Drugs 41 (Suppl. 3): 69-79, 1991
0012-6667/91 /0300-0069/$5.50/0
© Adis International Limited All
rights reserved.
DRSUP2 139a
The Efficacy of Diuretics in Acute and Chronic
Renal Failure Focus on Torasemide
T. Risler, B. Kramer and G.A. Milller
Section of Nephrology and Hypertension, Department of Medicine II I.
University of Tubingen. Tubingen, Federal Republic of Germany
Summary
Loop diuretics in high doses are the drugs of choice in the treatment of both acute
renal failure (ARF) and chronic renal failure (CRF). Their pharmacokinetic and pharmacodynamic properties give them a high efficacy, even in severely compromised renal
function. The serum elimination half-life and duration of action of most loop diuretics
are dependent on the glomerular filtration rate and are therefore prolonged in renal failure. Torasemide, a new high ceiling and long acting loop diuretic, is as potent as furosemide (frusemide) in patients with advanced renal failure. Unlike other loop diuretics
the half-life and duration of action of torasemide are not dependent on renal function
and the parent drug does not accumulate in renal failure. The extent of metabolism is
clinically negligible. A number of studies have demonstrated the efficacy of furosemide
bumetanide, piretanide and torasemide in patients with ARF and CRF. When compared
with the other loop diuretics, torasemide has the following advantages: a longer half-life
independent of renal function, no indications of toxic side effects and apparently less
influence on calciuresis.
Acute renal failure (ARF) is characterised by a
rapid deterioration of renal function, resulting in
progressive azotaemia. Although oliguria (urine
output < 400 ml/24h) is a common feature of ARF,
there have been some exceptions (nonoliguric or
polyline ARF) [Maharaj 1988].
Chronic renal failure (CRF) is a syndrome which
results from progressive and irreversible destruction of the nephron, regardless of the underlying
cause. It is defined by a reduced glomerular filtration rate (GFR) for > 3 to 6 months. The interindividual variety in the severity of the signs and
symptoms of uraemia may be great, depending on
the magnitude of renal failure.
Diuretics are of special importance in the treat-
ment of both ARF and CRF. Traditionally high
dose loop diuretics, mannitol, or both are used
either to prevent oliguric ARF or to convert it into
nonoliguric rena failure. which is easier to manage
clinically (Levine 1989). However, there are few
controlled studies to support this practice and it is still
uncertain whether diuretics can alter the course of
oliguric ARF.
In CRF loop diuretics in high doses are valu-able
in the management of associated fluid roten-tion and
hypertension.
For the treatment of ARF and CRF an ideal
diuretic should:
• increase renal volume and sodium excretion, in
70
a dose-dependent manner, even when the GFR is
as low as 5 ml/min:
• leave calcium and potassium excretion undisturbed;
• be excreted and metabolised independently of
renal function;
• have no toxic side effects even in high doses;
• not be eliminated via haemodialysis.
Torasemide is a new high ceiling loop diuretic
which, compared with furosemide (frusemide), has
a longer elimination half-life, a long duration of
action and a nearly complete bioavailability [Delarge 1988; Lesne 1988; Neugebauer et al. 1988].
The properties of torasemide will be compared with
other available loop diuretics according to the principles listed above. The role of loop diuretics in
general, their indications, pharmacokinetic and
pharmacodynamic properties and their clinical use
will be reviewed in this paper.
1. Available Diuretics for the Treatment
of Renal Failure
Renal physiologists have elucidated the mode of
action of almost all diuretics in animal models
(Greger & Schlatter 1983; Oberleithner et al. 1982).
According to their mode of action, diuretic substances can be divided into different groups, not
all of which are appropriate for use in renal failure.
The osmotic diuretics interfere with the capacity of the proximal tubule, the ascending limb of
the loop of Henle, and the collecting ducts to reabsorb water. Osmotically active but nonreabsorba-ble
sugars such as mannitol bind water and thus
impede its reabsorption. These substances are primarily used to treat ARF. Hanley and Davidson
(1981), among others, demonstrated a protective
effect of mannitol on the development of ARF in
their animal model. However, this preventive effect has not yet been confirmed in clinical medicine despite many studies.
Beall et al. (1965) attributed the beneficial effect
of mannitol more to the increase in diuresis than
glomerular filtration. This proposal alone justifies
a trial with osmotic diuretics in order to transform
an oliguric into a polyuric renal failure.
Drugs 41 (Suppl.3) 1991
The dosage should be restricted to prevent a
large amount of psmotically active material being
left in the circulation in case of therapeutic failure
Mannitol is very difficult to remove, even with
dialysis.
Osmotic diuretics have only a few and somewhat debatable indications in CRF (Rodrigo et al.
1977). Mannitol may be used to prevet hypotension and muscle cramps in patients on haemodialysis who present with a massive fluid overload
Dialysis dysequilibrium syndrome may be alleviated by mannitol in severely uraemic patients.
Drugs inhibiting the proxinnal tubular carboanhydrase reduce sodium bicarbonate reabsorption
and enhance water and salt excretion. Metabolic
acidosis, often accompanying renal failure, reduces
the availability of bicarbonate and thus inhibits this
class of diuretic. Therefore, carboanhydrase inhibitors are ineffective in renal failure.
Thiazides and analogous substances increase
diuresis by inhibiting sodium reabsorption in the
distal tubule. These drugs are of minor importance
in the treatment of patients with renal failure as
their effectiveness diminishes when the GFR is <
30 ml/min. Nevertheless, they may have clinical
importance by enhancing the effect of loop diuret
ics in terminal renal failure when given concomicantly. Loop diuretics improve the distal delivery
of sodium and thus allow thiazides to act more ef
fectively (Wollam et al. 1982).
Some related substances, such as xipamide, have
properties that place them between thiazides and
loop diuretics (Krömer & Rister 1988). They are
effective even in severe renal failure.
Potassium-retaining diuretics reduce potassium
excretion dependent on and independent of aldosterone in the distal part of the distal convoluted
tubule and the proximal collecting ducts.
This group of less effective diuretics is often
combined with thiazides for patients with hypertension or cardiac failure. Their potassium-retaining properties may increase dramatically in renal
failure and thus generate dangerous hyperkalaemia. Therefore, these substances have no place in
the therapy of patients with ARF and CRF.
Loop diuretics reduce sodium choride reab-
Efficacy of Diuretics in Acute and Chronic Renal Failure
sorption mainly in the thick ascending limb of
Henle's loop, but also in the proximal tubule (as a
consequence of parallel increases in osmolar clearance and bicarbonate excretion). This group of diaretics is mainly indicated in renal failure, because
of the marked effect in reduced renal function.
Thus, only loop diuretics meet the basic requirements for use in ARF and CRF.
1.1 Loop Diuretics in Acute Renal Failure
Animal experiments have demonstrated conflicting results on the effect of the loop diuretic
furosemide in the prevention of ARF (Baehler et
al. 1977, De Torrente et al. 1978; Fink 1982). In
are majority of these studies, loop diuretics increased urine production but did not improve renal
function. Furosemide appears to protect the thick
Escending limb of the loop of Henle by decreasing
oxygen-consuming transport processes (Brezis et al.
1984), which may improve tolerance to hypoxia.
Potential advantages of loop diuretics in ARF as
summarised by tiller and Mudge (1980) include
Dilution of toxins in the tubular lumen, increase of
intratubular pressure with consequent removal of
obstructions, enhanced potassium excretion and
liberal water and electrolyte intake.
The few controlled clinical studies on the treatment of oliguric ARF (Brown et al. 1981: Cantarovich et al. 1973; Epstein et al. 1975; Kleinknecht
et al. 1976; Minuth et al. 1976) demonstrate that
loop diuretics increase diuresis without improving
renal function and prognosis, but greatly facilitate
patient care. Use of very high doses has been associated with irreversible deafness in some patients
(Brown et al. 1981).
1.2 Loop Diuretics in Chronic Renal Failure
The choice of diuretics for use in ARF and CRF
is restricted to loop diuretics, thiazide analogues
with similar properties, and osmotic diuretics. All
others lose their effect in severely impaired renal
fuction. Thus, the following discussion on
pharmacology and clinical use will focus on these
drugs and their indications.
71
Loop diuretics are the drugs of choice in patients
with CRF. While a shortcut intense diuresis is obtained in patients with normal renal function, the
diuretic effect is reduced and prolonged by the
shrinking number of nephrons in renal failure.
Fractional excretion of salt and water decreases with
declining renal function. The effectiveness of loop
diuretics is correlated with the total amount of filtered salt and water. All loop diuretics act from the
luminal side of the tubule. Therefore, glomerular
filtration. and free tubular secretion of these drugs
is a prerequisite for their diuretic effect. Many different substances and drugs compete for the tubular
secretory system for weak organic acids. Thus,
endogenous acids as well as drugs may impede tubular secretion of loop diuretics in renal failure.
Brater et al. (1986) calculated a dose-response
curve for intravenous furosemide and demonstrated that a dose of > 160mg did not produce
enhanced diuretic activity. These results call into
question the prescribing of very high doses of loop
diuretics in patients with a GFR of < 5 ml/min.
The relationship between dose, effect and toxic side
effects will be discussed later.
As well as their tubular action, loop diuretics
may also enhance renal plasma flow (Higashio et
al. 1978). Some investigators (Fritz et al. 1971) have
used high doses to improve the GFR. These authors consider that a direct effect on glomerular filtration is likely, but others disagree with those results (Allison & Kennedy 1971). An increase in the
GFR as a consequence of increased renal plasma
flow may have been misinterpreted as an independent phenomenon.
In this paper, established loop diuretics (mainly
furosemide, but also bumetanide and piretanide)
will be compared with torasemide, a new member
of the class.
2. Pharmacokinetics and
Pharmacodynamics of Loop Diuretics in
Renal Failure
The pharmacokinetic properties of loop diuretics are of primary importance in renal failure, because they reach their site of action via glamerular
filtration and mainly tubular secretion.
72
Drug 41 (Suppl.3) 1991
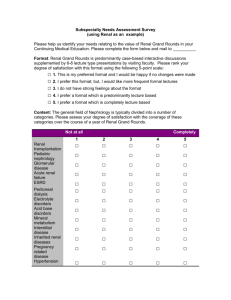
Fig. 1. Correlation of the amount of drug excreted into the urine (dotted lines) and sodium excretion (bars) for (a) torasemide
and (b) furosemide (frusemide) after single intravenous administration. Time 0 denotes administration of the drugs.Urine
was collected during 0 to 6, 6 to 12, 12 to 24 hours on a preceding control day, the day after administration of the drug,
and on the second day thereafter. * = significant differences from the respective collection period of the preceding contra
day (adapted from Klutsch et al. 1988: Kult et al. 1990, with permission).
Efficacy of Diuretics in Acute and Chronic Renal Failure
73
The bioavailability of furosemide is 40 to 65%
will wide intersubject variability in normal volunteers (Beerrnann & Groschinsky-Grind 1980; Benet
1979). The bioavailability of bumetanide is calculated between 65 and > 90% (Holazo et al. 1984;
lau et al. 1986; Marcantonio et al 1983) without
major differences in renal failure. According to
Marone et al. (1984), the bioavailability of piretanide is about 80%. For torasemide, bioavailability between 80 and 90% was demonstrated (Lesne
1988; Neugebauer et al. 1988).
The discrepancies between the findings from
studies of the bioavailability of various loop diuretics probably result from the different methods
used to determine drug concentrations, and different dosages. Some authors suggest an influence of
renal failure on bioavailability (Marcantonio et al.
1983; Tilstone & Fine 1978). Nevertheless, interindividual differences are substantial. Thus, individual factors more than renal failure may account
for the intraindividual variability in bioavailability
and salidiuretic response. The serum protein binding of diuretic drugs is a crucial consideration, since
only the free fraction of the drug undergoes glomerular filtration. All loop diuretics are avidly
bound to serum albumin (Goto et al. 1980); thus,
the main renal excretion mechanism of these drugs
is tubular secretion. In renal failure, the protein-bound
fraction decreases (Goto et al. 1980), which could
facilitate access to the site of action inside the
tubule. However, this effect is unlikely to become
clinically significant, since, for loop diuretics
eliminated mainly by the kidney, the terminal halflife is increased with the loss of renal function. The
terminal half-life of furosemide has been reported
to increase 3 times in functionally anephric patients
(Keller et al. 1981). However, Cutler et al. (1974)
demonstrated a less than doubled elimination halflife in an identical group of patients. Huang et al.
(1974) calculated an even longer terminal half-life
that was 10 times that of healthy controls. Similar
findings were reported by Walter et al. (1985) for
piretanide. The half-life increased up to 3-fold in
patients with end-stage renal failure. Bumetanide
is equalfy affected by a loss of renal function (Lau
et al. 1986; Marcantonio et al. 1983). Torasemide,
however, is an exception; the diuretic efficacy of
this new loop diuretic has been shown to be comparable to furosemide in single-dose studies in
patients with advanced renal failure using oral doses
of torasemide 100, 200 and 400mg compared with
furosemide 250 and 500mg and when torasemide
100 and 200mg and furosemide 100 and 200mg
have been administered intravenously to patients
with CRF (Grabensee et al. 1986; Klütsch et al.
1988). A long acting salidiuretic effect was demonstrated for torasemide.
After intravenous administration, the ratio of
equipotency of torasemide and furosemide was
1: 1, in contrast to studies with volunteers or
patients with acute heart failure where the ratio was
found to be 1: 2 on a weight basis (Lesne 1988;
Stroobandt et al. 1982). As demonstrated by Dodion and Willems (1986), the elimination half-life
of torasemide (3 to 4 hours) is independent of renal
function. A study by Knauf et al. (1990) on the
pharmacodynamic effect and pharmacokinetics of
torasemide (20mg, single intravenous dose) in
healthy controls and patients with stable CRF of
varying degrees found the half-life of torasemide
(3.4 to 4.1 hours) to be independent of renal function. This was due to the fact that nonrenal clearance of torasemide was 3 times higher than its renal
clearance.
In a controlled clinical trial, comparing the
pharmacodynamics and pharmacokinetics of torasemide and furosemide in patients with highgrade renal failure after single intravenous doses of
either torasemide 100 and 200mg or furosemide
100 and 200mg, all 4 drug preparations induced a
significant increase in fractional as well as cumulative urine volume, sodium and chloride excretion during 24 hours. Sodium excretion was directly correlated with the renal excretion of
torasemide and furosemide (fig. 1). This has been
noted as a general feature of loop diuretics (Brater
et al. 1986, 1987; Knauf et al. 1990). In patients
with renal failure, the half-life of torasemide in
serum and urine was unchanged compared with
healthy subjects, whereas it was prolonged in the
case of furosemide (table I). As expected, renal
clearance of both drugs was reduced in patients with
renal failure, whereas total clearance of torasemide
Efficacy of Diuretics in Acute and Chronic Renal Failure
75
prostaglandin levels in patients with ARF and that
the increase was more pronounced in responders
to loop diuretics than in nonresponders. By this
mechanism, loop diuretics may counteract the
vasoconstriction due to hyperactivity of the reninangiotensin-aldosterone system in renal failure.
In conclusion, effective loop diuretic action
seems to be dependent on a system which responds
with an increase in vasodilatory prostaglandins. It
could therefore be speculated that the effect of loop
diuretics on intrarenal prostaglandins might contribute to their natriuretic effect.
be expected to exert any clinically relevant diuretic
effects.
3. Clinical Efficacy of Loop Diuretics
3.1 Acute Renal Failure
As previously discussed, there is no evidence in
humans that loop diuretics prevent ARF. The outcome and prognosis of oliguric ARF are not influenced, but loop diuretics may improve the management of these patients by increasing salt and
water excretion. Furosemide (Brown et al. 1981;
Cantarovich et al. 1973; Kleinknecht et al. 1976)
and torasemide (Andreucci et al. 1990) were administered to patients with oliguric ARF. In these
studies, high doses reversed oliguria into polyuria
in most patients. Toxicity was dose related and
appeared to be of concern at gram-doses of furosemide. Side effects were not observed in patients
on torasemide.
There is. increasing evidence for an important
role of renal prostaglandins in various aspects of
renal function. It has been shown, for example, that
renal prostaglandin E excretion increases after
intravenous administration of furosemide and torasemide (Dupont et al. 1988; Mackay et al. 1984).
Kirsten et al. (1990) investigated the influence of
piretanide (single intravenous dose) on vasoactive
3.2 Chronic Renal Failure
The efficacy of loop diuretics in CRF has been
investigated in a number of controlled or comparative studies. The saluretic effect of torasemide was
compared with furosemide in double-blind, controlled studies. Mourad et al. (1988) treated 46
patients with a GFR of < 30ml per minute.
Torasemide 20mg had a short-lived natriuretic effect, while torasemide l00mg and furosemide 60mg
significantly increased 24-hour sodium excretion.
Torasemide l00mg was more effective than furosemide 60mg and had a longer duration of action.
Calcium excretion was significantly increased only
in the furosemide group (table II).
In a single dose multicentre study, intravenous
torasemide 100 and 200mg was compared with the
same doses of intravenous furosemide in 90 patients
prostagiandins, (catecholarnines,) renin and aldosterone in patients with ARF. It was shown that
loop diuretics in high doses increased
vasodilatory
Table II. Effect of torasemide 20mg and 100mg, furosemide (frusemide) 60mg and placebo after single intravenous (IV) doses on 24hour volume, sodium, potassium, chloride and calcium excretion in patients with chronic renal failure. Data are presented as a
mean percentage increase over the preceding control day (adapted from Mourad et al. 1988)
Change from control value (%)
no. of patients
volume
sodium
Torasemide 20mg IV
11
NS
Torasemide 100mg IV
10
+26
Furosemide 60mg IV
13
+32
Placebo
12
NS
NS
Abbreviation: NS = no significant change.
+34
potassium
chloride
calcium
NS
+52
NS
+78
NS
+127
NS
+55
NS
+72
+40
NS
NS
NS
76
(creatinine clearance < 30 ml/24 hours) [Klusch et
al. 1988; Risler et al. 1986]. Urine volume, and
renal sodium, calcium and chloride excretion increased with both drugs. Potassium excretion was
altered less by torasemide. A dose increase enhanced the diuretic effect of both drugs. However,
the increase in fractional excretion was greater with
torasemide than with furosemide when the dose
was doubled, indicating a steeper dose-response relationship for torasemide compared with furosemide in this dose range (fig. 2).
19 patients (creatinine clearance of 9 to 12ml
per minute) who had previously been receiving furosemide 500mg daily for 2 weeks, took part in a
study which compared the effects of torasemide
100 and 200mg with those of furosemide 250mg,
for 14 days (Kult et al. 1988). Compared with baseline on furosemide 500mg. water and sodium excretion remained almost unchanged in the torasemide 100mg group (volume: -7%. sodium: +12%)
and decreased in the furosemide 150mg group (volume: -11%, sodium: —15%), but increased significantly in the patients on torasemide 200mg (volume: +20%, sodium: +47%). Another clinical trial
compared high dose torasemide (200 mg/day orally)
with furosemide (500 mg/day orally) in 10 patients
with advanced CRF (Clasen et al. 1988). After 14
days the doses were doubled for a further 2 weeks
of treatment Although torasemide was administered in a 2.5 times lower dose, the effect of both
drugs on oedema and fluid and sodium excretion
was equipotent. Calcium excretion was significantly more pronounced in patients receiving furosemide and plasma reran activity also increased
in these patients but not in the torasemide--treated
group. No adverse effects and, notably no impairment of cochlear function, were observed in either
group, indicating that high dose torasemide is safe
and effective in the treatment of advanced CRF.
Russo et al. (1990) investigated the efficacy
of torasemide (200 mg/day) in 11 patients with
hypertension and CRF. Torasemide significantly
lowered blood pressure and reduced peripheral
oedema in all patients without adverse effects
(fig. 3).
Drugs 41 (Suppl. 3) 1991
3.2.1 Haemodialysis
Loop diuretics have also been used to treat
patients on haemodialysis. Patients with a residual
diuresis of 200 to 500ml benefit from diuretic
therapy; their urinary output increases, and their
fluid intake may be increased accordingly. The advantages of this treatment are gains in patient comfort and quality of life. Schulz et al. (1990) have
compared the effect of torasemide 200mg with furosemide 500mg and placebo in 80 patients over a
3-month treatment period.
This randomised
double-blihd trial demonstrated an increased urinary output of water, sodium and chloride in both
actively treated groups compared with placebo.
After 3 months, neurological examination dem-
Fig. 2. Median increases in 24-hour fractional excretion (FE),
∆ FE (obtained as median differences of FE in the therapy
period, minus the preceding control period over 24 hours
each) for volume, sodium and chloride after single intravenous doses of torasemide 100 and 200mg and furosemide 100
and 200mg (from Kult et al. 1990, .with permission).
* = p 0.05 when comparing the 200mg to the l00mg dose.
Efficacy of Diuretics in Acute and Chronic Renal Failure
77
Fig. 3. Reduction in blood pressure (bars) and bodyweight (line) in hypertensive patients with chronic renal failure during
9 days' treatment with intravenous torasemide (0.77 mg/kg bodyweight; from Russo et al. 1990, with permission).
* .= p < 0.0025; ** = p < 0.0005.
onstrated 2 detericration of polyneuropathy (unrelated to treatment in 4 furosemide patients. I
on placebo and none on torasemide.
Similar results were demonstrated by Schmidt
et al. (1981) in a short term study comparing furosemide 240mg with the same dose of muzolimine. In a second study, the efficacy of different
doses of torasemide and furosemide in 44 patients
on haemodialysis were investigated (Stolear et al.
1990). Compared with pretreatment placebo control, torasemide in doses of 100 to 200mg decreased interdialytic weight gain and increased urine
volume and sodium excretion simultaneously.
Haemodialysis and haemofiltration do not alter
the pharmacokinetics of torasemide; as might be
expected from its high degree of protein binding,
it has been shown that no significant elimination
of torasemide by dialysis occurs (Loute et al. 1986).
The administration of very high doses of these
drugs in severs renal failure and on dialysis has
provided a considerable amount of intermation on
their toxicity. Furasumide is ototoxic in high doses.
and toxicity is increased by aminoglycosides, Bumetanide may provoke muscular discomfort in
patients treated with more than 12mg per day. To
date, there have been no reports of severe side effects of torasemide or piretanide.
4. Conclusion
Torasemide is a high ceiling diuretic which, in
comparison with furosemide, has a longer elimination half-life independent of renal function. Torasemide increased fractional excretion of volume
and sodium dose-dependently up to 200mg orally
or intravenously in patients with CRF. Calcium
78
Drugs 41 (Suppl. 3) 1991
excretion appeared to be less than with furosemide.
Torasemide was shown to be as effective as furosemide in the diuretic management of patients with
advanced renal failure, promoting diuresis and
preventing weight gain without affecting the neurological status. Decreased GFR leads to retention
and prolongation of the half-life of furosemide,
which may account for an increase in therapeutic
potency compared with torasemide. In patients with
normal renal function, the ratio of equipotency is
1 : 2 (torasemide vs furosemide) and l : l in patients
with severe renal failure after intravenous administration. After oral administration, available data
suggest an equipotency ratio of l : 2.5 (torasemide
vs furosemide), whereas this ratio is approximately
1 : 4 in healthy volunteers and patients with normal renal function. The differences depending on
route of administration reflect the almost complete
bioavailability of torasemide compared with a bioavailability of approximately 50% for furosemide.
In a study of Kampf and Baethke (1980), bumetanide 6mg was less effective than furosemide
250mg in patients with a serum creatinine level between 3 and 7 mg/dl. In another group of patients
(serum creatinine between 7 and 14 mg/dl) bumetanide 12mg had a smaller diuretic effect than
furosemide 500mg.
In healthy humans, there is a ratio of 1: 40 between responses to equal doses of bumetanide and
furosemide. In renal failure this difference diminishes to 1 : 11 (Kampf & Baethke 1930), with the
maximal effect apparent - not at 1 to 1.5 hours but at 6 hours.
In conclusion, torasemide is a new high ceiling
loop diuretic which differs from other loop diuretics with respect to its almost complete bioavailability,
its longer half-life and duration of action being
independent of renal function, and its lack of
severe side effects.
References
Allison MEM, Kennedy AC. Diuretics in chronic renal disease: a study
of high dosage furosemide. Clinical Seience 41: 171-187, 1971
Andreasen. F. Hansen HE, Mikkelsen E. Phlarmacokinetics of
furosemide in anephric patients and in normal subjects. European
Journal of Clinical Pharmacology 13: 41-48. 1978
Andreucci NE. Russa D, Memoli B, Testa A. Rampino T, et al. Efficacy
of IV torasemide in the treatment of acute and chronic high grade
renal failure. In Kruck et al. (Eds) Torasemide: Clinical Pharmacology
and Therapeutic Applications, Progress, in Pharmacology and Clinical
Pharmacology Vol. 8/1, pp. 229-238, Gustav Fischer Verlag, Stuttgart, 1990
Baehler RW, Kotchen TA, Burke JA, Galla JH, Bhathena D. Consid
erations on the pathophysiology of mercuric chloride-induced renal
failure. Journal of Laboratory and Clinical Medicine 90: 330-340, 1971
Beall AC, Hall WC, Morris GC, DeBakey ME. Mannitol-induced os
motic diuresis during renal artery occlusion. Annals of Surgery
161:46-52, 1965 .
Beermann B, Groschinsky-Grind M. Clinical pharmacokinetics of di
uretics. Clinical Pharmacokinetics 5: 221-245, 1980
Benet LZ. Pharmacokihetics/pharmacodynarnics of furosemide in man:
a review. Journal of Pharmacokinetics and Biopharmaceutics 7: 127, 1979
Brater DC, Anderson SA, Brown-Cartwright D. Response to furosemide
in chronic renal insufficiency: rationale for limited doses. Clinical
Pharmacology and Therapy 40. 134-139, 1986
Brater DC, Leinfelder J, Anderson SA. Clinical pharmacology of torasemide, a new loop diuretic. Clinical Pharmacology and Therapeutics
42: 187-192, 1987
Brezis M, Rosen S, Silva P, Epstein FH. Transport activity modifies
thick ascending limb in the isolated perfused kidney. Kidney International 25: 65-72, 1984
Brown CB, Ogg CS, Cameron JS. High dose of furosemide in acute renal
failure: a controlled trial. Clinical Nephrology 15: 90-96, 1981
Cantarovich F, Galli C, Benedetti L, Chena C, Castro L, et al. Highdose furosemide in established acute renal failure. British Medical
Journal 4: 449-450, 1973
Clasen W, Khartabil T, Imm S, Kindler J. Torasemide for diuretic treatment of advanced chronic renal failure. Arzheimittel-Forschung 38:
209-211, 1988
Cutler RE, Forrey AW, Christopher TG, Kimpel BM. Pharmacokinetics
of furosemide in normal subjects and functionally anephric patients.
Clinical Pharmacology and Therapeutics 15: 588-596, 1974
Delarge J. Chemistry and pharmacological properties of the pyridine-2sulfonylurea derivative torasemide. Arzneimittel-Forschung 38: 144150, 1988
De Torrente A, Miller PD, Cronin RE, Pauisin PE, Erickson AL, et al
Effects of furosemide and acetylcholine in norepinephrine-induced
renal failure. American Journal of Physiology 235: F131-F136, 1978
Dodion L, Willems JL. Study of the elimination kinetics of torasemide.
a novel loop diuretic, in renal insufficiency. European Journal of
Clinical Pharmacology 31 (Suppl.): 49-51, 1986
Dupont AG, Gerlo E, Van der Niepen P, Piepsz A. Renal pharmacodynamic effects of torasemide and furosemide in normal man Arzneimittet-Forschung 38: 172 175, 1988
Epstein M, Schneider NS, Befeler B. Effect of intrarenal furosemide on
renal function and intrarenal hemodynamics in acute renal failure.
American Journal of Medicine 58: 510-516, 1975
Fink M. Are diuretics useful in the treatment of prevention of acute renal
failure? Southern Medical Journal 75: 329-334, 1982
Flamenbaun W, Friedman R. Pharmacology, therapeutic efficacy, are
adverse effects of bumetanide, a new 'loop' diureutic. Pharmacother
apy 2: 213-222, 1982
Fritz K.W, Wilbrandt R, Piehl W, Freyland MD, Freund HW. Longterm high dosage furosemide in chronic renal insufficiency. Postgraduate Medicine 47: 4244, 1971
Goto S, Yoshitomi H, Miyamoto A, [none K, Nakano M. Binding of
several loop diuretics to serum albumin and human serum from
patients with renal failure and liver disease. Journal of Pharmacodynamics 3: 667-676, 1980
Grabensee B, Knabe P, Koczy B, Hecring P, Achhammer J, et al. Witkungsvergleich unterschiedlicher oraler Dosen von Torasemid and
Furosemid bei chronischer Niercninsuffizienz. Nieren and Hochdruckkrankheiten 15: 374, 1986
Greger R, Schlatler E. Cellular mechanism of the action of loop
diuretic on Ihe thick ascending limb of Henle's loop. Klinische Wochenschrifl 61: 1019-1027, 1983
Efficacy of Diuretics in Acute and Chronic Renal Failure
Hanley MJ, Davidson K. Prior mannitol and furosemide infusion in a
model of ischemie acute renal failure. American Journal of Physiology 241: F556-F564. 1981
Higashio T. Abe Y, Yamamote K. Renal effects of bumetanide. Journal
of Pharmacology and Experimental Therapeutics 207: 212-220. 1978
Holazo AA, Colburn WA. Gustafson JH, Young RL. Parsonnet M. Pharmacokinetics of bumetanide following intravenous, intramuscular, and
oral administrations to normal objects. Journal of Pharmaceutical
Sciences 73: 1108-1113, 1984
Huang CM, Atkinson A. Levin N, Quintanilla A. Pharmacokinetics of
furosemide in advanced renal failure. Clinical Pharmacology and
Therapeutics 16: 659-666, 1974
Kampf D, Baethke R. Die diuretische Effektivitat von Bumetanid im
kontrollierten Vergleich zu Furosemid bei chronischer Niereninsuffizienz unterschiedlichen Schveregrades. Arzneimittel-Forschung 30:
1015-1018, 1980
Keller E, Hoppe-Seyler G, Mumm R, Schollmeyer P. Influence of hepatic cirrhosis and end-stage renal disease on pharmacokinctics and
pharmacodynamics of furosemide. European Journal of Clinical
Pharmacology 20: 27-33, 1981
Kirsten R, Rictbrock I, Huber ED. Heintz B. Nelson K, et al. Influence
of piretanide on vasoactive prostaglandins, catecholamines, renin and
aldosicrone in patients with acute renal failure. In Puschctt & Greenberg (Eds) Diuretics III: chemistry, pharmacology and clinical applications. Elscvicr Scicnt Publishing Company. New York. 1990
Kleinknecht D, Ganeval D, Gonzalez-Duque LA, Fermanian J.
Furosemide in acute oligutic renal failure: a controlled trial.
Nephron 17: 51-58, 1976
Klutsch K., Grosswendt J, Haecker W. Single dose comparison of
torasemide and furosemide in patients with advanced renal-failure,
Arzneimittel-Forschung 38: 200-204, 1988
Knauf H, Spahn H, Rucker II-M, Mutschler E. The loop diuretic
torasemide in renal failure. Kinetics and dynamics. In Kruck
et. al. (Eds) Torasemide: Clinical Pharmacology and Therapeutic Applications. Progress in Pharmacology and Clinical
pharmacology vol. 84 no.81,93. Gustav Fisher Verlag, Stutigart.
1990
Kramer BK. Risier T Xipamide- Cardiovascular Drug Review, 6:
141-154, 1988
Kult J, Hacker W, Glocke M. Comparison of efficacy and tolerance of different oral doses of torasemide and furosemide in
patients with advanced chronic renal failure. Arzneimittel-Forschung 38: 212-214. 1988
Kult J, Ziegler J, von Mollendorf E. Pharmacodynamics and
pharmacokinetics of torasemide and furosemide in patients with
high grade renal failure after application of high intravenous
doses. In Kruck et al. (Eds) Torasemide: Clinical Pharmacology and Therapeutic Applications. Progress in Pharmacology
and Clinical Pharmacology Vol. 8/1, pp. 239-248, Gustav
Fischer Verlag, Stuttgart, 1990
Lau HSH, Heyneck ML, Berardi RR, Swartz RD, Smith DE. Kinetics, dynamics, and bioavailability of bumetanide in healthy
subjects and patients with chronic renal failure. Clinical
Pharmacology and Therapeutics 39: 635-645, 1986
Lesne M. Comparison of the pharmacokinetics and pharmacodynamics of torasemide and furosemide in healthy volunteers.
Arzneimittel-Forschung 38: 160-163, 1988
Levine SD. Diuretics. Medical Clinics of North America 73: 271282, 1989
Loute G, Adam A, Ers P, Heremans C, Willems B. The influence
of haemodialysis and haemofiltration on the clearance of torasemide in renal failure. European Journal of Clinical
Pharmacology 31 (Suppl.): 53-55, 1986
Mackay IG, Muir AL, Watson ML. Contribution of prostaglandins to the systemic and renal vascular response to furosemide
in normal man. British Journal of Clinical Pharmacology 17:
513-519, 1984
Maharaj B. Diuretics in retinal failure. Progress in Pharmacology
6: 267-288, 1988
Marcantonio LA, Auld WKR, Murdoch WR, Purohit R, Skellern
GG, et al. The pharmacokinetics and pharmacodynamics of
79
the diuretic bumetanide in hepatic and renal disease. British
Journal of Clinical Pharmacology 15: 245-252. 1983
Marone C. Reuhi FC. Perisic M. Lahn W. Pharmacokinctics of
high closes of piretanidc in moderate to severe renal failure.
European Journal of Clinical Pharmacology 27: 589-593. 1984
Minuth AN, Terrell JB, Suki WN. Acute renal failure: a study of
the course and prognosis of 104 patients and of the role of
furosemide. American Journal of Medical Sciences 271: 317324, 1976
Mourad G. Haecker W, Mion C. Dose-dependent salidiuretic efficacy of torasemide in comparison to furosemide and placebo in
advanced renal failure. Arzneimittel-Forschung 38: 205-208. 1988
Neugebauer G. Besenfelder E, von Mollendorff E pharmacokinetics and metabolism of torasemide in man ArzneimittelForschung 38:164-166: 1988
Oberleithner H. Giebisch G, Lang F. Wang W. Cellular mechanism of the furosemide sensitive transport system in the kidney. Klinische Wochenzeitschrift 60: 1173-1179. 1982
Pentikaainen PJ. Pasternack A. Lampainen E. Neuvonen PJ.
Penttila A. Bumetanide kinetics in renal failure. Clinical
Pharmacology and Therapeutics 37: 582-588. 1985
Rane A. Villeneuve JP, Stone WJ, Nies AS. Wilkinson GR, et al.
Plasma binding and disposition cf furosemide in the nephrotic
syndrome and in uremia. Clinical Pharmacology and Therapeutics 24: 199-207, 1978
Risler T. Hellstern R, Ress K. Achhammer A, Hacker W. et al.
Torasemid bei chronischer Niereninsuffizienz. Nieren- und
Hochdruckkrankheiten 15: 527-528. 1986
Rodrigo F. Shideman J. McHugh R. Buselmeier T. Kjellstrand
C. National history, clinical correlations and influence of dialysate glucose and intravenous mannitol. Annals of Internal
Medicine 86: 554-561, 1977
Russo D. Gazzotti MR, Testa A. Torasemide a new loop diuretic
in patients with chronic renal failure. Nephron 55: l41 -1 4 5 .
1990
Schmidt P. Loew D, Dycka J. Kopsa H. Baleke P. et al. Compurison of the effects of neurochronic and furosemide in
patients with and-stage renal failure and chronic dialysis.
European, Journal of Chinical Pharmacology 20: 23-26,1981
Schulz. W, Dorfler A. Stiehl L. Achhammer I. Double blind
chinical trial investigating the efficacy and long-term
tolerance of torasemide 200mg p.o. compared with furosemide
500mg p.O. and placebo p.o. in patients with chronic renal
failure on hemodialysis - a multicenter study. In Kruck et al. (Eds)
Tora-semide Clinical Pharmacology and Therapeutic Applications.
Progress in Pharmacology and Clinical Pharmacology, Vol. 8/
1, pp. 249-257. Gustav Fischer Verlag, Stuttgart. 1990
Stolear IC, Achhammer I, Georges B. Efficacy of torasemide in
the treatment of patients with high-grade renal failure on dialysis. Progress in Pharmacology and Clinical Pharmacology
Vol. 8/l, pp. 259-267. Gustav Fischer Verlag, Stuttgart. 1990
Stroobandt R. Dodion L, Kaesteloot H..Clinical efficacy of torasemide, a new direutic agent, in patients with acute heart
failure: a double blind comparison with furosemide Archives of
International Pharmacodynamics 260: 151-15S. 1982
Tiller DJ, Mudgc GH. Pharmacologic agents used in the management of acute renal failure. Kidney International 18: 7007 l l , 1980
Tilstone WJ. Fine A. Furosemide kinetics in renal failure. Clinical
Pharmacology and Therapeutics 23: 644-650. 1978
Walter U, Rockel A, Lahn W, Heidland A. Heptner W. Pharmacokinctics of the loop diuretic piretanide in renal failure.
European Journal of Clinical Pharmacology 29: 357-343. l985
Wollam GL. Tarazi RC, Bravo EL. Dustan HP. Diuretic potency
of combined hydrochlorothiazide and furosemide therapy in
patients with azotemia. American Journal of Medicine 72: 929938, 1982
Correspondence and reprints: Dr Teut Risler, Section of Nephrology and Hypertension, Department of Medicine III, University
of Tubingen, Otfried-Muller-Strasse 10, 74 Tubingen, Federal Republic of Germany.