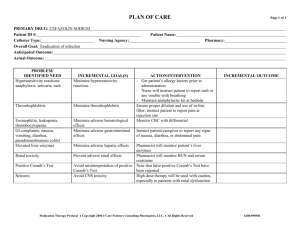
PROTOTYPE DRUG: Penicillin G Potassium (Pentids)
advertisement

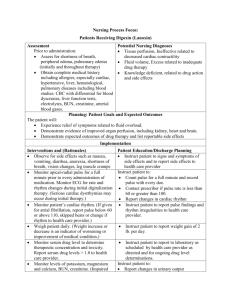
Nursing Process Focus: Patients Receiving Ciprofloxin (Cipro) Assessment Potential Nursing Diagnoses Prior to administration: Deficient Knowledge related to antibacterial drug therapy Obtain complete health history including allergies, drug history and possible drug Risk for fluid volume deficit related to GI interactions side effects from drug therapy Assess for presence or history of local or Diarrhea, related to effects of drug therapy systemic infections Obtain vital signs Obtain history of drug allergies Planning: Patient Goals and Expected Outcomes The patient will: Demonstrate understanding of drug therapy Demonstrate evidence of resolution of diagnosed infection after drug therapy is completed Maintain adequate fluid and electrolyte balance Implementation Interventions and (Rationales) Patient Education/Discharge Planning Safety for use by children under 18 not Instruct patient to contact health care established, due to possible action of Cipro provider at the first signs of tendon pain on the cartilage, usually the Achilles or inflammation. tendon: tendon rupture. (May interfere with bone development in children less than 18 years of age.) Avoid administering medications or foods Instruct patient to administer these that contain calcium, iron, or zinc such as substances and medications 2 hours antacids, dairy products, sucralfate or after ciprofloxacin. vitamin or mineral supplements, within 2 hours.. Administer with water and maintain Take each dose with a glass of water adequate fluid intake to avoid crystalluria. and drink several extra glasses of fluid daily to prevent formation of Monitor intake and output and urine pH. ciprofloxacin crystals in the urine. (The drug alters urinary pH and causes crystals to form in urine.) Monitor use of caffeine during drug Instruct patient to avoid caffeine intake therapy. (Absorption of Cipro is decreased during drug therapy. by caffeine.) Monitor plasma theophylline Inform patient that serum levels will concentrations for patients prescribed these need to be monitored. drugs. (The drug affects half-life of theophylline preparations.) Monitor patient for symptom of dizziness Advise patient to use caution when or lightheadedness. (This may occur due to driving, operating machinery, or the action of ciprofloxacin on the central performing other hazardous activities nervous system (CNS).) until effect of drug is known. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). Patients Receiving Trimethoprim (Bactrim, Septra) Assessment Potential Nursing Diagnoses Prior to administration: Infection, Risk related to contact with contagious agents (nosocomial or Obtain complete health history including allergies, drug history and possible drug community acquired) interactions Infection, Risk related to increased vulnerability secondary to diminished Assess for presence or history of systemic, respiratory or urinary tract infection immune response Assess intake and output Knowledge, Deficient, related to drug therapy and side effects Planning: Patient Goals and Expected Outcomes The patient will: Demonstrate reduction in symptoms related to the diagnosed infection Demonstrate understanding of drug therapy and side effects Remain free of symptoms of side effects of drug therapy Implementation Interventions and (Rationales) Patient Education/Discharge Planning Inform patient: Monitor renal function including BUN and creatinine values, and intake and That creatinine clearance tests and BUN output.(Drug can cause hematological may need to be monitored toxic effects, which are increased with To report changes in urinary elimination to kidney disease and also the elderly the health care provider population.) Advise patient to: Evaluate complaints of painful urination, flank pain, and fever. (Drug can change Drink 2.5-3 liters of fluid daily. the urine pH and could increase the Report painful urination, flank pain or patient’s risk for formation of renal fever to the health care provider calculi.) Monitor baseline and follow-up urinalysis, Instruct patient to continue medical CBC, platelet count, BUN and creatinine follow-up and laboratory test appointments clearance with long-term therapy. (To when receiving drug for extended period evaluate effectiveness of drug therapy.) of time. Observe for symptoms of adverse Instruct patient to report skin rash, sore reactions. (Evidenced in hematology and throat, fever, mouth sores, or unusual blood coagulation studies and by skin bleeding or bruising. manifestations.) Monitor skin integrity. (This drug can Instruct patient to avoid exposure to direct also increase patient’s sensitivity on the sunlight and sunlamps. skin to ultraviolet lights.) Monitor compliance with treatment Instruct patient to take drug as directed and regimen. (Full course of therapy is to complete full prescription. required. If patient stops medication before prescription is complete, symptoms may reoccur and this may increase resistance to further antibiotics.) Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). Nursing Process Focus: Patients Receiving Penicillin G (Pentids) Assessment Potential Nursing Diagnoses Prior to administration Infection, Risk for, related to weakened immune state or contact with pathogen Obtain complete health history including allergies, drug history and possible drug Knowledge deficient related to drug action interactions. and therapy treatment and prevention measures Assess for presence or history of local or systemic infection. Injury, Risk (anaphylaxis) for related to Obtain vital signs adverse effects of drug Planning: Patient Goals and Expected Outcomes The patient will: Remain free of signs of allergic reaction to drug therapy Demonstrate knowledge of drug action and side effects Demonstrate resolution to incidence of infection Implementation Interventions and (Rationales) Patient Education/Discharge Planning Monitor for evidence of allergic reaction Instruct patient: to drug. (Allergic reaction may occur Signs of allergic reaction including immediately or delayed beyond 72 itching, rash, respiratory distress hours.) To immediately contact the health care provider if allergic reaction occurs Monitor intake and output especially Advise patient to consult health care quantity and consistency of bowel provider before taking antidiarrheal movements. (Severe diarrhea may occur medication. These medications may due to the possible adverse effect from worsen or prolong diarrhea. Pseudomembranous colitis.) Evaluate patient’s understanding of drug Instruct patient to: therapy and administration. Take medication one hour before or two hours after a meal. Give medication on empty stomach to reduce destruction by gastric acid and Take medication with glass of water enhanced absorption. Take all of medication unless instructed to discontinue by the health care provider Evaluate patient for evidence of Instruct patient to notify the health care resolution of infectious process. (If the provider if symptoms persist or worsen. prescribed antibacterial is not effective another medication or different dosage may be required.) Observe for superinfection, especially in Instruct patient to report signs and susceptible patients including elderly, symptoms of superinfection. Symptoms debilitated, or immunosuppressed patient. may include: fever, black hairy tongue, (There is a high risk for superinfections stomatitis, loose, foul-smelling stools, due to normal flora reduced or vaginal discharge, or cough. eliminated.) Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes are met (see “Planning”). Nursing Process Focus: Patients Receiving Cefotaxime (Claforan) Assessment Potential Nursing Diagnoses Prior to administration Injury, Risk for (Allergic reaction) related to adverse reaction to drug Obtain complete health history including allergies, drug history and possible drug Infection, Risk for superinfection related to interactions effects of drug therapy Assess for presence of local or systemic Fluid volume, Risk for deficit, related to infection effects of drug on GI system Obtain vital signs Diarrhea, Risk for related to side effects of drug Obtain history of drug allergies Planning: Patient Goals and Expected Outcomes The patient will: Remain free of symptoms of allergic reaction Maintain adequate fluid balance Demonstrate absence of superinfection Maintain formed stool consistency Implementation Interventions and (Rationales) Patient Education/Discharge Planning Instruct patient to: Monitor for severe diarrhea caused by the disruption of normal bowel flora. Report loose stools or diarrhea. (May cause fluid electrolyte imbalance Avoid treating diarrhea with and superinfection of antibioticantidiarrheals as this can impede the associated pseudomembranous Colitis. process of eliminating “bad bacteria" Cultured dairy products with live active Check with health care provider before cultures, such as kefir or yogurt may be taking any probiotic products. used to help maintain normal intestinal flora. Supplements containing beneficial bacterial, such as acidophilus, are also available OTC). Monitor for rash, pruritus, or fever Instruct patient to report adverse (indicative of an allergic reaction to the reactions promptly. medications). Monitor intake and output carefully in Explain to patient purpose of required patients with compromised renal laboratory tests and schedule follow-up function or if receiving with health care provider. aminoglycoside. Monitor renal function with lab studies periodically during and after therapy. (Toxicity could occur from drug toxins that are unable to be excreted.) Monitor for superinfection, especially Instruct patient to report symptoms, with prolonged therapy. especially in debilitated or chronically ill patient. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see”Planning”). Nursing Process Focus: Patients Receiving Tetracycline HCl (Achromycin and others) Assessment Potential Nursing Diagnoses Prior to administration Body image, disturbed related to change in appearance Obtain complete health history including allergies, drug history and possible drug Noncompliance related to prolonged interactions. therapy Assess for presence/history of: Lyme Therapeutic regimen management, disease, pneumonia, acne vulgaris, Ineffective related to prolonged course of Typhus, Cholera, Rocky Mountain treatment spotted fever, Chlamydia, sexually Knowledge, Deficient, related to drug transmitted diseases, bladder infections, action and side effects Helicobacter Pylori ulcers Planning: Patient Goals and Expected Outcomes The patient will: Remain free of symptoms caused by the diagnosed infection. Maintain positive body image Demonstrate knowledge of drug therapy and side effects Demonstrate compliance with drug regimen Implementation Interventions and (Rationales) Monitor dental status when administered to children under age 8. (Drug may cause permanent discoloration of teeth, enamel defects, and bone growth retardation.) Administer with caution to patients with impaired kidney or liver function. (Could result in impaired metabolism and excretion.) Evaluate use of OTC products such as antacids, calcium supplements, iron products, and laxatives containing magnesium. (These products interfere with drug absorption). Evaluate patient understanding of drug therapy and administration. (Drug may cause photosensitivity and increase risk of sunburn. Tetracyclines can increase patient’s sensitivity of the skin to ultraviolet light.) Patient Education/Discharge Planning Instruct patient and caregivers to report evidence of tooth discoloration or dental abnormalities to health care provider. Instruct patient to: Report changes in urinary output Report for follow up care and lab tests of kidney and liver function and serum tetracycline levels. Instruct patient to consult with health care provider before taking over the counter drugs. Instruct patient to: Avoid direct exposure to sunlight during and after therapy. Wear protective clothing, sunglasses and sunscreen. Use an alternate form of birth control until all the medication is completed. Avoid taking drug with food, especially dairy products Report adverse effects of topical agent may cause irritation to eyes, nose, mouth, or allergic reaction. To report worsening of infection and burning sensation to health care provider. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes are met (see “Planning”). Nursing Process Focus: Patients Receiving Erythromycin (E-mycin, Erythrocin) Assessment Potential Nursing Diagnoses Prior to administration: Knowledge, Deficient related to disease process and drug therapy Obtain complete health history including allergies, drug history and Infection, Risk for related to superinfection possible drug interations. Fluid volume, Risk for Deficit related to Assess for presence/history of local or effects of drug on GI system systemic infection Diarrhea, Risk forrelated to effect of drug Obtain vital signs therapy Obtain history of allergic reaction to Injury, Risk for (anaphylaxis) , related to drugs adverse reaction to drug Planning: Patient Goals and Expected Outcomes The patient will: Demonstrate knowledge or drug therapy and treatment regimen Remain free of drug induced diarrhea Maintain adequate fluid balance Maintain absence of allergic reaction to drug Implementation Interventions and (Rationales) Patient Education/Discharge Planning Contraindicated in patients with hepatic Instruct patient to report history of medical disease. (Because the metabolism of problems to health care provider. erythromycin ethylsuccinate (EES) is mainly by the liver, it increases the patient’s risk for toxicity.) Monitor WBC, temperature, cultures, and Instruct patient: perform infection-focused physical To report fever and worsening symptoms examination. (To determine effectiveness of infection. of drug therapy.) To report for follow-up examinations. Instruct patient: Evaluate patient understanding of treatment regimen. (Patient must To complete full prescription even if complete full course of therapy to prevent feeling better or symptom free. bacterial resistance.) Take with full glass of water, on an empty stomach one-hour before or two hours after meals. Avoid taking with or just after acidic fruit juices or carbonated drinks. Monitor for evidence of G.I. distress. Instruct patient to report past history of GI (May require alternate form of problems to health care provider. medication.) Monitor for ototoxicity in patients receiving high dose, older adults, female and history of kidney or liver dysfunction. Instruct patient to immediately report dizziness, vertigo, nausea, tinnitus, roaring noises, or hearing impairment to the health care provider. Observe for signs and symptoms of Instruct patient to report diarrhea, superinfection by overgrowth of nonabdominal pain, vaginal discharge, or susceptible bacteria or fungi. fever. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). Nursing Process Focus: Patients Receiving Gentamicin (Garamycin) Assessment Potential Nursing Diagnoses Prior to administration: Injury, Risk for related to renal insufficiency related to aminoglycoside Obtain complete health history including allergies, drug history and possible drug therapy interactions Injury, Risk for related to disturbances of balance and impaired ability to detect Assess for presence/history of local or systemic infection environmental hazards Obtain vital signs Knowledge, Deficient related to drug therapy and side effects Obtain history of drug allergies Planning: Patient Goals and Expected Outcomes The patient will: Maintain normal renal function throughout drug therapy. Demonstrate knowledge of drug therapy and side effects Remain free of physical injury Implementation Interventions and (Rationales) Patient Education/Discharge Planning Instruct patient to provide thorough history of Use with caution with impaired renal medical conditions and treatment to health care function or neuromuscular disorders. provider. (Renal impairment can increase the risk of toxicity with this drug. Patients with neuromuscular disorders may experience greater muscular weakness due to possible neuromuscular blockade with the drug’s action.) Monitor for signs of renal toxicity including unusual appearance of urine (dark, cloudy) intake and output ratio, and the presence of edema. Report immedately Monitor for evidence of ototoxicity including headache, dizziness or vertigo, nausea or vomiting with motion, ataxia, nystagmus, tinnitus, roaring noises, sensation of fullness of ears and hearing impairment. Monitor peak and trough drug levels. (Aminoglycosides have a narrow therapeutic range.) Observe for symptoms of neurotoxicity or neuromuscular blockade. Instruct patient to: Increase fluid intake of 2000 ml per day. Report evidence of decreased urinary output to the health care provider Instruct patient to notify health care provider if changes in hearing occur. Explain to patient that frequent serum drug therapy levels are necessary to prevent and monitor for complications. Instruct patient to immediately report muscle twitching, numbness, seizures, weakness, or difficulty breathing to the health care provider. Observe for signs and symptoms of Instruct patient to report diarrhea, bacterial overgrowth due to drug’s effect anogenital itching, vaginal discharge, to “kill” all bacteria, even normal flora stomatitis, or glossitis. that can lead to superinfection. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). Nursing Process Focus: Patients Receiving Vancomycin (Vancocin) Assessment Potential Nursing Diagnoses Prior to administration: Sensory perception, Disturbed related to ototoxicity Obtain complete health history including allergies, drug history and possible drug Injury, Risk for deep vein thrombosis interactions related to chemical irritation of vein Assess for presence or history of infections Knowledge, Deficient, related to drug resistant to other antibiotics therapy and side effects Obtain history of hearing loss, impaired renal function Obtain history of cardiovascular disease Obtain history of hearing loss Planning: Patient Goals and Expected Outcomes The patient will: Demonstrate therapeutic response to drug therapy Remain free of phlebitis Maintain normal hearing acuity Implementation Interventions and (Rationales) Patient Education/Discharge Planning Inform patient: Evaluate hearing acuity. (Contraindicated with previous hearing loss due to drug’s That audiometry tests will be done to ototoxic effects.) prevent complications from possible ototoxicity. To report symptoms of hearing loss, buzzing in ears Monitor peak and trough vancomycin levels to ensure safe and effective dosage. Inform patient about purpose of laboratory studies. Monitor renal status. (Dosage is adjusted with renal insufficiency.) Advise patient of importance of laboratory studies to establish baseline renal function and to monitor function during and after treatment. Monitor IV site carefully. (Drug is irritating to tissues and causes necrosis and severe pain with extravasations.) Instruct patient to report pain or other symptoms of discomfort immediately during intravenous infusion. Monitor for proper use of medication. Patient must take medication as prescribed and complete full course of treatment. Do not take other antidiarrheal preparations. Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”). Nursing Process Focus: Patients Receiving Isoniazid (INH) Assessment Potential Nursing Diagnoses Prior to administration: Sensory perception, Disturbed related to peripheral neuritis and optic neuritis Obtain complete health history including allergies, drug history and possible drug Knowledge, Deficient, related to drug interactions therapy and side effects Assess for presence/history of Positive Therapeutic regimen management, tuberculin skin test, positive sputum culture Ineffective related to long term therapy or smear, close contact with person recently infected with tuberculosis, AIDS, receiving immunosuppressant drugs, alcohol abuse, liver or kidney disease Planning: Patient Goals and Expected Outcomes The patient will: Demonstrate adherence to extended drug therapy Demonstrate negative sputum cultures indicating effective drug therapy Demonstrate understanding of drug therapy Implementation Interventions and (Rationales) Patient Education/Discharge Planning Instruct patient to: Monitor liver function. (Contraindicated in patients with acute liver disease or history Provide accurate and complete medical, of isoniazid-related liver damage.) medication and treatment history. Avoid alcohol intake during drug therapy Report signs of liver impairment to health care provider, including jaundice, itching, fatigue Monitor for negative sputum cultures. Instruct patient to follow through on Change noted within 2-3 weeks. (To prescribed lab tests. evaluate effectiveness of drug therapy.) Instruct patient to: Monitor for presence of peripheral neuritis related to pyroxidine deficiency. Take pyrodoxine supplement to reduce (Pyrodoxidine (vitamin B6) deficiency risk of side effects. causes neurotoxic effects.) Report symptoms of numbness, tingling, or burning of feet to the health care provider Evaluate diet for ingestion of foods Advise patient to avoid foods such as containing tyramine. (Ingestion of aged cheeses, smoked fish, tuna, tyramine-containing foods may cause sauerkraut juice, and yeast extracts. palpitation, flushing and BP elevation, and histamine-containing foods may cause exaggerated drug response with headache, palpitation, sweating, flushing, itching, or diarrhea.) Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that patient goals and expected outcomes have been met (see “Planning”).