Protocol for management of acute life
advertisement

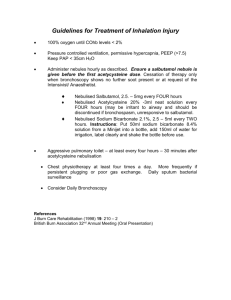
October 2004-09-21 Protocol for management of acute life-threatening asthma on PICU The following signs are established features of Life-threatening Asthma: Disturbance in conscious level (decreased conscious level or agitation) Silent Chest Exhaustion Poor Respiratory Effort Cyanosis in air (i.e. SaO2 < 85% in air) PEFR < 33% expected or best (BTA Guidelines, Thorax 1997)1 General Management Administer Oxygen Oxygen delivery should be adequate to maintain SaO2 above 94% Provide a calm and reassuring environment. Allow child to assume most comfortable position. Often sitting upright reduces distress and improves chest wall movement. NO routine CXR the decision to intubate, is made on clinical grounds Antibiotics are not routinely given. There is NO place for long acting beta2agonists in severe acute asthma Most asthmatics are dehydrated due to poor intake of fluids and increased insensible losses. Hence fluids should be given but care should be taken to maintain euvolaemic state as hyperhydration may lead to problems with pulmonary oedema and SIADH. Monitoring ECG monitoring Close serum electrolyte and blood glucose monitoring. Watch carefully for hypokalaemia. BP monitoring Oxygen saturation monitoring Note PEFR monitoring will not be tolerated by these patients. October 2004-09-21 Asthma therapy Beta2agonists Nebulised Salbutamol Dose 2.5 mg under 5yrs 5mg above 5 yrs IV Salbutamol bolus 5 micrograms per kilogram over 5 minutes IV Salbutamol infusion 1 to 5 micrograms per kilogram per minute Notes Can be repeated as required. Can give continuous nebulisation (up to between 40 and 80mg per hour) Maximum concentration 200 micrograms per ml. Dilute if needed in 0.9% Saline or 5% Dextrose. Recommended concentration 10 micrograms per ml. (If problems with excessive volume, maximum concentration 200 micrograms per ml). Dilute if needed in 0.9% Saline or 5% Dextrose. Nebulised therapy Administer salbutamol either nebulised or intravenously. Salbutamol via MDI is inappropriate in these hypoxic patients Nebulisation must be driven via oxygen between 6 and 10 l/min O2. In severe asthma, continuous nebulisation has been shown to be advantageous over intermittent nebulisation3. Intravenous Salbutamol Intravenous Salbutamol should be used in patients who are unresponsive to nebulised therapy or in patients who have decreased tidal volume with near complete airway obstruction. After an initial loading dose of 5micrograms/kg over 5 minutes, a continuous infusion of 1 to 5micrograms/kg/min should be set up 1. Monitor blood electrolytes and glucose carefully. Be especially vigilant for hypokalaemia. October 2004-09-21 Anticholinergics Nebulised ipratropium bromide Initial management Nebulised ipratropium bromide Subsequent management Dose Give 3 doses of 250 micrograms every 20 minutes 250 micrograms every 6 hours 500 micrograms every 6 hours Notes Ipatropium can be combined with salbutamol for nebulisation if 5 years age or younger if above 5 years age Current evidence suggests that Ipatropium Bromide significantly improves lung function in acute severe asthma5,6. Ipratropium Bromide should be nebulised concurrently with salbutamol. In severe or life-threatening episodes of asthma the greatest benefit is achieved by giving three doses of 250micrograms of nebulised Ipratropium Bromide in the first hour of management (i.e. every 20 minutes)5,6 After the first hour, nebulised Ipratropium should be prescribed 6-hourly (250micrograms if below 5 years and 500micrograms if above 5years). Steroids Hydrocortisone 4mg/kg (max 100mg) 6 hrly iv Switch to oral prednisolone once the patient is stable. Aminophylline Aminophylline has been shown to improve lung function and decrease the need for ventilation in severe asthma7. It has a place in the management of children not responding to aggressive beta2agonists and ipratropium therapy. It is administered intravenously: Loading dose 5mg/kg over 20 minutes (Omit if patient takes oral theophylline) Maintenance dose1mg/kg/hr (dilute to 1mg/ml in 0.9%Saline or 5%Dextrose). (If above 12 years of age, reduce to 800 micrograms/kg/hr) Monitor plasma levels and serum electrolytes. Reduce dose in liver disease and note potential for drug interactions. DRUG INTERACTIONS – Decreased effect/increased toxicity: (Decreased theophylline level Aminoglutethimide, barbiturates, carbamazepine, charcoal, high protein/low carbohydrate diet, hydantoins, isoniazid, I.V. isoproterenol, ketoconazole, October 2004-09-21 loop diuretics, phenobarbital, phenytoin, rifampin, smoking (cigarettes, marijuana), sulfinpyrazone, sympathomimetics Increased theophylline level Allopurinol, beta-blockers, calcium channel blockers, carbamazepine, cimetidine, ciprofloxacin, heart failure, corticosteroids, disulfiram, ephedrine, erythromycin, fever/viral illness, hepatic cirrhosis, influenza virus vaccine, interferon, isoniazid, loop diuretics, macrolides, mexiletine, oral contraceptives, propranolol, quinolones, thiabendazole, thyroid hormones, troleandomycin) IV Magnesium8 Indication: Intravenous magnesium is indicated in children not responding adequately to aggressive inhaled beta2agonists, ipratopium therapy and intravenous bronchodilators. It may be used as a treatment modality to try to avoid the need for ventilation. IV Magnesium Sulphate bolus Dose 0.2 mmol/ kg over 20 minutes Notes Dilute to maximum concentration 1mmol in 5mls (dilute with 0.9% Saline or 5% Dextrose). This use is as a one-off bolus in the early stages. It may be repeated after 12 hours but serum electrolytes and Magnesium levels should be checked first. Alternatively, an infusion of 0.4 mmol/ kg Magnesium Sulphate can be given over 6 hours (can repeat this infusion after 24 hours). Again, serum electrolytes and Magnesium levels should be checked before repeating the infusion. Heliox Unproven benefit in children9. October 2004-09-21 Intubation and mechanical ventilation should be avoided if at all possible. However, it may become necessary at any point from presentation and indications for intubation and mechanical ventilation are discussed below. Decision to Intubate If at all possible, mechanical ventilation should be avoided as this may increase bronchospasm, increase barotrauma and cause circulatory collapse. However, absolute indications for intubation include: Cardiac Arrest Respiratory Arrest Severe Hypoxia Rapid Deterioration in child’s mental state Progressive exhaustion despite maximal treatment is a relative indication Note that this decision is not based on arterial blood gas analysis but rather on clinical parameters. Induction & Intubation There is no uniform consensus on ventilation of Asthmatics but the following points should be remembered. 1) 50% of complications surrounding the mechanical ventilation of asthmatics occur around intubation. For this reason experienced senior help should be enlisted. Possible complications are due to gas trapping and include: i. worsening hypoxia ii. hypotension iii. pneumothorax and surgical emphysema iv. arrest v. tube malposition 2) Use Ketamine and consider rapid sequence induction using sedation and muscle relaxation aswell. (Ketamine acts as a bronchodilator as well as an induction agent). 3) Consider topical lignocaine to pharynx and larynx to avoid reactive bronchospasm. 4) Use a Cuffed tube (as high PIP’s are often required). October 2004-09-21 5) Avoid rapid breaths when ventilating by bag. Slow bagging will give time for adequate expiration and avoid dynamic hyperinflation. 6) CXR after intubation Ventilator Settings Tidal volume suggested 6 to 8 mls/kg Rate well below that expected for age (Suggest 8-16). Inspiratory time suggested 0.9-1.5s I: E ratio expiratory time must be longer to avoid dynamic hyperinflation. Adequate expiration can be assessed by termination of wheeze (or return to baseline on flow-time wave or return to plateau on capnography) before onset of the next breath (Suggest 1:3 to 1:5) PEEP High PEEP should be avoided to avoid dynamic hyperinflation. Initial PEEP should be set at ~60% of the initial intrinsic PEEP measured by the ventilator. (Suggest 4 cmH2O) PIP the PIP needed to achieve adequate tidal volumes is likely to be very high in asthmatic patients. Most of this pressure will not be transmitted to the alveoli and inspiratory plateau pressure may be a more accurate assessment of the amount of transmitted pressure.10 (Aim to keep plateau pressure < 30) Waveform A high inspiratory flow rate is needed if using volume ventilation. A square waveform is usually used October 2004-09-21 Permissive Hypercapnia The benefits of hypoventilating these patients when using mechanical ventilation have long been recognised.11 Lower rates and tidal volumes can be used to achieve permissive hypercapnia. PaCO2 up to 12 kPa have been allowed as long as the rise is not too rapid and the pH > 7.1 Contraindications to permissive hypercapnia include: 1. 2. 3. 4. Raised Intracranial Pressure Poor myocardial function Significant Metabolic acidosis Possible pregnancy Note: A rise in FIO2 is to be expected when utilising permissive hypercapnia PaCO2 should be allowed to rise slowly in increments of 1kPa every hour pH should be maintained above 7.1 Sodium Bicarbonate is seldom indicated in these patients Sedation and Paralysis Avoid Paralysis unless adequate ventilation cannot be achieved at acceptable inspiratory pressures. The combination of steroids and paralysis causes an unacceptably high rate of critical care myopathy and neuropathy. Check CK levels daily in paralysed patients Increased sedation is necessary if using permissive hypercapnia. Sedation should always be adequate enough to avoid patient-ventilator asynchronicity as this will worsen the hyperinflation. Refractory Hypoxaemia Other simple causes for hypoxia must be ruled out before resorting to the extraordinary treatment modularities outlined below. In particular, it is necessary to rule out atelectasis, pneumothorax, frequent β2agonists and hypovolaemia as causes of hypoxia. In some patients, simply reducing sedation, reducing the rate of ventilator breaths and allowing more patient-synchronised pressure supported breaths (ASB) can improve oxygenation. It is worthwhile trying this before resorting to extraordinary treatments. In the absence of other causes, the most likely cause for the hypoxaemia is the underlying V/Q mismatch of asthma. Possible treatment13,12 strategies include: 1. Ketamine infusion iv ketamine 2mg/kg bolus followed by an infusion at 0.2 to 2 mg/kg/hour 2. Magnesium infusion (see above). October 2004-09-21 3. Inhalational anaesthetics Isofluorane may be used as a bronchodilator but this requires a full-time anaesthetist. 4. Broncho-alveolar lavage or use of nebulised DNase has been tried to clear mucus plugging in extreme cases. Its role is uncertain. 5. ECMO The use of extra-corporeal membrane oxygenation in asthma is not certain. Currently, in the UK it used as a last resort 6. Consider proning Weaning The following clinical parameters can be used to assess clinical improvement of the ventilated asthmatic patient: i. Disappearance of pulsus paradoxsus (i.e. a drop of systolic bp of less than 10mm Hg in inspiration in a ventilated asthmatic patient is a sign of improvement). It is important to document daily the exact value of pulsus paradoxus in asthmatics. (This can be done by selecting arterial line on the main menu and choosing arterial cursor. The swing on the arterial line corresponding to inspiration will be obvious if present. Then the cursor can be moved to measure the peak arterial pressure in inspiration and expiration. The difference will be the exact value of the pulsus paradoxus). For example, below, pulsus paradoxus = 16mmHg. 94 78 ii. Good PaO2 in an FiO2 of 40% or less and a PIP of <35cmH20 iii. Minimal atelectasis on CXR iv. Decreased intrinsic PEEP (as measured by ventilator) When weaning, it is important to minimise patient – ventilator asynchrony as this will increase agitation and gas trapping. This can be achieved by reducing the rate of ventilator breaths and allowing more patient-synchronised pressure supported breaths (ASB). BIPAP/ASB or ASB alone are helpful at this stage. REFERENCES 1. British Thoracic Society Guidelines on Asthma. Thorax, 1997; 52: S2S8 2. Brooks et al. Significance of roentgenographic abnormalities in children hospitalised for asthma. Chest 1982 82: 315-318 3. Michele et al. A Prospective, randomised study of continuos versus intermittent nebulised albuterol for severe status asthmaticus in children. Critical Care Medicine 1993 21: 1479-1486 October 2004-09-21 4. 5. 6. 7. 8. 9. 10. 11. 12. Werner HA. Status Asthmaticus in Children. Chest 2001 119(6): 19131929 Zorc et al. Ipatropium bromide added to asthma treatment in the pediatric emergency department. Pediatrics 1999 103: 748-752 Rodrigo GJ and Rodrigo C. The role of anticholinergics in acute asthma treatment. Chest 2002 121(6) 1977-1987 Yung et al. Randomised Control Trial of aminophylline for severe acute asthma. Archives of Diseases in Childhood 1998 79: 405-410 Ciorallo et al. Intravenous Magnesium therapy for moderate to severe pediatric asthma: results of a randomised placebo controlled trial. Journal of Pediatrics 1996 129: 809-814 Carter et al. Evaluation of heliox in children with acute severe asthma, a randomised crossover trial. Chest 1996 109: 1256-1261 Leatherman et al. Life threatening asthma. Clinical Chest Medicine 1994 15:453 Dworkin et al. Mechanical ventilation for status asthmaticus in children. Journal of Pediatrics 1989 114: 545-9 Rice et al. Rapid response to isofluorane anaesthesia in refractory status asthmaticus. Archives of Diseases in Childhood 1998 78: 395-6 October 2004-09-21 SUMMARY CHART- ACUTE LIFE THREATENING ASTHMA ALL PATIENTS OXYGEN MONITOR ECG, SaO2 CONTINUOUS NEBULISED SALBUTAMOL NEBULISED IPATRIOPIUM EVERY 20 MINS IN FIRST HOUR AND 6 HOURLY THEREAFTER IV SALBUTAMOL OR IV AMINOPHYLLINE INTUBATE AT ANY STAGE IF: 1. Cardiac Arrest 2. Resp Arrest 3. Severe Hypoxia 4. Rapid deterioration in mental state Consider Intubation if progressive exhaustion CONSIDER IV MAGNESIUM IF INTUBATED SENIOR EXPERIENCED HELP ON INTUBATION RAPID SEQUENCE INDUCTION – CONSIDER KETAMINE, SUXAMETHONIUM AND MIDAZOLAM CONSIDER CUFFED TUBE SLOW BAGGING CXR POST INTUBATION IF VENTILATED ARTERIAL LINE CONSIDER PERMISSIVE HYPERCAPNOEA LONG EXPIRATORY TIMES LOW PEEP LAST RESORTS Ketamine infusion Magnesium infusion Broncho-alveolar lavage or DNAse Isofluorane ECMO