02-ACLS - WordPress.com

ACLS
1.
Keep up to date with ACLS recommendations
2.
Promptly defibrillate a patient with V. fib or pulseless/symptomatic V. tach.
3.
Diagnose serious arrhythmias (e.g. V. tach, V. fib, SVT, A. fib, or 2 nd /3 rd degree heart block), and treat according to ACLS protocol.
4.
Suspect and promptly treat reversible causes of arrhythmias (e.g. hyperkalemia, digoxin toxicity, cocaine intoxication) before confirmation of the diagnosis.
5.
Ensure adequate ventilation (i.e. with a bag valve mask) and secure the airway in a timely manner.
6.
In patients requiring resuscitation, consider their circumstances (e.g. asystole, long code times, pre-code prognosis, living wills) to help you to decide when to stop (e.g. avoid inappropriate resuscitation)
7.
In patients with serious medical problems or end stage disease, discuss code status and end of life decisions (e.g. resuscitation, feeding tubes, level of treatment) and readdress these issues periodically.
8.
Attend to family members (e.g. with counseling, attendance in the code room) during and after resuscitating a patient.
9.
In a pediatric resuscitation, use appropriate resources (e.g. Braeslow tape, the patient’s weight)to determine the correct drug doses and tube size.
Basic Approach
Pulseless Arrest
1. C-B-A -D-E does patient have a pulse? (dead or alive- less than 10 sec)
2010 guidelines recommend early CPR...therefore a change from ABCs to CBA...
2. Call for help/ code
3. No pulse, start Chest compressions
CPR Quality
• Push hard (≥2 inches [5 cm]) and fast (≥100/min) and allow complete chest recoil
• Minimize interruptions in compressions
• Avoid excessive ventilation
• Rotate compressor every 2 minutes
• If no advanced airway, 30:2 compression-ventilation ratio
• Quantitative waveform capnography
– If Petco2 <10 mm Hg, attempt to improve CPR quality
• Intra-arterial pressure
– If relaxation phase (diastolic) pressure <20 mm Hg, attempt to improve CPR quality
4. Attach leads and identify rhythm (VOICE- vitals, O2, IV, cardiac monitor and equipment)
5. Shockable or not shockable rhythm (minimize time off CPR)
Shock Energy
• Biphasic: Manufacturer recommendation (120-200 J); if unknown, use maximum available. Second and subsequent doses should be equivalent, and higher doses may be considered.
• Monophasic: 360 J
6. Drug Therapy
• Epinephrine IV/IO Dose: 1 mg every 3-5 minutes
• Vasopressin IV/IO Dose: 40 units can replace first or second dose of epinephrine
• Amiodarone IV/IO Dose: First dose: 300 mg bolus. Second dose: 150 mg.
- Atropine is no longer given routinely for slow PEA and asystole
7. Treat reversible causes
Hypothermia: keep patient warm
Hypovolemia: fluids, stop bleeding
Hypoglycemia: check blood glucose
Hyper/HypoKalemia: lytes and treat if present
Hypoxia: make sure adequate oxygenation and ventilation
H+: lytes, blood gases and consider bicarb
Toxins: think about digoxin
Tamponade: US to heart
Thrombus: MI or PE
Tension Pneumo: trachea midline, air entry
Trauma: look for signs of trauma and related injuries
Advanced Airway
• Supraglottic advanced airway or endotracheal intubation
• Waveform capnography to confirm and monitor ET tube placement
• 8-10 breaths per minute with continuous chest compressions
Return of Spontaneous Circulation (ROSC)
• Pulse and blood pressure
• Abrupt sustained increase in Petco2 (typically ≥40 mm Hg)
• Spontaneous arterial pressure waves with intra-arterial monitoring
PEA/ Asystole or VF/pulseless VT: see new circular algorithm on page 14: http://www.heart.org/idc/groups/heartpublic/@wcm/@ecc/documents/downloadable/ucm_317350.pdf
If they have a pulse:
1. Slow or Fast
2. P waves or no P waves
3. Regular or Irregular
4. Wide or Narrow
5. Stable or Unstable
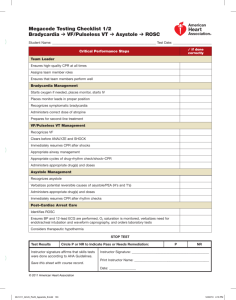
Bradycardia algorithm:
2010: For the treatment of the adult with symptomatic and unstable bradycardia, chronotropic drug infusions are recommended as an alternative to pacing.
If HR slow- atropine 0.5mg IV push, dopamine infusion 2-10mcg/kg/min, epinephrine infusion 2-10mcg/kg/min
Transcutaneous pacing- set at a rate of 60bpm or faster than underlying rhythm, 2mA > than capture, use femoral pulse to assess if perfusing as carotid can move with pacing.
Transvenous pacing
The major ECG rhythms classified as bradycardia include: Sinus Bradycardia, First-degree AV block, Second-degree AV block- Type I —Wenckenbach/Mobitz II- Type II —Mobitz II, Third-degree AV block complete block
Tachycardia algorithm:
The algorithm for treatment of tachycardia with pulses has been simplified. Adenosine is recommended in the initial diagnosis and treatment of stable, undifferentiated regular, monomorphic wide-complex tachycardia (this is also consistent in ACLS and PALS recommendations). It is important to note that adenosine should not be used for irregular wide-complex tachycardias because it may cause degeneration of the rhythm to VF.
With children : use the Breslow tape
In all patients: discuss code status, involve the family when appropriate, evaluate prognosis and avoid inappropriate resuscitation
Initial and Later Key Objectives of Post–Cardiac Arrest Care (New to 2010 guidelines)
1. Optimize cardiopulmonary function and vital organ perfusion after ROSC
2. Transport/transfer to an appropriate hospital or critical care unit with a comprehensive post–cardiac arrest treatment system of care
3. Identify and treat ACS and other reversible causes
4. Control temperature to optimize neurologic recovery
5. Anticipate, treat, and prevent multiple organ dysfunction. This includes avoiding excessive ventilation and hyperoxia.
REFERENCES:
2010 Guidelines: http://circ.ahajournals.org/content/vol122/18_suppl_3/#_____AMERICAN_HEART_ASSOCIATION_GUIDELINES_FOR_CARDIOPULMONARY_RESUSCITAT
ION_AND_EMERGENCY_CARDIOVASCULAR_CARE_SCIENCE http://www.heart.org/idc/groups/heart-public/@wcm/@ecc/documents/downloadable/ucm_317350.pdf
ACLS Simulator: http://acls-algorithms.com/2010-acls-guidelines
EM Crit Podcast (20minreview): http://emcrit.org/podcasts/acls-guidelines-2010/ (good summary notes and worth listening to)
NITIAL APPROACH TO CRITICALLY ILL PATIENT :
A - B - C
I – IV : 2 large bore, NS, wide open
M – Monitors: O2 Sat, ECG, BP
F – Foley
I
– Investigations
N – NG tube
E
– ‘Ex’-Rays (Abdomen, CXR), Imaging
* Always synchronize when patient has a pulse!
PEA\Asystolie : PEA = P-
Problem (H’s and T’s),
EEpi, AAtropine
V-TACH \ V-FIB: SCREAM = SShock, C -CPR, RRythm check, EEpi, A -Amiodarone, MMagnesium ( for torsades )
SHOCK: Biphasic: 120-200 J Monophasic: 360 J
Epi IV\IO: 1mg q3-5 minutes
Vasopressin IV\IO : 40u can replace 1 st or 2 nd dose of Epi
Amiodarone IV\IO : 1 st dose: 300mg bolus, 2 nd dose: 150mg
* Braeslow tape (for pediatric doses)
CAUSES:
H’s: Hypovolemia, Hypoxia, Hyper\Hypokalemia, Hypoglycemia, Hypothermia, Hydrogen ion (acidosis)
T’s: Trauma, Tamponnade, Thrombus (pulmonary\coronary), Tension pneumo, Toxins
Metoprolol: Uncontrolled Afib:
I.V.: 2.5-5 mg every 2-5 minutes (maximum total dose: 15 mg over a 10-
15 minute period). Note: Initiate cautiously in patients with concomitant heart failure; avoid in patients with decompensated heart failure.
POST-MI MEDS : ASO-BETO-STATO-PRIL
* Sprionolactone saves lives in CHF patients (stage 3-4)