10 mls every 2-4 days. Discuss any illicit drug use, and the potential risks. Day 3 Continue to titrate upwards until stabilisation has been achieved. 16/02/16 5 Hastings and St Leonards PCT Research has shown that: higher dosing of methadone (i.e. 60-80mls) has higher retention rates in treatment. greatly reduces illicit drug use and offending behaviour. Higher doses may be required depending on tolerance and specialist advice is recommended. Fortnightly prescriptions can be issued using FP10 instalment prescriptions, stating supervised consumption if required. GPs may obtain a handwriting exemption from the home office if prescribing 10 or more clients. Protocol For Prescribing Subutex Subutex can be considered for patients. 1. Using up to 1.5g of heroin daily 2. Less than 30mls methadone daily (or can be reduced to this level). Direct equivalence between subutex and methadone is difficult to estimate and is not a linear relationship, 12 to 16 mg of subutex is approximately as effective as 50 to 80 mg of methadone in reducing heroin use and retaining clients in treatment. Ideally baseline liver function studies should be obtained for those clients deemed to be at high risk of liver damage i.e. heavy drinkers who have established liver damages, symptomatic hepatitis, and any other disease affecting the liver. About subutex: 1. It is a semi synthetic derivative of opium. 2. It has an effective duration of at least 24 hrs with a half-life of 20-25 hrs. 3. It is available in 0.4mg, 2mg, and 8mg tablets. 4. Administration is via the sub-lingual route, and takes effect in 90-120 mins. 5. It binds to morphine receptors and acts as a partial agonist; because of this effect it may lead to a greater chance of stabilisation and less illicit use on top. 6. Less risk in overdose and lower risk of respiratory depression. 7. It is a useful alternative to methadone and can be considered for detox or maintenance. 8. It has lower euphoric effects at high doses. 9. Blockade of other opiates. 10. With doses between 8-16mg daily it reduces illicit use on top. Consider subutex for the following client categories: 1. Clients new to treatment. 2. Clients requesting a detoxification programme. 16/02/16 6 Hastings and St Leonards PCT 3. Clients wishing for an alternative to methadone. 4. Clients on low doses of methadone and wish to become drug-free, but may struggle with a methadone detox. 5. Clients who are relatively stable on methadone but are using regularly on top. 6. Clients who have long term opiate problems and have failed to stabilise on methadone. 7. Clients who have previously been prescribed methadone but did not respond successfully to their treatment plan. 8. Clients over 18 yrs. Do not use subutex for clients who:1. Are pregnant or breastfeeding without specialist advice/experience. 2. Have severe liver damage. Please note: 1. There is a risk of injecting subutex as it is only available as sub-lingual tablets and highly soluble. Practitioners should ensure that this risk is fully assessed before subutex is considered an appropriate treatment option 2. It is not picked up on a routine urine toxicology screen as an opiate and no subutex specific test is available locally via urine screening. Guidelines for prescribing subutex: 1. Clients using heroin should receive their first dose of subutex at least 6-8 hrs after the last dose of heroin, and preferably experiencing as much withdrawal symptoms as tolerable. Taking subutex soon after using heroin will increase the withdrawal symptoms due to the antagonist within it. 2. Clients on methadone should be reduced to 30 mls or less daily prior to transferring to subutex. They should receive their first dose of subutex at least 24 hrs after the last dose of methadone and/or when experiencing withdrawal symptoms. 3. Full explanation of how subutex works explained to the client. 4. Stabilisation on subutex usually achieved over three days. 5. Clients are usually unsettled for the first three days as the dose is titrated. Administration procedure for subutex: Day 1 Start treatment early in the week to enable daily contact and monitoring for at least the first three days. Starting dose normally 4mg-6mg Day 2 Assess for signs of withdrawal or sedation (it is unusual to experience sedation) and titrate accordingly. For withdrawal the dose should increase by 4mg – 8mg. For sedation reduce by 2mg-4mg. 16/02/16 7 Hastings and St Leonards PCT Day 3 Repeat day two. The most commonly effective maintenance dose is between 8 -16mg daily, but lower or higher doses may be used (maximum 32mg) . One of the most commonly reported problems of starting subutex is insomnia, which may necessitate the need to consider night sedation. In general a time-limited prescription of zopiclone would be recommended. Tablets are taken in one single dose daily sublingually. The GP liaison nurse should see the client at least weekly for the first three weeks of treatment. Any serious side effects should be discussed with the GP liaison nurse. Any missed doses of subutex should not be replaced, as subutex is long acting and the clients should not experience withdrawal symptoms if one day is missed. Subutex can be prescribed by instalments on an FP10 and in the initial stages of treatment daily supervised collection is advised. 16/02/16 8 Hastings and St Leonards PCT Appendix B BENZODIAZEPINE PRESCRIBING PROTOCOLS The central aim of these guidelines is to reduce all benzodiazepine prescribing for this patient group to nil. Key Considerations: 1. Long term benzodiazepine use may cause harm, particularly at doses greater than 30mg daily. 2. They are frequently used as a secondary drug of abuse, either to enhance the effect of the primary drug, or to reduce withdrawal effects. 3. They have a strong addictive potential and the withdrawal syndrome can be dangerous. 4. Illicit benzodiazepine use is widespread and causes a wide variety of harm related to: Ingestion (intoxication, bizarre behaviour) injection (thrombosis, infection) withdrawal (psychosis, fitting). Overdose. 5. Whilst there is no evidence to support the use for maintenance treatment, GPs should be able to accommodate and treat benzodiazapine users and prescribe where appropriate. When prescribed they should be withdrawn slowly and should only be used for detoxification from benzodiazapine addiction and not maintenance unless there are specific indications. 6. The illicit market only exists at all because they are widely prescribed. 7. Prescribing benzodiazepines to young people for the treatment of sleeping problems, anxiety or other psychological difficulties is rarely justified. 8. Benzodiazapines are often taken in conjunction with opiates, and for those clients prescribed methadone, the methadone dose should be kept stable throughout the benzodiazapine reduction period. Concurrent detoxification of both drugs is not recommended in community setting. 9. There are no licensed indications for the prescription of benzodiazepines for more than 2-4 weeks. 10. People who tend to “binges”, or overuse are not suitable for long-term prescribing. Long-term prescribing is sometimes justified, for example with clients who have had long-term prescriptions. However these clients should be encouraged to reduce from high daily doses to a safer one (preferably not more than 30mg). 11. The withdrawal syndrome is unpleasant and potentially dangerous. Sudden cessation of high-dose or long term regime (more than a few weeks) is not good practice. Withdrawal syndrome may start within hours, or be delayed a few weeks after withdrawing long-acting drugs. Symptoms may include: Confusion, psychotic-like states. Anxiety, insomnia, loss of appetite/weight. Tremor, perspiration, tinnitus, perceptual disturbance. Possibility of convulsions. Guidelines for prescribing: 1. Prescribing should only be initiated where there is clear evidence of dependency from the history and urine toxicology. (Caution clients may exaggerate the amount they are taking). This will be in conjunction with a full comprehensive assessment via the substance misuse service. 16/02/16 9 Hastings and St Leonards PCT 2. In general, it is recommended that a prescribing regime should be negotiated and agreed with the client. If considering a detox or reduction it should be determined by the individuals capacity to tolerate symptoms or, more often, by their anticipation of unpleasant withdrawals. Clients may be reassured that they will suffer less withdrawal symptoms on a regime where daily dose is reduced in small portions (range one-tenth to onequarter) every fortnight. Normally clients are able to tolerate a reduction of 2.5mg-5mg every two weeks. 3. For doses below 30mg reduce by 2mg - 2.5mg every 2 weeks. 4. If withdrawal symptoms occur maintain the dose until symptoms improve. 5. If severe withdrawal symptoms occur, increase the dose to alleviate symptoms and reduce by smaller increments. 6. Convert all benzodiazapines to equivalent diazepam dose using the conversion chart below. 7. Prescribe for daily collection using instalment contract (reduces risks of diversion to black-market 8. Overusing of daily dose, or loss of medication) 9. Daily doses should be divided to reduce the risk intoxication. 10. Regular review of the client’s progress by the GP and GP liaison nurse. 11. If carrying out a detox review the client six weeks after successful completion – consider whether there is a need of treatment for underlying mental health problems. Conversion Table For Benzodiazepines To Diazepam Equivalent: DRUG CHLORDIAZEPOXIDE LOPRAZOLAM LORAZEPAM OXAZEPAM TEMAZEPAM NITRAZEPAM 16/02/16 PCT DOSE EQUIVALENT TO 5MG DIAZEPAM 15MG 0.5MG 0.5MG 15MG 10MG 5MG 10 Hastings and St Leonards Appendix C OUTLINE OF ROLES AND RESPONSIBILITIES WITHIN FIVE WAY AGREEMENT The General Practitioner 1. To provide a prescription (as per local protocol) for the duration of the prescribing agreement, levels of medication to be agreed with GP Liaison Nurses. 2. To address the’ general health needs of the client, including encouragement of screening for Hepatitis B and C and uptake of vaccinations for Hepatitis B 3. To Liaise on a regular basis with the GP Liaison Nurses 4. To review the care plans a minimum of three monthly and review accordingly. 5. Ensure cover within the practice (or other LES practices) for periods of Annual Leave etc. The Substance Misuse Service: 1. To ensure the patient is registered with a GP. 2. To ensure liaison between GP’s and SMS consultant, where appropriate. 3. To ensure that the nominated pharmacy is willing to participate within the 5-way agreement and has capacity to undertake dispensing. 4. To ensure relevant paperwork has been completed. The essential documents being; The Triage and Comprehensive assessments, Care plan and STORS form. 5. To complete the assessment and discuss treatment options with the GP 6. To review the clients progress on a regular basis, (intervals to be agreed with LES GP’s). 7. To liaise with the nominated pharmacy on a regular basis 8. To facilitate fast tracking back to SMS for problematic clients. 9. Act as Case coordinator as per the models of care and local ICP protocol. The Pharmacist The pharmacist should report the following to the GP Liaison Nurse: 1. Regularly missed doses or whole dose not consumed under supervision 2. Attempts to avoid supervised consumption 3. Three or more missed consecutive daily doses 4. Late collection of weekly dispensed medication 5. Unacceptable behaviour (including theft) 6. Intoxication 7. Deterioration in health (mental or physical) 16/02/16 PCT 11 Hastings and St Leonards 8. Problems relating to the prescription 9. Requests for decreased frequency of collection, or requests for early Collection of weekend medication or any other concerns the pharmacy may have. Addaction: 1. To deliver structured day care and other services in line with the care plan: 2. Inform the GP liaison nurses of any changes in the circumstances of the client which may have an impact on treatment; 3. Inform the GP liaison nurse of any deterioration in the client’s presentation; 4. Inform the GP laison nurse of changes to drug use; 5. Addaction will maintain confidentiality regarding the use of the needle exchange. The Client: 1. To attend appointments on time and where possible unaccompanied. The exceptions to this being; child care issues or the need for a carer or advocate to also attend. This should prearranged prior to attendance. 2. To behave in an acceptable and appropriate manner (see standards of behaviour). 3. To provide samples when requested to do so, either urine or mouth swab. 4. Female clients to inform GP Liaison Nurse immediately if suspect they may be pregnant. 5. To accept responsibility for dispensed medication and store in a safe and appropriate place. To accept that lost or stolen medication will not be replaced. 6. Not to approach GP directly for increase/decrease in medication but liase with GP Liaison Nurse. 7. To accept that inappropriate or abusive behaviour at the GP surgery, pharmacy, Addaction or SMS may result in termination of treatment programme. 8. Any escalation in illicit drug use or destabilisation will result in review of treatment programme. Fees In 2004/05 each practice contracted to provide these services will receive a £1,032.00 annual retainer, £516.00 withdrawal (detoxification) per patient per annum, and £361.00 maintenance per treatment place per annum. Payments will be made quarterly in arrears following submission of activity data to the PCT These fees will be uprated by 3.225% from 1:4:05 Signed: GP: ------------------------ Pharmacist: ------------------------ GP Liaison Nurse: ------------------------- Addaction worker: ------------------------- Patient: ------------------------ 16/02/16 PCT Date 12 -----------------------Hastings and St Leonards Appendix D Patients suitable for Treatment within Primary Care 1. If under 19 need to be assessed by specialist under 19’s team and need to co-ordinate accordingly. 2. Not pregnant. 3. No severe and enduring mental heath issues that could affect ability to attend appointments and engage effectively with service 4. No severe alcohol use that could adversely affect prescribed medication ( e.g. methadone, diazepam and heavy alcohol use could possibly potentiate unintentional over dose) 5. Those on benzodiazepines should be willing to convert to appropriate level of diazepam and be willing to engage in reduction programme (see appendix 4) 6. Show motivation to reduce or abstain from illicit drug use. 7. Only prescribed medications approved in the Department of Health Clinical Guidelines would be accepted into shared care, eg DF118’s not acceptable, physeptone tablets or injectables would not be considered appropriate. 8. Patients must be willing to undertake a prescription on daily collection and the dose negotiated with the individual GP via the GP Liaison Nurses. Frequency of collection may decrease on evidence of stability/compliance on an individual basis. 16/02/16 PCT 13 Hastings and St Leonards Appendix E PATIENT ATTENDANCE and COMPLIANCE REQUIREMENTS 1 Regular attendance with the GP Liaison Nurses is a condition of LES shared care, intervals of appointments would be negotiated with the GP’s and individual clients as would location of appointments as identified in the care plan. 2 Urine or mouth swabs need to indicate stability and compliance with prescribed medication, any evidence of increase in illicit drug use or downturn in stability would result in re-assessment and possible fast tracking back into the care of the Substance Misuse Service. 3 Patients will be required to enter into a five way contract agreement between the GP, SMS, named Pharmacist, Addaction and the client. 4 Patients on the shared care scheme will be offered Structured Day Care if assessed as suitable and beneficial for the client. 5 The patient or any person accompanying them must not at any time cause a disturbance at any of the agents involved in the five-way agreement. 6 No lost prescription will be replaced. Once collected, the prescription is the responsibility of the client. 7 Any attempt to obtain further amounts of the prescribed medication from any other GP, or fraudulent change to any prescription will result in the contract being withdrawn and the police informed. 8 Theft of property from any of the above parties, their premises or agents (on or off duty) will result in the police being informed and may result in the contract being withdrawn, a period of rapid detoxification or a return to secondary care. 9 Aggressive behaviour (verbal or physical), threats of aggression, racial abuse or intimidation to the above named parties or their agents 10 Attending at any of the above agencies heavily intoxicated with illicit drugs or alcohol will result in review of your contract. 11 The GP reserves the right to issue a written warning for behaviours deemed to be inappropriate, which will remain on record. Any reoccurrence of such behaviours may result in removal from the GP’s list and subsequent withdrawal of the contract. 12 Emergency appointments and house calls are not to be requested in relation to medication issues. 16/02/16 PCT 14 Hastings and St Leonards Appendix F AUDIT AND MONITORING The LES for Drug Misuse will be subject to the following audits: Six monthly audit of prescribing practice and adherence to the standards and protocols contained in the attached guidance (Appendix A and B). Review of the operation of shared care arrangements. This will include the specialist providers that have entered into the 5 way agreement and encompass the provision of facilities, administrative support, clinic preparation, access to information. To be undertaken three monthly initially. Risk assessment to ensure premises are fit for purpose. Patient reviews to an agreed frequency, no less than three monthly for patients receiving maintenance prescription, weekly for patients undergoing withdrawal (detoxification). Audit of those patients returned to secondary care, outcomes of treatment interventions, attendance and DNA rates. Effectiveness of communication with colleagues holding GMS responsibility for patients treated within the scheme. Compliance with additional training and continuing professional development needs identified as a prerequisite to joining the scheme. 16/02/16 PCT 15 Hastings and St Leonards