Warfarin Management Guidelines
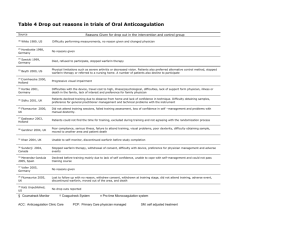
advertisement

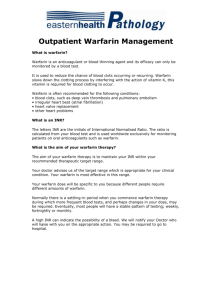
WARFARIN MANAGEMENT GUIDELINES WARFARIN WISE FEBRUARY 2006 LIVERPOOL HOSPITAL DEVELOPED AS PART OF THE “SAFER SYSTEMS SAVING LIVES “ PROJECT. WARFARIN MANAGEMENT IN ACUTE STROKE PATIENTS TABLE OF CONTENTS ANTI-COAGULATION USING WARFARIN ........................................................ 1 OUTCOME ................................................................................................................ 1 GUIDELINES ............................................................................................................. 1 1. 2. 3. 4. 5. 6. PRESCRIBING AND ADMINISTRATION ......................................................................... 1 MONITORING ........................................................................................................... 2 DRUG INTERACTIONS .............................................................................................. 2 INR GREATER THAN THERAPEUTIC RANGE ............................................................... 3 DISCHARGE INSTRUCTIONS ...................................................................................... 3 RENAL IMPAIRMENT ................................................................................................. 4 COMPILED BY ........................................................................................................... 5 PATIENT EDUCATION & DISCHARGE MANAGEMENT ....................................... 6 WARFARIN THERAPY CHART ....................................................................... 7 DISCHARGE CHECKLIST .............................................................................. 8 WARFARIN ALERT CARD SAMPLE ............................................................................... 8 WARFARIN: IMPORTANT INFORMATION FOR PATIENTS .................................... 9 WARFARIN ALERT CARD ............................................................................................ 9 INR BLOOD TESTS.................................................................................................... 9 WARFARIN ............................................................................................................... 9 WARFARIN DOSE ...................................................................................................... 9 ADMINISTRATION TIME............................................................................................... 9 LABORATORY TESTS ................................................................................................. 9 OTHER MEDICATIONS .............................................................................................. 10 DIETARY PRINCIPLES .............................................................................................. 10 SURGICAL PROCEDURES ......................................................................................... 10 TRAVEL .................................................................................................................. 10 PREGNANCY ........................................................................................................... 10 SIGNS OF BLEEDING ................................................................................................ 10 D:\106741972.doc Table of Contents ANTI-COAGULATION USING WARFARIN OUTCOME To promote therapeutic anti-coagulant levels the following guidelines should be implemented to minimise the risk of bleeding and thromboembolism. GUIDELINES COUMADIN® is the preferred brand of Warfarin at Liverpool Health Service. Coumadin will be supplied for all inpatients starting Warfarin. Patients already on the Marevan® brand should use their own tablets, as Marevan and Coumadin are NOT EQUIVALENT. Reference: Aust Prescriber Vol 21 No. 3 1998. 1. PRESCRIBING AND ADMINISTRATION The prescribing doctor will write the indication for Warfarin, the duration of Warfarin therapy and the desired therapeutic INR range on the ‘Warfarin Therapy Chart’ (Page 7). For chronic AF and valve replacements, start Warfarin alone. For restarting Warfarin postoperatively, restart patient on ‘usual’ pre-operative maintenance dose - do not reload. For acute DVT or PE, start Warfarin on the same day as Heparin/Low Molecular Weight Heparin (LMWH) (see Table 4). It is generally recommended to overlap Heparin/LMWH with Warfarin for a minimum of five (5) days and until the INR is >2.0 for at least two (2) consecutive days. Assess each patient for risk factors for increased sensitivity to warfarin and therefore bleeding: Risk factors include: > 'frail' elderly; > low body weight; > abnormal liver function tests including albumin; > INR 1.4; > any other bleeding risk such as severe heart failure or low platelets; and > concomitant drugs which increase the effect of Warfarin (see Table 2). If no risk factors exist, start Warfarin at 5mg daily, monitor INR daily and adjust dose using the nomogram in Table 1. If risk factors exist, consider smaller loading doses (2 - 4mg) and seek senior/specialist advice. Monitor INR daily. High loading doses such as 10 mg should not be used as they may increase the risk of bleeding. Warfarin is to be administered at 1800 hours and must be prescribed before that time. Aged adjusted commencing dose: > 60 to 70 years - 4.5mg/day > 70 to 80 years - 4.0mg/day > 80 to 90 years - 3.5mg/day (Source: Sullivan Nicholaides Pathology) Liverpool Stroke Unit Warfarin Management guidelines adapted from the Alfred Hospital Melbourne, Yarrawonga Health Service and Armidale Health Service, WA by the” Safer Systems Saving Lives” project. Warfarin management in acute stroke patients. February 2006 Page 1 of 10 (If Pre-Treatment INR, Hepatic Function and Serum Albumin are Normal) Day INR Dose <1.4 5 mg 1 TABLE 1 Dosage Adjustment in a Patient Starting Warfarin 2 Ensure the Patient is Entering Warfarin Dose and INR in the Warfarin Booklet and has Acknowledged Education (See Page 6) 3 Based on Gedge et al a Comparison of a Low Dose Warfarin Induction Regimen with the Modified Fennerty Regimen in Elderly Patients [Age Ageing 2000; 29:31-4] <1.8 1.8 to 2.0 >2.0 <2.0 2.0 to2.5 2.6 to2.9 3.0 to3.2 3.3 to3.5 >3.5 <1.4 1.4 to 1.5 1.6 to 1.7 1.8 to 1.9 2.0 to 2.3 2.4 to 3.0 3.1 to 3.2 3.3 to 3.5 >3.5 4 5 mg 1 mg Nil 5 mg 4 mg 3 mg 2 mg 1 mg Nil 10 mg 7 mg 6 mg 5 mg 4 mg 3 mg 2 mg 1 mg Nil Dosage Adjustment After Day 4 Depends on Clinical Judgement 2. MONITORING Daily INR monitoring and warfarin dose adjustment is necessary until the INR is therapeutic and stable. Blood should be collected for INR on the morning blood collection round. (Write Request Form previous day.) 3. DRUG INTERACTIONS Certain drugs may increase or decrease the effect of Warfarin and the risk of bleeding/ thrombosis (Table 2). When starting or stopping a drug, particularly antibiotics, the INR must be checked 1 to 2 days after the change in therapy. SOME MAJOR DRUG INTERACTIONS WITH WARFARIN TABLE 2 INCREASED DECREASED Effect of Warfarin Anti-Platelet Agents Analgesics Abciximab (ReoPro), Aspirin, Paracetamol (Large Dipyridamole, NSAIDs, Doses ie. 4 to 7g Per Clopidogrel, Tirofiban Week), Tramadol COX-2 Inhibitors Anticonvulsants Celecoxib, Rofecoxib Phenytoin Check with Pharmacy or Via Clinicians Health Channel (Micromedex) if More Information Required Antibiotics Cephalosporins, Macrolides, Metronidazole, Sulphonamides, Quinolones, Vancomycin Antifungals Itraconazole, Fluconazole, Ketoconazole Antiarrythmics Amiodarone, Mexiletine, Verapamil Herbal Medicines Dong Quai, Garlic, Papaya, St Johns Wort, Ginkgo, Ginger and Garlic (Large Amounts), Guarana Selective Serotonin Reuptake Inhibitors Fluoxetine Effect of Warfarin Ascorbic Acid (Large Doses) Vitamin K Anticonvulsants Carbamazepine, Phenytoin Antibiotics Rifampicin, Rifabutin Tricyclic Antidepressants Sedatives Barbiturates Raloxifene, Tamoxifen Quinine and Quinidine Herbal Medicines Ginseng, Slippery Elm Bark, Green Tea, Co-Enzyme Q10 Liverpool Stroke Unit Warfarin Management guidelines adapted from the Alfred Hospital Melbourne, Yarrawonga Health Service and Armidale Health Service, WA by the” Safer Systems Saving Lives” project. Warfarin management in acute stroke patients. February 2006 Page 2 of 10 4. INR GREATER THAN THERAPEUTIC RANGE If INR is greater than the therapeutic range, see Table 3 for management. Contact prescribing doctor if INR > 6 and / or there is any bleeding during Warfarin therapy. TABLE 3 : BLEEDING NO YES INR < 5 INR >5 TO <9 INR >9 Withhold Warfarin Check INR at 24 Hours (No Vitamin K) Resume Warfarin at Lower Dose when INR is In Therapeutic Range Withhold Warfarin Give 2mg Vitamin K (Oral) Withhold Warfarin and Give 5mgVitamin (IV) OR IF Rapid Reversal Necessary Give 4mg Vitamin K (Oral) Check INR at 6 Hours If Rapid Reversal Necessary (ie. Surgery) Give 2mg Vitamin K (Oral) Check INR at 24 Hours If INR >4 Give 2mg Vitamin K (Oral) Resume Warfarin at Lower Dose When In Therapeutic Range INR >15 OR Life Threatening Bleeding or Warfarin Overdose Give 10mg Vitamin K (IV) Supplement with FFP If INR >4 Check INR at 6 Hours Give 5mg Vitamin K (IV) If INR >4 Recheck at 6 Hours Then Daily for Three (3) Days (If INR Rises LMO to Assess) Resume Warfarin at Lower Dose When In Therapeutic Range Give 10mg Vitamin K (IV) Recheck INR at 6 Hours Then Daily for Three (3) Days If INR >4 LMO to Assess Repeat Vitamin K as Necessary Oral Vitamin K tablets should not be used as only 10mg tablets are available. Use the IV injection (Konakion MM) solution orally. For oral administration give undiluted. For some conditions such as prosthetic heart valves, the degree of reversal must be decided on an individual basis. All patients with bleeding should be evaluated to identify local anatomical reasons for bleeding. It may be advisable to consult HMO. NOTE: Clinical judgement to be used when assessing a patient’s severity to bleeding. Heparin to be initiated when Vitamin K has been administered in excessive doses making the patient unresponsive to Warfarin therapy. Heparin to be continued until Warfarin becomes therapeutic. Notes on Vitamin K Administration: Use of Vitamin K may be followed by a period of Warfarin resistance. If after cessation of bleeding, anti-coagulation is once again necessary, eg. in patients with mechanical heart valves, Heparin may be required until INR levels are once again therapeutic. Do not mix ampoules of Vitamin K with other infusion solutions. 5. DISCHARGE INSTRUCTIONS Discharging Medical Officer is responsible for Discharge Summary. Information to include: > > > > target INR; Warfarin dose; date of next test; and proposed duration of treatment. Include this information in the Discharge Summary. Liverpool Stroke Unit Warfarin Management guidelines adapted from the Alfred Hospital Melbourne, Yarrawonga Health Service and Armidale Health Service, WA by the” Safer Systems Saving Lives” project. Warfarin management in acute stroke patients. February 2006 Page 3 of 10 The ‘Warfarin Therapy Chart’ should be given to the patient and a copy to the patient’s GP, and the discharge checklist on the back of this chart should be completed and signed. The ‘Discharge Instructions’ should be completed by a medical officer and given to the patient. The ‘Patient Education and Discharge Management’ should be completed and counselling provided by the clinical pharmacist or appropriate Registered Nurse. A ‘Warfarin Alert Card’ and ‘Important Information for Patients’ should be given to the patient. TABLE 4 SUGGESTED TREATMENT TIMETABLE Timeline Management Plan Pre Treatment Commencing Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 Day 7 Post First Week Full Blood Count (FBC) International Normalised Ratio (INR) Activated Partial Thromboplastin Time (APTT) Biochemistry Liver Function Test Oral Warfarin as Per Age Adjusted Nomogram S/C Enoxaparin (Clexane) 1mg/kg bd Oral Warfarin as Per Age Adjusted Nomogram S/C Enoxaparin (Clexane) 1mg/kg bd Full Blood Count (FBC) International Normalised Ratio (INR) Oral Warfarin as Per Nomogram S/C Enoxaparin (Clexane) 1mg/kg bd Full Blood Count (FBC) - If Indicated International Normalised Ratio (INR) Oral Warfarin as Per Nomogram S/C Enoxaparin (Clexane) 1mg/kg bd Full Blood Count (FBC) - If Indicated International Normalised Ratio (INR) - If Indicated Oral Warfarin as Per Nomogram S/C Enoxaparin (Clexane) 1mg/kg bd Full Blood Count (FBC) - Note Platelets International Normalised Ratio (INR) - If Indicated Cease S/C Enoxaparin (Clexane) 1mg/kg bd if INR is Therapeutic for the Previous 48 Hours (INR Range 2-3) If INR Not Therapeutic Range Administer S/C Enoxaparin (Clexane) 1.5mg/kg Full Blood Count (FBC) - If Indicated International Normalised Ratio (INR) Cease S/C Enoxaparin (Clexane) 1mg/kg bd if INR is Therapeutic for the Previous 48 Hours (INR Range 2-3) Continue Warfarinisation for at Least 3 Months Check International Normalised Ratio (INR) Weekly as Appropriate GP / MO May Wish to Discuss Future Management and Duration of Treatment with a Specialist Physician 6. RENAL IMPAIRMENT The following dosage adjustments are recommended for the treatment dosage ranges. This dosing applies to patients with a creatinine clearance of less than 30mL/min. Drug Normal Dosing Enoxaparin Enoxaparin 1 mg/kg Twice Daily 1.5 mg/kg Once Daily Severe Renal Impairment Creatinine Clearance Less Than 30mL/min 1 mg/kg Once Daily 1 mg/kg Once Daily Although no dosage adjustment is recommended in patients with moderate (creatinine clearance 30-50mL/min) and mild (creatinine clearance 50-80mL/min) renal impairment, careful clinical monitoring of potential bleeding complications is advised. Liverpool Stroke Unit Warfarin Management guidelines adapted from the Alfred Hospital Melbourne, Yarrawonga Health Service and Armidale Health Service, WA by the” Safer Systems Saving Lives” project. Warfarin management in acute stroke patients. February 2006 Page 4 of 10 COMPILED BY Safer Systems Saving Lives Collaboration. Liverpool Hospital. Warfarin in acute stroke patients program (WASPP) working party. April 2006 Pharmacy Department in consultation with the Medical Services and the Pharmacy Advisory Committee. Armadale Health Service. With reference and acknowledgements to: The Western Hospital Anti-coagulation and Thromboembolism Prophylaxis (Guidelines for), 1999. North Western Health, Prescriber Guidelines for Initiation of Full Anti-coagulation, 1999. The Alfred, Guidelines on the Use of Anticoagulants. 1998. Adapted from Wimmera Warfarin Therapy Chart in: Wimmera Clinical Risk Management - A Systematic Approach To Reducing Medical Errors. Wimmera Health Care Group, 2001. Liverpool Stroke Unit Warfarin Management guidelines adapted from the Alfred Hospital Melbourne, Yarrawonga Health Service and Armidale Health Service, WA by the” Safer Systems Saving Lives” project. Warfarin management in acute stroke patients. February 2006 Page 5 of 10 LIVERPOOL HOSPITAL HEALTH SERVICE PATIENT EDUCATION & DISCHARGE MANAGEMENT Date: …………………………………….. PATIENT IDENTIFICATION UNIT RECORD NO: …………………………………………………….……………. SURNAME: ……………………………………………………………………………. GIVEN NAMES:………………………………………………………….……………. DATE of BIRTH: ………….../………....../…………... Sex ……….…………….. (Or Affix Patient Label) Education to begin at commencement of Warfarin Therapy including ongoing completion of the booklet patient. Only check patient’s knowledge twice if patient answered ‘no’ to any question in first session. OBJECTIVES OF EDUCATION : Prior to Discharge the Patient Will be Able to: 1. Indicate that He/She has a Warfarin Education Booklet/ information sheet Yes 2. State that He/She has Read the Booklet/information sheet Yes 3. Demonstrate that the Documentation of the Dose and INR in the Warfarin Yes Booklet/information sheet is up to Date 4. Explain the Action of Warfarin Anticoagulant drug, used to prevent or treat thrombosis by decreasing the clotting power of the Yes blood. 5. Answer the Following Questions Regarding Warfarin Are you aware there are two brands of Warfarin? (Yes) Yes State the brand that you are on (Marevan / Coumadin). Yes Are the two brands the same? (No) Yes Can you swap between brands? (No) Yes 6. State: (a) Why He/She is Taking Warfarin (b) The Length of Time Required to Take Warfarin To prevent clot formation around the prosthetic or bioprosthetic valve. Yes To prevent the recurrence of deep vein thrombosis (DVT). Yes To prevent clot formation in heart (Atrial Fibrillation). Yes Length of time (see “planned duration” on Page 3). Yes 7. Identify the 3 manufactured doses of Warfarin brand he/she is taking: Coumadin 1 mg - Light Tan; 2 mg - Lavender; 5 mg - Green Yes 8. State: (a) When to take Warfarin With the evening meal every day - use a calendar. Yes (b) Why it is Important to Take the Drug at the Same Time Every Day To maintain consistency for checking of INR. Yes 9. Outline the Steps to Take if They Forget to Take their Dose of Warfarin at 6.00pm If patient remembers within two to three hours they can take Warfarin. Yes If longer don’t take Warfarin, take next dose when it is due and tell your doctor or laboratory. Yes 10. Outline When Blood Tests are Required at Home Every 2nd day until INR is stabilised, then as directed by the GP or Pathology Service. Yes 11. Identify Significant Signs of Bleeding Obvious bleeding ie. cuts, nosebleed, bleeding gums. Yes Less obvious bleeding – urine, faeces, vomit and coughing. Yes 12. State What He/She Will do in the Event of Signs of Bleeding Call the GP promptly. Yes 13. Identify other Medications that May Interfere with the Way that Warfarin Works Prescription medications and over the counter medications eg. aspirin, paracetamol or other pain Yes medications, rubs, liniments, cold or cough preparations. Antacids, laxatives, multi-vitamins (may contain Vitamin K). Yes Herbal medications. Yes 14. Identify Illnesses that Require Reporting to Their GP Diarrhoea, vomiting. Yes Infection or fever. Yes Pain, swelling or discomfort. Yes 15. Understand Significant Dietary Facts Maintain a well balanced and consistent diet – Avoid crash dieting and binge eating. Yes Stabilise intake of Vitamin K. This includes green leafy vegetables. Yes If taking vitamin or herbal supplements discuss with GP or pharmacist. Yes Take alcohol in moderation. Yes 16. Understands the Discharge Instructions Sheet Completed by the Doctor Yes 17. Patient has had Warfarin Education with Pharmacist/RN Yes Pharmacist's Signature: Date: Staff Members Signature: Designation: SEND COMPLETED FORM TO PHARMACY by the No No No No No No No No No No No No No No No No No No No No No No No No No No No No No No No No No Issued: July 2004 Page 6 of 10 LIVERPOOL HOSPITAL HEALTH SERVICE PATIENT IDENTIFICATION UNIT RECORD NO: WARFARIN THERAPY CHART SURNAME: Name of GP: ……………………………………………………. Date: ………./………./………. …………………………………………………….………… ………………………………………………………………………… GIVEN NAMES: ………………………………………………………….………… DATE of BIRTH: ………….../…………...../…………... Faxed: ………./………./……….. Faxed By: ………………. Sex ……….………… (Or Affix Patient Label) INDICATION: Atrial Fibrillation Deep Vein Thrombosis Pulmonary Embolism Prosthetic Valve Other: …………………………………………………………………………………………………………………………… PRESCRIBER'S SIGNATURE: SURNAME (Print): SUGGESTED THERAPEUTIC INR RANGES (TARGET INR) Low Risk Mechanical Prosthetic Heart Valves High Risk Mechanical Prosthetic Heart Valves All other indications Date This data should be Commenced included in the Discharge Summary and the Warfarin Booklet Target INR 2.0 to 3.0 2.5 to 3.5 2.0 to 3.0 Planned Usual Maintenance Duration Dose INSTRUCTIONS FOR USE: 1. This WARFARIN THERAPY CHART must be used for EVERY patient on oral Anticoagulant Therapy. 2. The doctor should write in the Regular Medications section of the Medication Chart “SEE WARFARIN THERAPY CHART” or should apply the Warfarin sticker provided. If this is not done, then a nurse or pharmacist should do it. 3. YDHS ‘Guidelines for Anti-Coagulation Using Warfarin’ should be used when prescribing warfarin, which are available on all wards. 4. If patient's Marevan is unavailable, only Coumadin is kept at YDHS, so use Patient's own. TREATMENT ORDERS / TELEPHONE ORDERS / RECORD OF TREATMENT INR WARFARIN (Coumadin) Dosage Time to be Given mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 WARFARIN mg 1800 Date Time Initial Doctor's Signature MR/168 WARFARIN Administered Nurse's Signature NEXT INR DUE AM ON: ……………………………………………………………………….. (Day and Date) COPY TO BE GIVEN TO PATIENT ON DISCHARGE D:\106741972.doc WARFARIN THERAPY CHART Date Page 7 of 10 DISCHARGE CHECKLIST The following checklist must be completed and signed prior to the patient being discharged from Yarrawonga District Health Service. The relevant documentation is available in the 'Medication Procedures Manual' or in the 'Clinical Procedures Manual'. Sign When Completed 1. The ‘Discharge Instructions’ should be completed and given to the patient. 2. The ‘Patient Education and Discharge Management’ should be completed, with counselling provided or organised with the clinical pharmacist or Nurse. 3. The ‘Warfarin: Important Information for Patients’ and a blue ‘Warfarin: Important Instructions for Patients’ book should be given to the patient. 4. A ‘Warfarin Alert Card’ should be produced and given to the patient. WARFARIN ALERT CARD SAMPLE A personalised plastic ‘Warfarin Alert Card’ should be organised for the patient through the ward pharmacist prior to discharge. If the patient is being discharged over the weekend, the card can be sent to them. The following is a sample of what the card will look like: WARFARIN PATIENT DETAILS Name: …………………………………….. IMPORTANT PATIENT INFORMATION Immediately consult doctor if increased bruising, blood stained vomit/urine, dark bowel actions, nose bleed, headache/dizziness, joint/muscle /stomach / back pain, leg weakness/numbness. Always attend for regular blood tests (INR). Ensure your doctor orders more frequent INRs & adjusts warfarin dose when new medications are started / stopped, regular medication doses are changed or with reduced oral intake, illness and vomiting. Indication: ………………………………… Recommended INR: …………………….. Expected Duration of Treatment: ……………………………. Doctor: …………………………………… Please Show This Card When Presenting to Hospital &/or Emergency Department, Doctor, Pharmacist or Dentist If this Card is Found Please Return to Liverpool Hospital Health Service Pharmacy Department (02) 98283000 Page 8 of 10 WARFARIN: IMPORTANT INFORMATION FOR PATIENTS WARFARIN ALERT CARD Please present this Card when attending for treatment or seeking advice from your doctor, dentist, pharmacist, physiotherapist, occupational therapist or any other health practitioner. INR BLOOD TESTS After leaving hospital, your next INR test is due on: …………………………………… This test can be performed by your local doctor, pathology laboratory. You must contact your Doctor when you have your INR results to find out what your Warfarin dose should be. WARFARIN Warfarin belongs to a class of drugs known as anticoagulants, or ‘blood thinners’. It helps to prevent the blood from clotting in your blood vessels (ie. arteries and veins). There are TWO different brands of Warfarin, they are Marevan and Coumadin. (Yarrawonga District Health Service only prescribes the Coumadin brand.) Always use the same brand of Warfarin: do not swap Coumadin tablets for Marevan. WARFARIN DOSE Warfarin is prescribed in milligrams. There are THREE different strengths of Coumadin: 1mg Tablets: Light Tan Colour 2mg Tablets: Lavender Colour 5mg Tablets: Green Colour Ensure you take the correct tablets by checking the colour and strength against the dose prescribed by your doctor. ADMINISTRATION TIME Take the exact number of tablets prescribed under your doctor’s direction at the same time each day. If you forget your regular daily dose, you may take that dose within 2-3 hours of missing that dose. If 2-3 hours has already passed, please consult your doctor. Do not take an extra dose on the next day. LABORATORY TESTS The safety and effectiveness of Warfarin must be monitored regularly by performing INR blood tests. Your doctor will order these to ensure the correct amount of Warfarin is prescribed. The INR blood level should be measured every 1 to 2 days if: Starting warfarin for the first time. Starting warfarin again, after having stopped it for a surgical procedure or other reason. Starting on new medicines or herbal preparations that are prescribed by your doctor or bought over-the-counter (without a prescription). Stopping any prescribed or over-the-counter medicines or herbal preparations. You are eating less for any reason (eg. with illness, vomiting, fasting for religious reasons). Consult your doctor & request an INR test if any of the above situations arise. Page 9 of 10 After your INR test: 1. 2. Phone your doctor (or the laboratory where the test is performed) on the day your INR test is taken, and ask what, if any, dose adjustment is required. Write down the INR result and any dosage changes in your record book. Once the INR result is stable, your INR may be monitored less frequently (usually once every two to four weeks, depending upon your particular situation). OTHER MEDICATIONS Other medications may change the blood-thinning effect of warfarin. This includes medicines that are prescribed by your doctor or bought over-the-counter without a prescription (eg. Aspirin, cold and cough mixtures, laxatives, antacids, herbal, and vitamin preparations). If you take warfarin, please tell your doctor all the medicines and other remedies you are taking. Please ensure you read the section on Laboratory tests and the need for regular INR test if you start, stop, or change medications. DIETARY PRINCIPLES Avoid crash dieting and binge eating. Use alcohol in moderation - avoid binge drinking. If taking laxatives or antacids, use in moderation and discuss this with your doctor. Green leafy vegetables may be eaten in moderation (these contain Vitamin K, which opposes the action of Warfarin). SURGICAL PROCEDURES Your Warfarin may need to be stopped well before your surgery, dental work or medical procedure (eg. Gastroscopy, colonoscopy, arthroscopy, emergency room treatment after injury). At your first appointment please tell the doctor/dentist performing your procedure that you are taking warfarin. TRAVEL Please ensure that your doctor provides you with a letter, and arranges for an INR test and follow up with another doctor during your period of travel. PREGNANCY Warfarin should not be taken if you are pregnant, or are considering becoming pregnant. If you become pregnant, you must report to your doctor immediately. Please discuss an alternative type of anticoagulant therapy with your doctor. SIGNS OF BLEEDING Warfarin acts as a blood thinner and therefore it increases the risk of bruising and bleeding. Please attend your doctor or a hospital emergency department immediately if you experience: Less Obvious Signs: Red or dark urine or bowel actions. Blood-stained vomit. Joint, muscle, stomach or back pain. Leg weakness or numbness. Headache, visual disturbance or dizziness. Page 10 of 10 Obvious Bleeding: Bruising: ANY OTHER UNUSUAL FEATURES. Any bleeding that does not stop by itself (eg prolonged bleeding from cuts). Nosebleeds. Bleeding of gums from brushing. Increased menstrual flow, vaginal bleeding. Increased or new appearance of black or blue bruise marks. Acknowledgement to the Yarrawonga District Health Service Pharmacy Department, the Alfred Hospital in Melbourne, and Armadale Hospital. Page 11 of 10