Nevoid Basal Cell Carcinoma Syndrome
advertisement

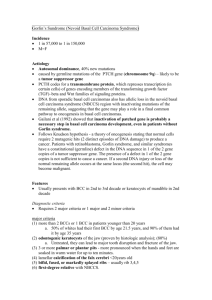
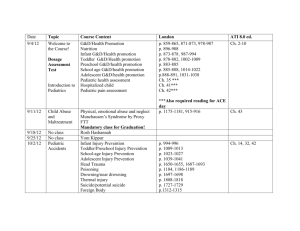
Nevoid Basal Cell Carcinoma Syndrome Author: Daniel Berg, MD, FRCP(C), Professor of Dermatology, Director of Dermatologic Surgery, University of Washington School of Medicine Contributor Information and Disclosures Updated: Mar 12, 2009 Introduction Background The autosomal dominant nevoid basal cell carcinoma syndrome (NBCCS) represents a series of multiorgan abnormalities known to be the consequence of abnormalities in the PTCH gene. The syndrome has been documented for 50 years, but more recent developments in molecular genetics have dramatically increased understanding of its pathophysiology (see Causes). Pathophysiology Multiple organ systems may be impacted in nevoid basal cell carcinoma syndrome (NBCCS). Abnormalities of the skin, the skeletal system, the genitourinary system, and the CNS are the most common. A variety of less common neoplasms are also associated. Frequency International The approximate prevalence is reported to be 1 case per 56,000-164,000 population. The prevalence is likely to be considerably higher in individuals younger than 20 years who present with basal cell carcinomas (BCCs). Mortality/Morbidity Morbidity and premature mortality are primarily related to the development of skin cancers and other tumors associated with the syndrome. Actual mortality rates are unavailable; morbidity from multiple skin cancers and their treatment may be severe. Race The syndrome is found in all races. However, a definite but smaller percentage of African Americans present with skin cancer and have fewer skin cancers than whites who are affected. This decreased number of skin cancers, a diagnostic hallmark, may account for the comparatively fewer African Americans ascertained in reviews of the syndrome. Full expression of the non – skin cancer features of the syndrome is found in African Americans. Sex Men and women are affected equally. The male-to-female ratio is estimated to be 1:1.3. Age The disease is present (inherited) at birth and most commonly manifests itself with either BCCs (usually multiple) occurring at a young age (third decade or earlier) or odontogenic keratocysts presenting in the second or third decade. Other incidental findings, such as cleft lip, or asymptomatic findings, such as hypertelorism, may be noticed earlier, but these features may not lead to the diagnosis until the development of more specific findings. Findings usually seen in the syndrome, such as jaw cysts, BCCs, calcification of the falx, and ovarian fibromas, develop more commonly with increasing age in the individual who is affected. Some findings are present earlier in childhood. Medulloblastoma, though a relatively less common manifestation of NBCCS, is a tumor of early childhood. Radiologic abnormalities, such as bifid ribs, or asymptomatic findings, such as palmar pits, may be present at a higher frequency in childhood; these findings may be helpful in making an early diagnosis. 1 Clinical History Many of the features of nevoid basal cell carcinoma syndrome (NBCCS) present as signs rather than symptoms. Symptoms are most likely related to the major findings. Cutaneous symptoms: Local invasion of an aggressive BCC may lead to pain or symptoms (eg, neurologic) related to local invasion. Metastasis is extremely rare. Neurologic symptoms: Medulloblastoma, a cerebellar tumor of young childhood, may present with neurologic symptoms in a child who is affected. Genitourinary symptoms: Ovarian fibromas are usually asymptomatic, but they may present with pain secondary to torsion. Dental symptoms: Odontogenic keratocysts (also called keratocystic odontogenic tumors) may be asymptomatic, or they may manifest as jaw pain or abnormal dentition. Physical Despite the recent understanding of the underlying genetic basis of nevoid basal cell carcinoma syndrome (NBCCS), the diagnosis remains clinical. Kimonis et al have suggested the following diagnostic criteria to help the clinician. Although not absolute, these criteria help guide the clinician in choosing laboratory evaluation for both diagnostic purposes and ongoing surveillance. Clinicians must remember that some of the findings listed may present at different ages; therefore, ongoing surveillance with respect to diagnosis may be needed. Diagnosis of NBCCS is made in the presence of 2 major criteria or 1 major and 2 minor criteria. The major criteria consist of the following: (1) more than 2 BCCs or 1 BCC in patients younger than 20 years; (2) odontogenic keratocysts of the jaw (proven by histologic analysis); (3) 3 or more palmar or plantar pits; (4) bilamellar calcification of the falx cerebri; (5) bifid, fused, or markedly splayed ribs; and (6) first-degree relative with NBCCS. The minor criteria include the following: (1) macrocephaly; (2) congenital malformations, such as cleft lip or palate, frontal bossing, coarse facies, and moderate or severe hypertelorism; (3) other skeletal abnormalities, such as Sprengel deformity, marked pectus deformity, and marked syndactyly of the digits; (4) radiologic abnormalities, such as bridging of the sella turcica, vertebral anomalies, modeling defects of the hands and feet, or flame-shaped lucencies of the hands and the feet; and (5) ovarian fibroma or medulloblastoma. Several studies have documented the incidence of the various features found in the syndrome.2,3,4,5,6 Characteristic facies occur due to increased calvarial size. Other contributing features include a broadened nasal root, frontal and biparietal bossing, mild hypertelorism, and an exaggerated length of the mandible. Ocular findings include congenital blindness due to corneal opacity and cataract or glaucoma, occurring in as many as 10-15% of patients. Strabismus (exotropia) may be seen. Cleft lip or palate occurs in 3-5% of patients. BCCs are the most common finding in the syndrome. Of whites older than 40 years, 97% had BCCs. Tumors are usually multiple. BCCs are most common on the face, the neck, and the upper part of the trunk, that is, in sun-exposed areas, but they are also increased in relatively sun-protected areas. Although some lesions may become aggressive, most are not. Tumors largely begin to appear between puberty and age 35 years, but they may appear at a younger age. In 1997, Kimonis et al found that 50% of whites had their first BCC by age 21.5 years and 90% had it by age 35 years.6 Lesions may present as any kind of clinical or histologic BCC; however, some lesions may be small and resemble milia, small nevi, tags, or hemangiomas. Milia may be seen in as many as 30% of patients with NBCCS. Multiple basal cell carcinomas on the back of a patient with nevoid basal cell carcinoma syndrome. Multiple small papules on the neck and upper trunk in a 10-year-old patient. Biopsy confirmed basal cell carcinoma. Asymmetric palmar and/or plantar pits are seen in 65-87% of all people with NBCCS. When they do develop, they often do so early in life, being found in as many as 80% of patients younger than 10 years. Thus, they may be a helpful early criterion for the diagnosis of NBCCS. More than 3 pits should be noted because the relevance of 1 or 2 pits may not be diagnostic. Odontogenic keratocysts are seen in 74-80% of patients. They usually begin to develop in the first decade (after age 7 y), with the peak incidence in the second and third decades, which is younger than seen with isolated odontogenic cysts. They are more common in the mandible than in the maxilla. They are usually asymptomatic, but they may cause pathologic fracture, swelling, loose teeth, or displacement of developing permanent teeth. Medulloblastoma (malignant tumors of the cerebellum) occur in 1-4% of patients. They present in childhood, with the greatest risk from birth to 3 years, although cases have been reported as late as 7 years. Skeletal abnormalities include polydactyly of the hands or the feet, hallux valgus, pectus excavatum or pectus carinatum, and syndactyly of the second and third fingers. Kyphoscoliosis may also be more common or more severe in NBCCS. Sprengel deformity of the shoulder occurs in 5-10% of patients. A short fourth metacarpal may be seen with increased frequency, although as many as 10% of healthy persons also have this sign. Genitourinary system findings include bilateral calcified ovarian fibromas, which are found in 14-24% of women; these are often asymptomatic and rarely become malignant. Men may have associated cryptorchidism or gynecomastia and reduced body hair, although these findings have not been confirmed by recent studies. Cardiac findings are less common, but an increased risk of cardiac fibroma may be present. Cardiac fibroma usually presents in children or young adults. Other tumors, including fibrosarcoma, rhabdomyosarcoma, and meningioma, may be increased in frequency in persons with NBCCS. Causes Nevoid basal cell carcinoma syndrome (NBCCS), also known as basal cell nevus syndrome (BCNS), is an autosomal dominant syndrome caused by mutations in the PTCH (patched) gene found on chromosome arm 9q. The disease has complete penetrance and variable expressivity. Although clinical features vary more among families than within families, no clear-cut link exists between specific mutations and phenotype. Approximately one third of cases are new mutations. Genetics of NBCCS7,8,9,10,11 o First elucidated in fruit flies, the protein product of the patched gene is important in determining segment polarity of wings and limbs (anterior-posterior relationships in developing embryos). In mammals, the patched gene (PTCH) is an important inhibitor in the so-called hedgehog (HH) signaling pathway, whose downstream proteins can lead to cell growth. PTCH is frequently mutated on 1 allele in sporadic BCCs, and, according to Epstein, "upregulation of HH signaling is the pivotal abnormality in all BCCs."12 . o Its wide-reaching activity accounts for the myriad of findings in patients with NBCCS. o Ultraviolet (UV) light exposure appears to be an important cofactor. BCCs are much more common in sun-exposed areas and are much more common in whites with the syndrome. Nevertheless, molecular genetic studies looking for o UV-related mutations in BCCs obtained from patients with NBCCS leave the possibility that agents other than UV-B may cause alterations to the gene.13 Patients are particularly sensitive to ionizing radiation (XRT), and reports of multiple BCCs in the radiation portal developing in patients treated with XRT for medulloblastoma exist. Reports of more aggressive BCCs occurring in sites of previous XRT for BCC also exist. Radiobiologic studies on fibroblasts suggest an abnormal response to radiation in fibroblasts obtained from patients with NBCCS. Differential Diagnoses Fibrous Papule of the Face Milia Nevi, Melanocytic Seborrheic Keratosis Other Problems to Be Considered Bazex syndrome (X-linked dominant syndrome with BCCs, follicular atrophoderma, hypertrichosis, and hypohidrosis of the face and the head) Pseudohypoparathyroidism Rombo syndrome Unilateral nevoid BCC with comedones Workup Laboratory Studies No routine laboratory studies are helpful for nevoid basal cell carcinoma syndrome (NBCCS). Molecular genetic testing: Although the diagnosis is usually made in adults or older children based on clinical findings, molecular testing is available to confirm the diagnosis in patients with atypical findings or possibly for prenatal diagnosis. Molecular testing may be useful for infants of an affected patient who is too young too have developed diagnostic clinical findings. Because of imperfect sensitivity and specificity, genetic testing should be performed in conjunction with a genetic counselor. Availability and methodology of testing may change with time; this is another reason genetic counseling is recommended. Current and updated information on available genetic testing is available through GeneTests. Imaging Studies Radiography14 o Skull radiography: Calcification of the falx cerebri is the most common radiologic finding, occurring in 65-92% of individuals and seen on anteroposterior skull radiographs. This finding is age-related; in one study, this finding was observed in 37% of patients younger than 20 years and in 77-79% of patients older than 20 years. This finding may also be seen in approximately 5% of unaffected individuals. Calcification of the tentorium cerebelli is observed in 20-40% of patients. This is more typically seen on lateral skull radiographs. Calcification of the petroclinoid ligament, pia, and choroid plexus may also be observed. Calcification of the diaphragma sellae may be observed in 60-80% of patients with NBCCS, compared with 4% of the healthy population. Recent studies have suggested both a lower prevalence in people affected and a higher prevalence in unaffected relatives, making this finding less specific. o Skeletal radiography: Bifid, hypoplastic, fused, partially missing, or splayed ribs are observed in 38-60% of patients. These features may be a helpful diagnostic criterion because it is present in children before other features may show up and because it is uncommon in the general population. Most commonly affected ribs are the 3rd, 4th and 5th though others may be involved. It is important that the radiologist specifically look for these features in order not to overlook them. Malformations at the occipitovertebral junction and cervical or upper thoracic vertebral fusion may also be observed. Calcification of the nuchal ligament occurred in one study in 18% of affected people. Small, pseudocystic, lytic bone lesions known as "flame-shaped lucencies" are found on radiographs of the hands (30%) and feet (17%) of affected people. o Dental panoramic radiography: This screening is useful for the finding of odontogenic keratocysts, which are relatively common in NBCCS. When monitoring a child with NBCCS, consider regular dental visits plus panoramic radiography to detect odontogenic keratocysts. Cardiac echocardiography: This study may be used to look for cardiac fibroma (relatively rare). In patients with NBCCS, one might consider a baseline test at birth and subsequently if clinical suspicion arises for cardiac fibroma. MRI of the head: MRI may be more sensitive than plain radiography for calcification, and it may be indicated if medulloblastoma is suspected in a child with NBCCS. Because of the concern about exposure to radiation in patients with the syndrome, MRI is the preferred imaging modality over CT scanning. Consider an annual MRI up to age 7 years. Pelvic ultrasonography: Consider performing ultrasonography around puberty as a baseline and, then, if symptoms are present, to look for ovarian fibromas. Other Tests Physical examination for the cutaneous and extracutaneous features of NBCCS may be helpful in finding criteria to make the diagnosis in uncertain cases. Procedures Biopsy of skin lesions: The histologic features of the individual skin cancers are indistinguishable from ordinary BCC and include the full spectrum of histologic subtypes. Biopsy of jaw cysts: Odontogenic keratocysts have a characteristic pathologic finding that shows the lining with keratinizing epithelium. Treatment Surgical Care Treatment of patients with nevoid basal cell carcinoma syndrome (NBCCS) involves surveillance for and treatment of the associated findings. Because most of the findings involve tumors (benign and malignant), treatment is often surgical. Oral surgery involving cyst enucleation followed by mechanical curettage or use of peripheral ostectomy may be required for odontogenic keratocysts. The incidence of recurrence following treatment is high. For BCCs, early detection and treatment are critical to prevent any individual lesion from becoming invasive. Avoidance of radiation is an important principle based on several reports of BCCs developing in radiated fields. Surgical methods include electrodesiccation and curettage (ED&C), simple excision, Mohs micrographic surgery, and photodynamic therapy. o ED&C is an excellent treatment for BCCs in this syndrome, especially small or primary lesions. In addition to being relatively simple, this modality avoids the covering-up of possible residual tumor with skin grafts or flaps. Patients who have had multiple ED&Cs rather than multiple complex closures are more likely to keep reconstructive options intact should they require more significant excisions in the future. Superficially destructive modalities such as carbon dioxide laser have been reported but few data exist to support routine use. o Surgical excision may often be performed in an outpatient setting. The main disadvantage in patients with NBCCS is the creation of full-thickness skin defects that may need complex repairs, skin grafts, or skin flaps for closure. Because of the expectation that patients with NBCCS will develop many tumors, assessing whether a new lesion is primary or recurrent in the face of previous excisions can be difficult. o Mohs micrographic surgery should be saved for larger, recurrent, or more aggressive tumors or those in critical locations where simpler modalities, especially ED&C, are less likely to lead to a cure. o Photodynamic therapy for BCC involves the delivery of a phototoxic drug (topically or systemically) followed by light treatment. Topical aminolevulinic acid (ALA-PDT) and methyl-aminolevulinic acid (MAL-PDT) have been used with various light sources to treat BCC.15,16 The main potential advantage is the ability to treat multiple small lesions in one sitting. It is not as effective for recurrent or larger tumors. Photodynamic therapy is currently approved by the US Food and Drug Administration for treatment of actinic keratosis in the United States. Surgery for ovarian tumors or cardiac tumors may be required for either treatment or prevention of symptoms. Consultations A dermatologist should maintain ongoing surveillance and treatment of skin cancer. Frequent visits (every 2-3 mo) are recommended to identify and to treat lesions when they are as small as possible. A genetic counselor is a critical component of the ongoing care of the patient, particularly with issues of having children. As new research is performed, the availability, sensitivity, and specificity of molecular testing may change. Other specialists may be needed to help manage associated abnormalities if they develop; specialists may include a neurologist and/or a neurosurgeon, a pediatrician, a cardiologist and/or a cardiac surgeon, a gynecologist, a dentist and/or an oral surgeon, a plastic surgeon, and an ophthalmologist. Medication Topical agents such as imiquimod17 and 5-fluorouracil are available and have been approved for treatment of BCC in the United States. These medications have a lower cure rate than surgical therapy but may be a useful adjunct in patients with multiple lesions. Despite the lower cure rate (which may reach up to 80% for superficial BCCs with imiquimod), they may play a useful role in allowing patients to treat their own selected smaller lesions, especially superficial BCCs on the trunk and extremities. In general, they should be considered best for use in smaller or more superficial lesions, away from critical anatomic sites. Investigations and clinical trials are being undertaken into the use of novel agents such as tazarotene (Tazorac) and a newly developed HH inhibitor.12 Although potentially promising, approval by the US Food and Drug Association and availability await further testing and results. Antineoplastic Agent, Antimetabolite 5-Fluorouracil, topical (Carac, Efudex) Cycle-specific agent that has activity as single agent and, for many years, has been combined with biochemical modulator leucovorin. Shown to be effective in adjuvant setting. Classic antimetabolite anticancer drug with chemical structure similar to endogenous intermediates or building blocks of DNA or RNA synthesis. Inhibits tumor cell growth through at least 3 different mechanisms that ultimately disrupt DNA synthesis or cellular viability. These effects depend on intracellular conversion of 5-FU into 5FdUMP, 5-FUTP, and 5-FdUTP. 5-FdUMP inhibits thymidylate synthase (key enzyme in DNA synthesis). 5-FUTP is incorporated into RNA and interferes with RNA processing. 5-FdUTP is incorporated into DNA, leading to cytotoxic DNA strandbreaks. Used topically for management of superficial BCC. Dosing Apply bid, in sufficient amount to cover lesions, for a minimum of 3 wk; only 5% strength is recommended; therapy might be required for up to 10-12 wk Pediatric Administer as in adults Interactions Adult None reported Contraindications Documented hypersensitivity; potentially serious infections Precautions Pregnancy X - Contraindicated; benefit does not outweigh risk Precautions Inflammatory reactions may occur with use of occlusive dressings; porous gauze dressing may be applied for cosmetic reasons without increase in reaction; patients should expect inflammatory reaction with crusting Topical Skin Product Imiquimod (Aldara) Immune response modifier thought to produce a nonspecific anti-AK response (interferon, natural killer cells) and a specific immune response (cytotoxic T cells). Indicated to treat clinically typical, nonhyperkeratotic, nonhypertrophic AKs on the face or scalp. Precise mechanism for superficial BCC is unknown. May increase tumor infiltration of lymphocytes, dendritic cells, and macrophages. Indicated for biopsy-confirmed, primary superficial BCC in adults with normal immune systems. Additionally, tumors must not be >2 cm in diameter on certain areas of the body. Only indicated when surgical methods are not appropriate. Dosing Apply cream to treatment area (including 1 cm of skin surrounding tumor) 5 nights/wk at bedtime for 6 wk; leave on for 8 h, then wash area Pediatric Not established Interactions None reported Contraindications Documented hypersensitivity Precautions Adult Pregnancy C - Fetal risk revealed in studies in animals but not established or not studied in humans; may use if benefits outweigh risk to fetus Precautions Medical follow-up is essential to ensure cancer has responded adequately to treatment; may cause redness, swelling, and sore development at application site; may cause itching or burning Avoid exposure to sunlight or artificial tanning devices; regular use of sunscreen is encouraged; avoid contact with lips, eyes, or nostrils; common adverse effects include erythema, edema, vesicles, erosion or ulceration, weeping, exudate, flaking, scaling, dryness, scabbing, or crusting Follow-up Further Outpatient Care Ongoing surveillance and treatment for sequelae of nevoid basal cell carcinoma syndrome (NBCCS) is required. In addition, in family members of patients with NBCCS in whom the diagnosis is possible but not confirmed, ongoing follow-up to help detect diagnostic criteria may be important. BCCs require frequent follow-up care, 3-4 times a year (or more), to achieve early diagnosis and treatment. In young children at risk, medulloblastomas necessitate a neurologic examination every 6 months, and intermittent MRIs should be considered in children younger than 7 years. Odontogenic keratocysts require dental follow-up visits, including periodic radiographic evaluation, especially in childhood and early adolescence. Ovarian fibromas should be followed-up with regular pelvic examinations, with pelvic ultrasonography as required to help detect ovarian fibromas. Cardiac fibromas have an incidence as high as 3% in some studies. A baseline echocardiography should be considered with the diagnosis. Deterrence/Prevention Patients should be aware of the possible deleterious effect of XRT in NBCCS. Patients should be aware of the hereditary nature of the disease, and they should have genetic counseling. Patients should be aware of the need for limiting exposure to UV light. Patient Education Patients with nevoid basal cell carcinoma syndrome (NBCCS) need information about the syndrome. Coping with the multiple BCCs and the required multiple treatments is often difficult, and patient counseling and support may be critical. Web sites exist with resources for patients with BCNS (see BCCNS Life Support Network). In regard to skin cancer, patients should be advised to reduce UV light exposure. Patients should also be advised about the relative risk of receiving XRT for their skin cancers. With respect to other findings, patients should be counseled to look for symptoms referable to the CNS, the genitourinary system, the cardiovascular system, and dentition, as well as other potentially involved systems. For excellent patient education resources, visit eMedicine's Cancer and Tumors Center. Also, see eMedicine's patient education articles Skin Cancer and Skin Biopsy.