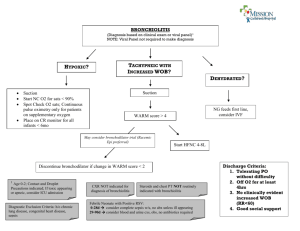
TCTCH Bronchiolitis Guidelines
advertisement

T.C. Thompson Children’s Hospital Evidence Based Clinical Practice Guidelines for Infants with Bronchiolitis (September 23, 2010) Modified from the Cincinnati Children’s Hospital Medical Center Guidelines (August 15, 2005) Target Population 1. Infants less than one year of age presenting to the hospital for the first time with bronchiolitis typical in presentation and prehospital clinical course. 2. These Guidelines are not intended for use in the following types of bronchiolitis patients: Patients with a history of cystic fibrosis, bronchopulmonary dysplasia, asthma, or other significant respiratory disease. Patients with immunodeficiencies. Patients admitted to an intensive care unit. Patients with other significant comorbid conditions complicating care, which may include congenital heart disease, Down syndrome, and conditions which predispose to pulmonary hypertension. 3. For those infants who initially meet guideline criteria but do not subsequently follow a typical course, consideration for a pulmonary consult should be given. 4. The information provided is intended for informational purposes only. This information is derived from clinical experience and clinical research and is intended as a guideline and not as a replacement for any medical provider’s decision making, which shall at all times be and remain in the sole discretion of such provider. Introduction Bronchiolitis is an acute inflammatory disorder of the lower respiratory tract, occurring most commonly in infants and young children, caused by infection with seasonal viruses. Respiratory syncytial virus (RSV) accounts for 50% to 80% of cases.1 Other causes include parainfluenza virus, influenza virus, adenovirus, and human metapneumovirus.2 Viral etiology does not reliably predict illness severity. Typical bronchiolitis is a self-limited disease that is little modified by aggressive evaluations, use of antibiotics, or other therapies. The median duration of illness for children with bronchiolitis is 12 days; after 21 days approximately 18% will remain ill, and after 28 days 9% will remain ill.3 Most infants who contract RSV infection recover without sequelae; however, up to 40% may have subsequent wheezing episodes through five years of age and approximately 10% will have wheezing episodes after age five.4 The average hospital stay is 3-7 days.5-7 RSV associated infant deaths number less than 500 per year in the U.S.; most deaths occur in children without concurrent cardiac or pulmonary disease.8 “Recognizing the pathologic picture that occurs in the airways of children with bronchiolitis is important in understanding the clinical manifestations and developing rational management. The viral infection occurs through the upper respiratory tract and spreads lower within a few days. This results in inflammation of the bronchiolar epithelium, with peribronchial infiltration by mostly mononuclear cells and edema of the submucosa and adventitia. Plugs of sloughed, necrotic epithelium and fibrin in the airways cause partial or total obstruction to 1 airflow. The degree of obstruction may vary as these areas are cleared, resulting in rapidly changing clinical signs that confound an accurate assessment of the severity of illness. A ‘ballvalve’ mechanism can result in trapping of air distal to obstructed areas, with subsequent absorption, atelectasis, and a mismatch of pulmonary ventilation and perfusion that may lead to hypoxemia. Atelectasis may be accelerated by the lack of collateral channels in young children and potentially by the administration of high concentrations of supplemental oxygen, which is absorbed more rapidly than room air. Smooth muscle constriction seems to have little role in the pathologic process, which may explain the limited benefit of bronchodilators observed in clinical studies.” 9 (p 343) Several studies of the use of clinical guidelines for the management of bronchiolitis have shown a reduction in unnecessary resource utilization with a streamlining of medical care for these infants.5,10-15 This document provides a practical, evidence based approach to the diagnosis and management of acute bronchiolitis in infants and children less than two years of age. The recommendations are based on the most current and best scientific information available. In the absence of quality evidence, expert opinion and group consensus were used. Guideline Recommendations Prevention: 1. High Risk Patients: Infants with the following conditions are at increased risk of significant morbidity from bronchiolitis and are at increased risk for hospitalization: age < 3 months prematurity (<35 weeks corrected gestational age) chronic lung disease congenital heart disease immune deficiency syndromes8,16-19 Prevention of bronchiolitis in these patients is of primary importance. Specific measures to prevent bronchiolitis include: limiting exposure to contagious settings (i.e., daycare) and siblings eliminating exposure to second-hand tobacco smoke careful handwashing to minimize spread of viruses. These measures should be discussed regularly with parents of newborns upon nursery discharge and at primary care visits for all high risk patients listed above during bronchiolitis season. Additionally, preventive medical therapy such as palivizumab (Synagis®, MedImmune) may be considered for selected, high-risk patients. Please refer to the current edition of the AAP's RedBook for recommendations on palivizumab's indications and dosing. 2 2. Nosocomial Prevention: Transmission of RSV and other respiratory viruses occurs by direct inoculation of contagious secretions from the hands or by large-particle droplets into the eyes and nose, but rarely the mouth.20,21 Nosocomial infection may place medically fragile patients at increased risk for morbidity and mortality.22 It is therefore recommended that droplet and contact isolation measures be followed for all patients with bronchiolitis.23 "Droplet Precautions" and "Contact Precautions" signs are to be placed on the patient's door A private room is preferred Patients are not allowed in common areas (i.e., playroom) or other patient rooms A surgical mask is to be worn by all healthcare workers within 3 feet of the patient Protective eyewear is encouraged Strict hand washing should precede and follow all patient encounters and gloves should be worn by all who enter room Impervious cover gowns should be worn when it is anticipated that clothing will have contact with the patient or patient's environment Dedicated patient equipment should remain in the patient's room and not be shared with other patients. A disposable stethoscope provides a sub-optimal auscultory exam. A dedicated stethoscope should remain in the patient’s room and be sanitized upon discharge. General: The basic management of typical bronchiolitis is anchored in the provision of therapies that ensure the patient is clinically stable, well oxygenated, and well hydrated. The main benefits of hospitalization of infants with bronchiolitis are the careful monitoring of clinical status, maintenance of a patent airway (through positioning, suctioning, and mucus clearance), maintenance of adequate hydration, and parental education24-27 (Local Expert Consensus). Diagnosis and Assessment: The diagnosis of bronchiolitis and assessment of its severity is rooted in the clinician’s interpretation of the constellation of characteristic findings and is not dependent on any specific clinical finding or diagnostic test. “Clinicians recognize bronchiolitis as a constellation of clinical symptoms and signs including a viral upper respiratory prodrome followed by increased respiratory effort and wheezing in children less than 2 years of age.”28 (pp1776-7) Clinical signs and symptoms of bronchiolitis may include rhinorrhea, cough, auscultatory findings of wheezing or crackles, tachypnea, and increased respiratory effort manifested by grunting, nasal flaring, and intercostal and/or subcostal retractions. The physical exam reflects the variability in the disease state and benefits from serial observations over time to fully assess 3 the child’s status. Upper airway obstruction may contribute to the work of breathing, and nasal suctioning and positioning of the child may affect the assessment. Other important issues to assess in the patient with bronchiolitis include the impact of respiratory symptoms on feeding and hydration and the response, if any, to therapy. The ability of the family to care for the child and return for further care should also be assessed. A history of underlying conditions such as prematurity, cardiac or pulmonary disease, immunodeficiency, or previous episodes of wheezing should be identified. Several studies have associated premature birth (less than 37 weeks) and young age (less than 6-12 weeks) with an increased risk of severe disease.6,29,30 Other underlying conditions that have been associated with an increased risk of progression to severe disease or mortality include hemodynamically significant congenital heart disease, chronic lung disease (bronchopulmonary dysplasia, cystic fibrosis, congenital anomaly), and the presence of an immunocompromised state.28 Apnea is a specific and important concern in the management of young infants with bronchiolitis, especially with RSV. In a retrospective study of 691 infants younger then 6 months of age hospitalized for bronchiolitis, apnea occurred in 19 (2.7%).31 Risk factors included either (1) history of an apneic event having already occurred or (2) young age, defined as less than 1 month for term infants or a postconceptional age of less than 48 weeks for premature infants. Laboratory and Radiographic Tests: Routine laboratory studies are generally not necessary and may result in increased rates of unnecessary hospital admissions and therapies and unwarranted diagnostic testing. Chest X-Rays are not routinely recommended and should only be obtained as clinically indicated when the diagnosis of bronchiolitis is unclear or when the presentation is severe.13,32-34 Routine testing for the presence of RSV antigen or other viral infections by PCR from nasopharyngeal washings is not recommended for infants >8 weeks of age. Similarly, risk of serious bacterial infection in infants >8 weeks of age with bronchiolitis is extremely low, and so routine cultures of blood and CSF are not recommended.13,14,25,35-40 Those infants not following a typical course may, however, warrant a rapid respiratory panel for diagnostic purposes (Local Expert Consensus). In the infant <8 weeks of age with clinical symptoms of bronchiolitis and a positive RSV antigen, routine blood and spinal fluid cultures are not indicated.41 There is, however, a clinically relevant rate (approximately 5%) of UTI in these infants, thus urinalysis and urine culture should be considered.36,37,42,43 Capillary or arterial blood gas testing is recommended only as clinically indicated for individual patients28 (Local Expert Consensus). 4 Medications: 1. Oxygen therapy is frequently required in the treatment of bronchiolitis. It is recommended that oxygen saturation monitoring be utilized to maintain blood oxygen levels within a normal range. This range is variable in definition and patient specific, though in general adequate arterial oxygen levels are achieved when the oxygen saturation is between 90% and 94%. Therefore, starting supplemental oxygen when the saturation is consistently less than 90% and weaning oxygen when it is consistently higher than 94% is considered reasonable44 See the Monitoring section for recommendation regarding oxygen saturation monitoring. 2. Hypertonic saline In 2008, a Cochrane review stated: “Current evidence suggests nebulized 3% saline may significantly reduce length of stay and improve the clinical severity score in infants with acute viral bronchiolitis.” 45 There are many other studies that suggest hypertonic saline may be of some clinical benefit in bronchiolitis improving clinical scores and length of hospital stay.46-50 However, these studies allowed the use of bronchodilators with the hypertonic saline for fear of inducing bronchospasm as a complication of hypertonic saline as single therapy. One study has recently shown that the overall adverse event rate for single therapy hypertonic saline is relatively low at 1%.51 Hypertonic 3% saline may be used to promote airway clearance. Evidence suggests that adverse events are uncommon, but may result in deterioration of clinical status and bronchiolitis clinical score. If that occurs consideration should be given to stopping this treatment.46,47,51,52 3. Bronchodilators: Although widely used and studied, the efficacy of inhaled bronchodilators in the treatment of bronchiolitis is uncertain, and the published results have been variable. For this reason, multiple evidence-based systemic reviews and meta-analysis studies have been done regarding their use. Based on the evidence reviewed by this committee, bronchodilators should not routinely be used among inpatients as there has been no proven benefit in length of hospital stay or long term clinical outcome.9,28,53-55 Deterioration has been associated with bronchodilator inhalation therapies.56,57 Therefore, if a trial of bronchodilator inhalation therapy is undertaken, and there is no significant improvement in clinical appearance between 15-30 minutes,24,58 it is recommended that the therapy not be continued or repeated (Local Expert Consensus). Inhaled Beta Agonists: From a recent Cochrane review: “Bronchodilators [other than epinephrine] produce small short-term improvements in clinical scores among infants with bronchiolitis and may slightly improve oxygenation in those treated as outpatients. However, given the high costs, incidence of adverse effects and uncertain efficacy based on the findings of this meta-analysis, bronchodilators cannot be recommended for routine management of first time wheezers who present with the clinical findings of 5 bronchiolitis. Bronchodilators should not be used in patients who are hospitalized with bronchiolitis.” 53 (p8) Other studies support that it is reasonable to give a trial of nebulized albuterol therapy with close monitoring for clinical improvement to patients with significant risk factors for asthma. These include a prior history of wheezing or eczema, or a firstdegree relative with asthma. Scheduled or serial use of bronchodilator aerosol therapies is not recommended unless there is documented objective clinical improvement.9,28,54,59,60 Three meta-analysis and several randomized controlled trials have not shown dramatic effects on clinical scores or hospitalization rates from therapy with nebulized albuterol.53,61-63 In the majority of cases the use of inhalation therapies and other treatments effective for treating the bronchospasm characteristic in asthma will not be efficacious for treating the airway edema typical of bronchiolitis.20,24 Inhaled Epinephrine: In 2004, a Cochrane review stated: “There is insufficient evidence to support the use of epinephrine for the treatment of bronchiolitis among inpatients. There is some evidence to suggest that epinephrine may be favorable to salbutamol and placebo among outpatients.”55 (p2) Among the 5 inpatient studies comparing nebulized epinephrine to placebo, only one showed a statistically significant outcome that favored epinephrine. That outcome was an improvement in clinical score at 60 minutes. Among the 4 inpatient studies comparing epinephrine and salbutamol, only one had statistically significant clinical improvement favoring epinephrine. That improvement was a better respiratory rate at 30 minutes. In all studies reviewed, there were no long term clinical improvements favoring epinephrine.55 One older study showed that nebulized racemic epinephrine reduced hospitalizations rates by 59%, but other studies had inconsistent results.57,64-69 Two studies have shown that nebulized epinephrine does not reduce hospital length of stay.57,69 4. Antibiotics are not recommended in the treatment of bronchiolitis unless a specific coexisting bacterial infection has been identified. Multiple randomized controlled trials have shown no benefit in antibiotic use.70-72 A meta-analysis in 2007 again found no evidence to support the use of antibiotics for bronchilitis.73 A recent summary article on the management of bronchilitis does not even mention antibiotics.9 When coexisting bacterial infections are identified (urinary tract infection, acute otitis media) they should be managed in the same manner as in the absence of bronchiolitis. 5. Over-the-counter cough and cold medications are not recommended for routine therapy. There is no evidence to date for their efficacy in the reduction of cough or congestion in infants with upper and lower respiratory tract infections.74-78 The FDA recommends that “these drugs not be used to treat children under 2 years of age because serious and potentially life-threatening side effects can occur.” 79 (p1) 6 6. Steroid therapy given as by inhalation, intravenously, orally, or intramuscularly is not routinely recommended due to a lack of effect on clinical status or on absolute length of stay in the hospital.24-26,80-84 A single study using a high dose of dexamethasone in outpatients with bronchiolitis has shown decreased hospitalization rates in the treated group compared to placebo. However, the side effects and relative risks and benefits with these doses of dexamethasone require further study before advocating routine implementation.85 One large study of 147 infants <24 months of age showed no benefit of prednisolone in the acute phase, at 1 month follow up and 1 year follow up. The conclusion was that such therapy should not be prescribed. 86 A more recent study evaluated the use of high dose inhaled steroids for 3 months after hospitalization for severe RSV infection. The intent was to prevent recurrent wheezing which occurs following severe infection in young infants. No benefit was found and such treatment should not be advocated. 87 A final word of caution should be given concerning steroids in young children. Significant alveolar development occurs in the postnatal lung. Animal studies have demonstrated a deleterious effect on alveolar development with both parenteral and inhaled steroids.88,89 An editorial in the New England Journal of Medicine also warned of possible effects in young children.89 7. Montelukast: It is known that the airway obstruction in viral induced bronchiolitis is due to inflammation. One inflammatory mediator is cysteinyl-leukotriene (cys-LT). Because montelukast is a leukotriene receptor antagonist, there has been interest in using this medication in both treatment for bronchiolitis and in reducing recurrent wheezing after bronchiolitis. A promising pilot study seemed to show a reduction in respiratory symptoms in this population.90 A much larger study by the same authors failed to show any benefit for montelukast in reducing post RSV respiratory symptoms. However, post hoc analysis suggested that a subgroup with more persistent symptoms showed some improvement.91 Another study looked at the reduction in post-RSV respiratory symptoms92 and again failed to show benefit. A single study has looked at the use of montelukast in the treatment of acute bronchiolitis. Although small, no benefit (length of stay, clinical score, and cys-LT levels) was seen in the treatment group.93 Based on these studies, it is recommended to not routinely use montelukast in the treatment of bronchiolitis. A subgroup of patients with persistent symptoms in the months following a severe episode of bronchiolitis might, however, benefit from montelukast Respiratory Care Therapies: 1. It is recommended that the infant be suctioned before feedings, as needed, and prior to any aerosol therapy (Local Expert Consensus). Suction should be performed with either a 7 nasal olive or a bulb syringe. Normal saline drops may be used prior to suctioning (Local Expert Consensus). Deep catheter suctioning should be avoided. 3% saline, given in doses of 4mL nebulized q2 hours x 3, then q4 hours x 5, then q6 hours until discharge, is a reasonable, evidence-based therapy to promote airway clearance in infants with bronchiolitis.46,47 2. Other routine respiratory care therapies are not helpful and are not generally recommended. Chest physiotherapy (CPT) is not recommended.94,95 Cool mist therapy is not recommended.96 Aerosol therapy with normal saline alone is not recommended.56,97,98 Monitoring: Serial clinical assessments by skilled physicians, nurses, and respiratory therapists are the mainstay of monitoring for worsening respiratory distress. Electronic monitoring of heart rate, respiratory rate, and oxygen saturation can provide useful additional clinical data, but may also increase length of stay and impede a patient’s transition to home. 1. Serial assessments using the bronchiolitis respiratory care flow sheet should be used pre- and post-respiratory care intervention. 2. Cardiorespiratory monitors are not routinely recommended for patients with bronchiolitis. 3. Consider cardiorespiratory monitoring for those hospitalized patients at highest risk for apnea during their first 48-hours of illness. Because RSV-associated apnea is usually of short duration, there is no indication for home monitoring after hospitalization.99,100 4. In hospitalized patients, it is recommended that scheduled spot checks of pulse oximetry be utilized in infants with bronchiolitis as opposed to continuous pulse oximetry (Local Expert Consensus). Due to the technical complexity and variability in readings in infants, continuous pulse oximetry may increase duration of hospitalization through unnecessary continuation of supplemental oxygen after resolution of other clinical symptoms.6,101,102 Pulse oximetry has not been shown to be helpful in predicting morbidity or length of stay in wheezing infants or infants with bronchiolitis.103-105 Parent Education 1. Educate parents on the basic pathophysiology and expected clinical course of bronchiolitis, emphasizing that it is a self-limited disease. Refer to Introduction section. 2. Educate parents on the proper techniques for suctioning, airway maintenance, and feeding techniques (Local Expert Consensus). 3. Educate parents about when to call their health care provider by explaining the signs of worsening clinical status: Increasing respiratory rate and work of breathing as indicated by accessory muscle use. Inability to maintain adequate hydration. 8 Worsening general appearance. 4. Infection Control Education Refer to Prevention Section. ED Discharge Criteria Respiratory Status 1. 2. 3. 4. Baby relatively comfortable on room air. Respiratory rate < 70/min. Parents demonstrate ability to perform nasal suctioning. Oxygen saturation is consistently > 90%. Nutritional Status 1. The patient is not dehydrated and demonstrates an ability to feed by mouth. Treatment Modalities 1. Patient is able to tolerate oral medications if indicated. Social 1. Parents demonstrate an understanding of discharge instructions and education on signs of worsening clinical status. Follow Up 1. Patient has a reasonable availability of medical care if respiratory status worsens. Hospital Discharge Criteria Respiratory Status 1. Respiratory rate usually < 70/min and baby relatively comfortable. 2. Parent can clear the infant’s airway using bulb suctioning. 3. Patient is stable in room air with oxygen saturation consistently > 90%. Nutritional Status 1. The patient is on oral feedings at a level to prevent dehydration. Treatment Modalities 1. The patient is on oral medications if indicated. 9 Social 1. Home resources are adequate to support the use of any necessary home therapies. 2. Parent is proficient with therapies required. 3. Family has participated in the processes leading to the discharge decision. Follow Up 1. When indicated, home care and durable medical supply agencies have been notified and arrangements for visits finalized. 2. The primary care provider has been identified, notified, and agrees with discharge decision, and follow-up appointments have been scheduled. Committee: Joel Ledbetter, MD, Annamaria Church, MD, Jennifer Hamm, MD, Kourtney Santucci, MD, and Robert Wood, MD Ad Hoc Committee: Tina Borey, RN, Linda Hill, RT, Toni Karimian, RN, Darcy Knowles, and Alan Kohrt, MD 10 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Wright AL, Taussig LM, Ray CG, Harrison HR, Holberg CJ. The Tucson Children's Respiratory Study. II. Lower respiratory tract illness in the first year of life. Am J Epidemiol. Jun 1989;129(6):1232-1246. Mansbach JM, McAdam AJ, Clark S, et al. Prospective multicenter study of the viral etiology of bronchiolitis in the emergency department. Acad Emerg Med. Feb 2008;15(2):111-118. Swingler GH, Hussey GD, Zwarenstein M. Duration of illness in ambulatory children diagnosed with bronchiolitis. Arch Pediatr Adolesc Med. Oct 2000;154(10):997-1000. van Woensel JB, Kimpen JL, Sprikkelman AB, Ouwehand A, van Aalderen WM. Longterm effects of prednisolone in the acute phase of bronchiolitis caused by respiratory syncytial virus. Pediatr Pulmonol. Aug 2000;30(2):92-96. Kotagal UR, Robbins JM, Kini NM, Schoettker PJ, Atherton HD, Kirschbaum MS. Impact of a bronchiolitis guideline: a multisite demonstration project. Chest. Jun 2002;121(6):1789-1797. Wang EE, Law BJ, Stephens D. Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) prospective study of risk factors and outcomes in patients hospitalized with respiratory syncytial viral lower respiratory tract infection. J Pediatr. Feb 1995;126(2):212-219. Green M, Brayer AF, Schenkman KA, Wald ER. Duration of hospitalization in previously well infants with respiratory syncytial virus infection. Pediatr Infect Dis J. Sep 1989;8(9):601-605. Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ. Bronchiolitisassociated hospitalizations among US children, 1980-1996. JAMA. Oct 20 1999;282(15):1440-1446. Zorc JJ, Hall CB. Bronchiolitis: recent evidence on diagnosis and management. Pediatrics. Feb 2010;125(2):342-349. Todd J, Bertoch D, Dolan S. Use of a large national database for comparative evaluation of the effect of a bronchiolitis/viral pneumonia clinical care guideline on patient outcome and resource utilization. Arch Pediatr Adolesc Med. Nov 2002;156(11):1086-1090. Harrison AM, Boeing NM, Domachowske JB, Piedmonte MR, Kanter RK. Effect of RSV bronchiolitis practice guidelines on resource utilization. Clin Pediatr (Phila). Sep 2001;40(9):489-495. Perlstein PH, Kotagal UR, Schoettker PJ, et al. Sustaining the implementation of an evidence-based guideline for bronchiolitis. Arch Pediatr Adolesc Med. Oct 2000;154(10):1001-1007. El-Radhi AS, Barry W, Patel S. Association of fever and severe clinical course in bronchiolitis. Arch Dis Child. Sep 1999;81(3):231-234. Liebelt EL, Qi K, Harvey K. Diagnostic testing for serious bacterial infections in infants aged 90 days or younger with bronchiolitis. Arch Pediatr Adolesc Med. May 1999;153(5):525-530. Perlstein PH, Kotagal UR, Bolling C, et al. Evaluation of an evidence-based guideline for bronchiolitis. Pediatrics. Dec 1999;104(6):1334-1341. 11 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. Boyce TG, Mellen BG, Mitchel EF, Jr., Wright PF, Griffin MR. Rates of hospitalization for respiratory syncytial virus infection among children in medicaid. J Pediatr. Dec 2000;137(6):865-870. Church NR, Anas NG, Hall CB, Brooks JG. Respiratory syncytial virus-related apnea in infants. Demographics and outcome. Am J Dis Child. Mar 1984;138(3):247-250. Joffe S, Escobar GJ, Black SB, Armstrong MA, Lieu TA. Rehospitalization for respiratory syncytial virus among premature infants. Pediatrics. Oct 1999;104(4 Pt 1):894-899. Shay DK, Holman RC, Roosevelt GE, Clarke MJ, Anderson LJ. Bronchiolitis-associated mortality and estimates of respiratory syncytial virus-associated deaths among US children, 1979-1997. J Infect Dis. Jan 1 2001;183(1):16-22. Hall CB. Respiratory syncytial virus and parainfluenza virus. N Engl J Med. Jun 21 2001;344(25):1917-1928. Hall CB, Douglas RG, Jr., Schnabel KC, Geiman JM. Infectivity of respiratory syncytial virus by various routes of inoculation. Infect Immun. Sep 1981;33(3):779-783. Langley JM, LeBlanc JC, Wang EE, et al. Nosocomial respiratory syncytial virus infection in Canadian pediatric hospitals: a Pediatric Investigators Collaborative Network on Infections in Canada Study. Pediatrics. Dec 1997;100(6):943-946. Erlanger Health System. Policy and Procedure: Isolation Precautions. 8304.075. 2008. Klassen TP. Recent advances in the treatment of bronchiolitis and laryngitis. Pediatr Clin North Am. Feb 1997;44(1):249-261. Lugo RA, Nahata MC. Pathogenesis and treatment of bronchiolitis. Clin Pharm. Feb 1993;12(2):95-116. Panitch HB, Callahan CW, Jr., Schidlow DV. Bronchiolitis in children. Clin Chest Med. Dec 1993;14(4):715-731. Nicolai T, Pohl A. Acute viral bronchiolitis in infancy: epidemiology and management. Lung. 1990;168 Suppl:396-405. American Academy of Pediatrics. Subcommitte on the Diagnosis and Management of Bronchiolitis. Diagnosis and Management of Bronchiolitis. Pediatrics. 2006;118(4):1774-1793. Chan PW, Lok FY, Khatijah SB. Risk factors for hypoxemia and respiratory failure in respiratory syncytial virus bronchiolitis. Southeast Asian J Trop Med Public Health. Dec 2002;33(4):806-810. Shaw KN, Bell LM, Sherman NH. Outpatient assessment of infants with bronchiolitis. Am J Dis Child. Feb 1991;145(2):151-155. Willwerth BM, Harper MB, Greenes DS. Identifying hospitalized infants who have bronchiolitis and are at high risk for apnea. Ann Emerg Med. Oct 2006;48(4):441-447. Schuh S, Lalani A, Allen U, et al. Evaluation of the utility of radiography in acute bronchiolitis. J Pediatr. Apr 2007;150(4):429-433. Roback MG, Dreitlein DA. Chest radiograph in the evaluation of first time wheezing episodes: review of current clinical practice and efficacy. Pediatr Emerg Care. Jun 1998;14(3):181-184. Swingler GH, Hussey GD, Zwarenstein M. Randomised controlled trial of clinical outcome after chest radiograph in ambulatory acute lower-respiratory infection in children. Lancet. Feb 7 1998;351(9100):404-408. 12 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. Luginbuhl LM, Newman TB, Pantell RH, Finch SA, Wasserman RC. Office-Based Treatment and Outcomes for Febrile Infants With Clinically Diagnosed Bronchiolitis. Pediatrics. November 1, 2008 2008;122(5):947-954. Antonow JA, Hansen K, McKinstry CA, Byington CL. Sepsis evaluations in hospitalized infants with bronchiolitis. Pediatr Infect Dis J. Mar 1998;17(3):231-236. Kuppermann N, Bank DE, Walton EA, Senac MO, Jr., McCaslin I. Risks for bacteremia and urinary tract infections in young febrile children with bronchiolitis. Arch Pediatr Adolesc Med. Dec 1997;151(12):1207-1214. Schwartz R. Respiratory syncytial virus in infants and children. Nurse Pract. Sep 1995;20(9):24-29. Chiocca EM. RSV and the high-risk infant. Pediatr Nurs. Nov-Dec 1994;20(6):565-568. Stark JM, Busse WW. Respiratory virus infection and airway hyperreactivity in children. Pediatric Allergy and Immunology. 1991;2(3):95-110. Titus MO, Wright SW. Prevalence of serious bacterial infections in febrile infants with respiratory syncytial virus infection. Pediatrics. Aug 2003;112(2):282-284. Purcell K, Fergie J. Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections. Arch Pediatr Adolesc Med. Apr 2002;156(4):322-324. Levine DA, Platt SL, Dayan PS, et al. Risk of Serious Bacterial Infection in Young Febrile Infants With Respiratory Syncytial Virus Infections. Pediatrics. June 1, 2004 2004;113(6):1728-1734. National Asthma Education and Prevention Program. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda (MD): National Institutes of Health; 1997: NIH Pub. No. 97-4051. Zhang L, Mendoza-Sassi RA, Wainwright C, Klassen TP. Nebulized hypertonic saline solution for acute bronchiolitis in infants. Cochrane Database Syst Rev. 2008(4):CD006458. Dubik M. Nebulized Hypertonic Saline as a Treatment for Bronchiolitis. AAP Grand Rounds. December 1, 2007 2007;18(6):63-64. Kuzik BA, Al-Qadhi SA, Kent S, et al. Nebulized hypertonic saline in the treatment of viral bronchiolitis in infants. J Pediatr. Sep 2007;151(3):266-270, 270 e261. Luo Z, Liu E, Luo J, et al. Nebulized hypertonic saline/salbutamol solution treatment in hospitalized children with mild to moderate bronchiolitis. Pediatr Int. Apr 2010;52(2):199-202. Tal G, Cesar K, Oron A, Houri S, Ballin A, Mandelberg A. Hypertonic saline/epinephrine treatment in hospitalized infants with viral bronchiolitis reduces hospitalization stay: 2 years experience. Isr Med Assoc J. Mar 2006;8(3):169-173. Weinberger M. Bronchiolitis in Hospital: Nebulized Hypertonic Saline/Salbutamol? AAP Grand Rounds. February 1, 2010 2010;23(2):16-. Ralston S, Hill V, Martinez M. Nebulized Hypertonic Saline Without Adjunctive Bronchodilators for Children With Bronchiolitis. Pediatrics. 2010;126(3):e520-525. Conway E, Schoettker PJ, Moore A, Britto MT, Kotagal UR, Rich K. Empowering respiratory therapists to take a more active role in delivering quality care for infants with bronchiolitis. Respir Care. Jun 2004;49(6):589-599. Gadomski AM, Bhasale AL. Bronchodilators for bronchiolitis. Cochrane Database Syst Rev. 2006;3:CD001266. 13 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. 70. 71. Petruzella FD, Gorelick MH. Current therapies in bronchiolitis. Pediatr Emerg Care. Apr 2010;26(4):302-307; quiz 308-311. Hartling L, Wiebe N, Russell K, Patel H, Klassen TP. Epinephrine for bronchiolitis. Cochrane Database Syst Rev. 2004(1):CD003123. Ho L, Collis G, Landau LI, Le Souef PN. Effect of salbutamol on oxygen saturation in bronchiolitis. Arch Dis Child. Sep 1991;66(9):1061-1064. Wainwright C, Altamirano L, Cheney M, et al. A Multicenter, Randomized, DoubleBlind, Controlled Trial of Nebulized Epinephrine in Infants with Acute Bronchiolitis. New England Journal of Medicine. 2003;349(1):27-35. Bausch and Lomb Pharmaceuticals. Drug Package Insert:Albuterol Sulfate Inhalation Solution, 0.5%*. Tampa2008. Pate BM. Assessment of Pharmacologic Therapies and Diagnostic Tests for Viral Bronchiolitis: Drugs and Tests Appear to Be of No Value. AAP Grand Rounds. July 1, 2004 2004;12(1):3-4. King VJ, Viswanathan M, Bordley WC, et al. Pharmacologic treatment of bronchiolitis in infants and children: a systematic review. Arch Pediatr Adolesc Med. Feb 2004;158(2):127-137. Flores G, Horwitz RI. Efficacy of beta2-agonists in bronchiolitis: a reappraisal and metaanalysis. Pediatrics. Aug 1997;100(2 Pt 1):233-239. Gadomski AM, Lichenstein R, Horton L, King J, Keane V, Permutt T. Efficacy of albuterol in the management of bronchiolitis. Pediatrics. Jun 1994;93(6 Pt 1):907-912. Kellner JD, Ohlsson A, Gadomski AM, Wang EE. Efficacy of bronchodilator therapy in bronchiolitis. A meta-analysis. Arch Pediatr Adolesc Med. Nov 1996;150(11):1166-1172. Menon K, Sutcliffe T, Klassen TP. A randomized trial comparing the efficacy of epinephrine with salbutamol in the treatment of acute bronchiolitis. J Pediatr. Jun 1995;126(6):1004-1007. Reijonen T, Korppi M, Pitkakangas S, Tenhola S, Remes K. The clinical efficacy of nebulized racemic epinephrine and albuterol in acute bronchiolitis. Arch Pediatr Adolesc Med. Jun 1995;149(6):686-692. Kristjansson S, Lodrup Carlsen KC, Wennergren G, Strannegard IL, Carlsen KH. Nebulised racemic adrenaline in the treatment of acute bronchiolitis in infants and toddlers. Arch Dis Child. Dec 1993;69(6):650-654. Numa AH, Williams GD, Dakin CJ. The effect of nebulized epinephrine on respiratory mechanics and gas exchange in bronchiolitis. Am J Respir Crit Care Med. Jul 1 2001;164(1):86-91. Sanchez I, De Koster J, Powell RE, Wolstein R, Chernick V. Effect of racemic epinephrine and salbutamol on clinical score and pulmonary mechanics in infants with bronchiolitis. J Pediatr. Jan 1993;122(1):145-151. Abul-Ainine A, Luyt D. Short term effects of adrenaline in bronchiolitis: a randomised controlled trial. Arch Dis Child. Apr 2002;86(4):276-279. Field CM, Connolly JH, Murtagh G, Slattery CM, Turkington EE. Antibiotic treatment of epidemic bronchiolitis--a double-blind trial. Br Med J. Jan 8 1966;1(5479):83-85. Friis B, Andersen P, Brenoe E, et al. Antibiotic treatment of pneumonia and bronchiolitis. A prospective randomised study. Arch Dis Child. Nov 1984;59(11):1038-1045. 14 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. 87. 88. 89. Kabir AR, Mollah AH, Anwar KS, Rahman AK, Amin R, Rahman ME. Management of bronchiolitis without antibiotics: a multicentre randomized control trial in Bangladesh. Acta Paediatr. Oct 2009;98(10):1593-1599. Spurling GK, Fonseka K, Doust J, Del Mar C. Antibiotics for bronchiolitis in children. Cochrane Database Syst Rev. 2007(1):CD005189. Clemens CJ, Taylor JA, Almquist JR, Quinn HC, Mehta A, Naylor GS. Is an antihistamine-decongestant combination effective in temporarily relieving symptoms of the common cold in preschool children? J Pediatr. Mar 1997;130(3):463-466. Hutton N, Wilson MH, Mellits ED, et al. Effectiveness of an antihistamine-decongestant combination for young children with the common cold: a randomized, controlled clinical trial. J Pediatr. Jan 1991;118(1):125-130. American Academy of Pediatrics. Committee on Drugs. Use of Codeine- and Dextromethorphan-Containing Cough Syrups in Pediatrics. Pediatrics. 1978;62(1):118122. American Academy of Pediatrics. Committee on Drugs. Use of codeine- and dextromethorpan-containing cough remedies in children. Pediatrics. 1997;99(6):919. Gadomski A, Horton L. The need for rational therapeutics in the use of cough and cold medicine in infants. Pediatrics. Apr 1992;89(4 Pt 2):774-776. U.S. Food and Drug Administration. Public Health Advisory: FDA Recommends that Over-the-Counter (OTC) Cough and Cold Products not be used for Infants and Children under 2 Years of Age. Silver Spring, MD: U.S. Department of Health and Human Services; 2010. Cade A, Brownlee KG, Conway SP, et al. Randomised placebo controlled trial of nebulised corticosteroids in acute respiratory syncytial viral bronchiolitis. Arch Dis Child. Feb 2000;82(2):126-130. Garrison MM, Christakis DA, Harvey E, Cummings P, Davis RL. Systemic corticosteroids in infant bronchiolitis: A meta-analysis. Pediatrics. Apr 2000;105(4):E44. Richter H, Seddon P. Early nebulized budesonide in the treatment of bronchiolitis and the prevention of postbronchiolitic wheezing. J Pediatr. May 1998;132(5):849-853. De Boeck K, Van der Aa N, Van Lierde S, Corbeel L, Eeckels R. Respiratory syncytial virus bronchiolitis: a double-blind dexamethasone efficacy study. J Pediatr. Dec 1997;131(6):919-921. Roosevelt G, Sheehan K, Grupp-Phelan J, Tanz RR, Listernick R. Dexamethasone in bronchiolitis: a randomised controlled trial. Lancet. Aug 3 1996;348(9023):292-295. Schuh S, Coates AL, Binnie R, et al. Efficacy of oral dexamethasone in outpatients with acute bronchiolitis. J Pediatr. Jan 2002;140(1):27-32. Bulow SM, Nir M, Levin E, et al. Prednisolone treatment of respiratory syncytial virus infection: a randomized controlled trial of 147 infants. Pediatrics. Dec 1999;104(6):e77. Ermers MJ, Rovers MM, van Woensel JB, Kimpen JL, Bont LJ. The effect of high dose inhaled corticosteroids on wheeze in infants after respiratory syncytial virus infection: randomised double blind placebo controlled trial. BMJ. 2009;338:b897. Kovar J, Willet KE, Hislop A, Sly PD. Impact of postnatal glucocorticoids on early lung development. J Appl Physiol. Mar 2005;98(3):881-888. Zhang H, Garber SJ, Cui Z, et al. The angiogenic factor midkine is regulated by dexamethasone and retinoic acid during alveolarization and in alveolar epithelial cells. Respir Res. 2009;10:77. 15 90. 91. 92. 93. 94. 95. 96. 97. 98. 99. 100. 101. 102. 103. 104. 105. Bisgaard H. A randomized trial of montelukast in respiratory syncytial virus postbronchiolitis. Am J Respir Crit Care Med. Feb 1 2003;167(3):379-383. Bisgaard H, Flores-Nunez A, Goh A, et al. Study of montelukast for the treatment of respiratory symptoms of post-respiratory syncytial virus bronchiolitis in children. Am J Respir Crit Care Med. Oct 15 2008;178(8):854-860. Proesmans M, Sauer K, Govaere E, Raes M, De Bilderling G, De Boeck K. Montelukast does not prevent reactive airway disease in young children hospitalized for RSV bronchiolitis. Acta Paediatr. Nov 2009;98(11):1830-1834. Amirav I, Luder AS, Kruger N, et al. A double-blind, placebo-controlled, randomized trial of montelukast for acute bronchiolitis. Pediatrics. Dec 2008;122(6):e1249-1255. Nicholas KJ, Dhouieb MO, Marshall TG, Edmunds AT, Grant MB. An Evaluation of Chest Physiotherapy in the Management of Acute Bronchiolitis: Changing clinical practice. Physiotherapy. 1999;85(12):669-674. Webb MS, Martin JA, Cartlidge PH, Ng YK, Wright NA. Chest physiotherapy in acute bronchiolitis. Arch Dis Child. Nov 1985;60(11):1078-1079. Gibson LE. Use of water vapor in the treatment of lower respiratory disease. Am Rev Respir Dis. Dec 1974;110(6 Pt 2):100-103. Gadomski AM, Aref GH, el Din OB, el Sawy IH, Khallaf N, Black RE. Oral versus nebulized albuterol in the management of bronchiolitis in Egypt. J Pediatr. Jan 1994;124(1):131-138. Chowdhury D, al Howasi M, Khalil M, al-Frayh AS, Chowdhury S, Ramia S. The role of bronchodilators in the management of bronchiolitis: a clinical trial. Ann Trop Paediatr. 1995;15(1):77-84. Kneyber MC, Brandenburg AH, de Groot R, et al. Risk factors for respiratory syncytial virus associated apnoea. Eur J Pediatr. Apr 1998;157(4):331-335. Anas N, Boettrich C, Hall CB, Brooks JG. The association of apnea and respiratory syncytial virus infection in infants. J Pediatr. Jul 1982;101(1):65-68. Brooks AM, McBride JT, McConnochie KM, Aviram M, Long C, Hall CB. Predicting deterioration in previously healthy infants hospitalized with respiratory syncytial virus infection. Pediatrics. Sep 1999;104(3 Pt 1):463-467. Unger S, Cunningham S. Effect of oxygen supplementation on length of stay for infants hospitalized with acute viral bronchiolitis. Pediatrics. Mar 2008;121(3):470-475. Bishop J, Nolan T. Pulse oximetry in acute asthma. Arch Dis Child. Jun 1991;66(6):724725. Mallory MD, Shay DK, Garrett J, Bordley WC. Bronchiolitis management preferences and the influence of pulse oximetry and respiratory rate on the decision to admit. Pediatrics. Jan 2003;111(1):e45-51. McMillan JA, Tristram DA, Weiner LB, Higgins AP, Sandstrom C, Brandon R. Prediction of the duration of hospitalization in patients with respiratory syncytial virus infection: use of clinical parameters. Pediatrics. Jan 1988;81(1):22-26. 16