EM Legends
advertisement

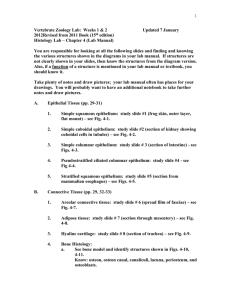
Electron Micrograph Legends Epithelium EM #1, 2, 4, 11 Use these micrographs to review the structure of organelles. Be sure you can recognize favorable sections of the nucleus, mitochondria, and rough ER. EM #0 JUNCTIONS Review the structure of occluding and communicating junctions. EM #70 SIMPLE SQUAMOUS EPITHELIUM (Rhodin 16-6) The endocardium, the simple squamous epithelial lining of the heart, can be seen at the top of this section. Under it, you can see connective tissue, which we will study next time. Note how thin the epithelium is. EM #17 SIMPLE COLUMNAR EPITHELIUM (Rhodin 3-8) You can see that this is a simple epithelium, as it is one cell layer thick, and columnar, as the cells are tall. Note the basal lamina at the base of the epithelium. You can see the apical area where junctions are located. This cell also has very short apical microvilli. EM # 128 SIMPLE CUBOIDAL EPITHELIUM (Rhodin 32-13) Here we see a kidney tubule cut in cross section. Fingerlike microvilli can be seen. A similar structure in the intestine gives rise to the "striated border" we saw in the LM. EM #18 3-15) STRATIFIED SQUAMOUS KERATINIZING EPITHELIUM (Rhodin You can appreciate that this epithelium (skin) is stratified (has multiple layers of cells), and that the layers near the surface (at the top of the micrograph) have keratinized (lost their nuclei, and become a layer of keratin). The spiny appearance of cells deeper in the epithelium can also often be seen in the light microscope. They are points of cell-cell attachment, made more obvious by shrinkage during preparation. What junctions are found here? (EP2) EM #94 STRATIFIED SQUAMOUS NONKERATINIZING EPITHELIUM (Rhodin 26-10) Compare this micrograph to the previous one. This is the lining of the mouth, where it is no longer necessary to have an outer keratinized layer to protect against desiccation, as it was for skin. Thus, the outermost layer is still cellular and contains a nucleus. Note again the spiny appearance of the cells, due to the desmosomal attachments. EM # 101 PSEUDOSTRATIFIED EPITHELIUM (Rhodin 31-22) The definition of a pseudostratified epithelium is one in which there are multiple levels of nuclei, but all cells extend to the base of the epithelium. In this micrograph, you can find cells with nuclei at different levels which can be traced down until they are at least close to the base of the epithelium before some of them go out of the plane of section. Note also the apical cilia and basal bodies. You can see that the goblet cells are not ciliated, and are polarized for secretion, i.e., the nucleus is basal to the clear secretion granules, which will be released into the lumen at the top of the micrograph. EM #102 (Rhodin 31-25) This is the apex of the epithelium seen in EM #101, cut in a different plane of section, as indicated by the line in #101. You can see cross sections of the cilia, and also the secretion granule-filled apex of an occasional goblet cell. Connective Tissue #20 MESENCHYMAL CONNECTIVE TISSUE (Rhodin, Fig. 7-1). Note the paucity of collagenous fibrils and the large number of mesenchymal cells. Is there a pronounced cytological difference between a fibroblast and a mesenchymal cell? (CT6) #21 DENSE CONNECTIVE TISSUE (no Rhodin counterpart) Note the alternating layers of fibroblasts and collagenous bundles. Make sure you can see the difference between cross sectioned and longitudinally sectioned collagenous fibrils. In dense connective tissue, which cell is most common? (CT7) #22 LOOSE & DENSE CONNECTIVE TISSUE (Rhodin, Fig. 31-68) This is an excellent low power example of the roles connective tissue serve. Observe how the connective tissue fibers and cells "embed" other tissues, such as nerves, smooth muscle, and serve as base for epithelium. Blood vessels are also encircled by connective tissue, and an extension of the epithelium -- the glands. Where are the nuclei of the fat cells? (CT8) #23 FIBROBLASTS (no Rhodin counterpart) Observe the large amount of RER in these cells. Is this an indication of an active or inactive cell? (CT9) Test your ability to identify different organelles at this magnification! #24 COLLAGEN & ELASTIN (CROSS SECTION) (Rhodin, Fig. 7-7) In this cross section of connective tissue fibers, note the rather equal diameter of all collagenous fibrils. Observe the two components of the elastic fiber. #25 COLLAGEN & ELASTIN (LONGITUDINAL SECTION) (no Rhodin counterpart) Observe the branching nature of the elastic fiber and the "mantle" of elastic microfibrils. The cross banding of the collagenous fibrils is easily observed. #26 CONNECTIVE TISSUE CELLS (no Rhodin counterpart) In this micrograph of loose connective tissue (core of intestinal villus, the lamina propria) numerous (labeled) cells of the connective tissue are present. Note the relative size of the different cell types, their shapes, amount of RER and variously sized granules and inclusions. Then use your text and atlas to review the diagnostic features of each connective tissue cell present in the micrograph. Note the paucity of collagen fibrils. What was present in the "empty" looking intercellular space? (CT10) #27 MAST CELL (no Rhodin counterpart) Mast cell granules exhibit ultrastructural differences that are species specific. The human mast cell contains secretory granules which have the specific ultrastructure illustrated, the significance of which is unknown. What are the secretory products of the mast cell? (CT11) #28 FAT CELLS (no Rhodin counterpart) Study the formation of fat droplets. Note that each fat cell is enclosed by a thin basal lamina. Muscle #41 SKELETAL MUSCLE (longitudinal section) (Rhodin 11-5) Find the skeletal muscle nuclei and note their peripheral location. Note the intimate contact between capillaries and muscle cells, and be sure you can tell where one muscle cell or fiber stops and another begins (you can see parts of four fibers in this picture). Make sure you known which is the longitudinal axis of the cell. Identify sarcomeres, A bands, I bands, Z lines and H zones. Note that, as you saw at the LM level, the individual myofibrils do not line up perfectly across the fiber. #42 SKELETAL MUSCLE (cross-section) (Rhodin 11-6) Note location of muscle fiber nuclei. You can see cross sections of A bands (darker) and I bands (lighter) side by side in the same cell because of the fact that the myofibrils don't line up perfectly. Identify the approximate outline of a single myofibril. #43 SKELETAL MUSCLE (Longitudinal section) (Rhodin 11-10 is similar) Identify a sarcomere. Relate the sarcomeric structure seen in the LM to the structure seen here. Note that there is also lots of glycogen in the region between the two myofibrils in this picture, a storage form for glucose (which is metabolized to provide energy for muscle contraction). #44 SKELETAL MUSCLE (cross-section) (Rhodin 11-11) Review the reasons for the fact that you can see only cross-sectioned thin filaments in the I bands, whereas the A bands may contain both thin and thick filaments. Thus, you should be able to tell at which level each of these myofibrils was cut. Note the abundance of the sarcoplasmic reticulum. #45 CARDIAC MUSCLE (longitudinal section) (Rhodin 11-26 is similar) Note central location of muscle nuclei. Note the "stacks" of mitochondria between myofibrils. Cardiac muscle is even richer than skeletal muscle in mitochondria (again, important for energy production). An intercalated disc is present in the upper left region of the picture. #46 CARDIAC MUSCLE (intercalated disc) (Rhodin 11-27 is similar) Note the irregular course of the intercalated disc. In this preparation, the I bands are very short. Does this reflect a relaxed or contracted state of the sarcomere? (MU3) Review the types of junctions present in an intercalated disc and their functions. #48 SMOOTH MUSCLE (no Rhodin equivalent) Study the orientation of the smooth muscle layers in the intestine. The diagram will help you understand the patterns which arise from longitudinal and cross-sections. #50 SMOOTH MUSCLE (Rhodin 11-44) Here you can see the filaments in cross-section, appearing as dots. Also, the dark areas which are membrane-associated are called dense plaques and are sites of filament attachment. Nervous System #51 Motor neuron (ventral horn, rat). In this electron micrograph, note some of the features you saw in ventral horn motor neurons with the light microscope, such as the large, pale nucleus, prominent nucleolus, Nissl bodies, dendrites and axon. Adjacent to the neuron, note myelinated axons of various sizes, and also that there is no space between cell processes--all space is occupied either by the processes of neurons or glia, or by capillaries (capillaries are somewhat swollen here because the tissue was fixed by perfusion). (Rhodin, Fig. 13-1; also W pgs 118-9, 7.3). #52 Nucleus and cytoplasm of a neuron (Purkinje cell, rat). Details of neuron ultrastructure are shown in this electron micrograph. In the nucleus, note the small amount of heterochromatin (suggesting broad transcriptional activity) and the prominent nucleolus (abundant production of ribosomes and presumably, therefore, of proteins). The "Nissl substance" is well developed, and is made up of numerous free polysomes as well as rough ER cisternae (Rhodin, Fig. 13-2). #53 Nerve Process (CNS). In this field you see two oligodendrocytes, the cells that make myelin in the CNS, surrounded by numerous myelinated axons of various size, cut in cross section. (Rhodin, Fig. 15-3). #54 Nerve Process (PNS). Note the numerous myelinated axons of various size. Associated with each is the Schwann cell that produced the myelin (occasionally the Schwann cell nucleus is in the plane of section). In contrast to the CNS, where a single oligodendrocyte can myelinate portions of numerous axons, in peripheral nerves a particular Schwann cell myelinates only a segment of a single axon. On the other hand, a Schwann cell can support several non-myelinated axons (you will see this best in EM # 55). Between the axons you will see delicate connective tissue and an occasional fibroblast, which constitute the endoneurium. At the periphery of the fascicle, observe the perineurium, made up of several layers of flattened cells; it is a highly specialized layer that acts as a barrier and protects the nerve from the environment. (Rhodin, Fig. 12-19; also, W pg. 122, 7.5). #55 Nerve Process (PNS), (autonomic nerve, kidney, rat). Most of the axons seen in this electron micrograph of an autonomic nerve are non-myelinated. All of the non-myelinated fibers are embedded in grooves in the surface of Schwann cells (in some cases there may be more than one axon per groove), with each Schwann cell thus supporting a considerable number of these small axons. Although the axons are very close together, you will observe thin partitions of Schwann cell between them. Also note a few myelinated fibers and a very sparse endoneurium. A very thin perineurium surrounds the nerve. (Rhodin, Fig. 13-28). #57 Schwann cell and cross-sectioned myelinated axon (sciatic nerve, rat). In this cross section of a myelinated nerve process, note the axon, containing microtubules and neurofilaments, and bounded by a plasma membrane ("axolemma"). Outside the plasma membrane of the axon is the myelin sheath, which you will remember is composed of tightly-wrapped plasma membranes of the Schwann cell. Also note the nucleus and cytoplasmic organelles of the Schwann cell. Remember that the myelin is part of the Schwann cell, not of the axon. (Rhodin, Fig. 13-18). #58 Node of Ranvier (sciatic nerve, rat). The myelin is much better preserved in this electron micrograph than in the earlier light microscope slides, but otherwise you are viewing the same structures. Remember that the node of Ranvier is actually a short segment of the axon that is bare at the junction between two Schwann cells, making "saltatory conduction" possible. Note the manner in which the myelin ends in each Schwann cell at the junction, by a "peeling off" of successive myelin layers which come to lie against the axon as small cytoplasmic swellings. (Rhodin, Fig. 13-22; also, W pg. 125, 7.7). Cardiovascular System #69 EPICARDIUM & MYOCARDIUM Note the very thin, squamous mesothelium, provided with numerous microvilli. The epicardium (visceral layer of pericardium) is rather thin, but contains blood vessels as well as lymphatics. One such lymph capillary (which is impossible to identify as such based upon this one micrograph) and part of an epicardial vein are seen here. Observe the dense arrangement of myocardial cells, and the numerous blood capillaries which permeate the myocardium. (Rhodin, Fig. 16-8). #70 ENDOCARDIUM Observe how thick the endocardium is in comparison with the epicardium. At this magnification, it is not possible to see the structural difference between smooth muscle cells and fibroblasts. However, it should be remembered that the endocardium does contain smooth muscle cells in addition to some nerves and impulse conducting cells (not seen here) usually located immediately adjacent to the myocardium. Is there a difference in endocardial thickness between the atria and ventricles? (CV4) (Rhodin, Fig. 16-6). #71 ATRIOVENTRICULAR VALVE Note that the valve is composed of two apposing layers of endocardium. The core of the valve contains loose connective tissue near the surface of the atrioventricular orifice, and a thick, dense connective tissue plate on the opposite side. Note the absence of smooth muscle cells or capillaries within the substance of the valve. What covers the valve leaflets? (CV5) PATHOLOGY: The small dense spherules in the connective tissue represent the beginning of a calcification process - an aging phenomenon. (Rhodin, Fig. 16-10). #72 CHORDA TENDINEA In this electron micrograph, study the arrangement of collagenous and elastic fibers in this small tendon. The endocardium is reduced to the layer of endothelial cells. Where are the cardiac muscle fibers? (CV6) (Rhodin, Fig. 1612). #73 IMPULSE CONDUCTING SYSTEM - PURKINJE CELL (FIBER) Note that the term “Purkinje fiber” is used more often than “Purkinje cell” in the impulse conducting system. Observe the great width of the Purkinje fibers in this part of the conducting system, and compare them with the width of the ordinary myocardial cells. The Purkinje fibers have more glycogen but fewer myofibrils. Note the extensive lateral contact between neighboring Purkinje fibers. It is believed that this relationship increases the rate of impulse propagation. (no Rhodin counterpart). #74 ELASTIC TYPE ARTERY - AORTA (cross sectioned) Note the alternating layers of connective tissue and smooth muscle cells in the media. If there are no fibroblasts in the media, which cell is involved in the synthesis and maintenance of the collagen and elastic fibers as well as vascular proteoglycans? (CV7) The junction between the intima and media is difficult to identify! (Rhodin, Fig. 16-16). #75 MUSCULAR TYPE ARTERY (cross section) Note that the intima in this type of artery consists of only the endothelium. Note also, the obvious internal elastic lamina, the paucity of elastic components within the media, and the arrangement of smooth muscle cells. (Rhodin, Fig. 1625). #76 INTIMA & MEDIA The narrow space between adjacent endothelial cells, although provided with junctional complexes, is used for some transendothelial passage of metabolites and fluid. Find the interruption (fenestra) of the internal elastic lamina. This is also said to facilitate transport of metabolites to and from the media. Review the structure of the smooth muscle cell. (Rhodin, Fig. 16-26). #77 HELICINE ARTERY This artery is unusual in that the intima contains longitudinally arranged smooth muscle cells. (Rhodin, Fig. 16-28). #78 ARTERIOLE Note that the media in an arteriole consists of only one or two layers of smooth muscle cells. An adventitia may not be present. CAUTION: Although this arteriole (afferent arteriole of the renal corpuscle of the kidney) contains a thin internal elastic membrane, many arterioles do not. (Rhodin, Fig. 16-30). #79 CAPILLARY NETWORK The capillary bed consists of highly anastomosing endothelia-lined tubes, seen here in a longitudinal view. It is not difficult to understand the basic function of a capillary when one sees the extremely thin endothelial wall separating the blood from the extravascular tissue space. (Rhodin, Fig. 16-35). #80 CAPILLARY (muscle tissue type) Note abundance of micropinocytotic vesicles. (Rhodin, Fig. 16-36) #16 CAPILLARY (fenestrated type) Note the diaphragms within fenestrations. (Rhodin, Fig. 16-37). #81 CAPILLARY (nervous tissue type) Note the lack of vesicles, a reflection of a true blood-brain barrier. Remember that true tight junctions restrict transendothelial passage of metabolites and fluid. (Rhodin, Fig. 15-25). #82 POSTCAPILLARY VENULE This is an electron micrograph of a portion of a microcirculatory bed. Observe the addition of pericytes to the wall of the venous capillary (those capillaries that empty into venules) and the postcapillary venule -- as opposed to the situation in true capillaries. (You do not have to distinguish subtle differences in microcirculatory bed structure!) Remember that this is the segment of the microvascular bed where lymphocytes and polymorphonuclear leukocytes exit the vascular systems by traversing the vessel wall by the process of diapedesis. (Rhodin, Fig. 16-42). Blood #61 ERYTHROCYTE (RBC) RBC's are cut in several planes of section in this micrograph. Why does the one sectioned in the equatorial plane appear to have a large hole in the middle? (BL1) Note the two platelets--are they cut transversely or equatorially? (BL2) Note that neither RBC's nor platelets contain a nucleus, in contrast to the lymphocyte. The plasma has a flocculent appearance, because the protein concentration is high and has been precipitated by the fixative. #62 NEUTROPHIL OR POLYMORPHONUCLEAR LEUKOCYTE (PMN) Remember the multilobed nucleus and the abundance of dense heterochromatin that you saw in the blood smear. The cytoplasm contains both azurophilic and specific granules. The distinction between these two granule populations is not very clear in this micrograph, and you are not responsible for recognizing granule types. (Rhodin, Fig. 5-10). #63 EOSINOPHIL The bilobed nucleus, in combination with the specific granules that contain crystalloids, make it possible to identify this cell as an eosinophil. #64 BASOPHIL Note that the granules are true secretory granules, discharged by exocytosis. The nucleus is oval or kidney-shaped. #65 LYMPHOCYTE Note the small amount of cytoplasm and sparse organelles (except ribosomes). Cartilage #29 HYALINE CARTILAGE (Rhodin, Fig. 8-2) Note the abundance of intercellular matrix. Are capillaries present in the matrix? (CA2) Study the development of chondrocytes from chondroblasts. #30 CHONDROCYTE (HYALINE CARTILAGE) (Rhodin, Fig. 8-3) Note that the collagenous fibrils are partially obscured and lack obvious periodicity. What type of collagen is present in the matrix? (CA3) Note the many cell organelles in this very active chondrocyte. #31 CHONDROCYTE (FIBROUS CARTILAGE) (no Rhodin counterpart) Extracellular collagenous fibrils are coarser in fibrous cartilage than in hyaline cartilage, and do show periodicity. (They are made of type I collagen.) Observe the varied directions of collagenous bundles. The amorphous matrix surrounding the chondrocyte helps distinguish this cell from that of a fibroblast in dense connective tissue. Check back to chart #23. #32 ELASTIC CARTILAGE (no Rhodin counterpart) Find the elastic components in the matrix. The delicate intracellular filaments are intermediate (vimentin) filaments. Bone and Bone Formation #33 INTRAMEMBRANOUS BONE FORMATION (Rhodin, Fig. 10-1) Why is this sometimes called "direct" bone formation? Why is the term "membrane" used here? Would you expect to find chondrocytes in this section? Find the capillaries. What is their significance? Make sure you know the structural and functional differences between an osteoblast and osteocyte. #34 INTRAMEMBRANOUS BONE FORMATION (Rhodin, Fig. 10-5) Observe (and remember) that the bone formation which occurs from the periosteum of the diaphysis of long bones is identical to the process of intramembranous bone formation. In this unique micrograph, study the differentiation of osteoprogenitor cells to osteoblasts and subsequently to osteocytes. What is osteoid? (BO7) Note the formation of long cell processes as the osteoblast (lower right corner) prepares for the transformation into an osteocyte. Find the cell process which is already located in a canaliculus. #35 OSTEOCYTE (Rhodin, Fig. 9-10) The calcium crystals of the bone matrix were removed in this preparation by a decalcification process. Note how coarse the collagenous fibrils are, and the difficulty in visualizing the periodicity of the fibrils (probably due to the process of mineralization). #36 ENDOCHONDRAL BONE FORMATION (Rhodin, Fig. 10-14) Note that the bony collar is formed from the cells of the periosteum/perichondrium. Central chondrocytes of this cartilage model break down and die because the cartilage matrix becomes calcified. Subsequently, periosteal blood vessels break (erode) the bony collar and invade the lacunae of the dying chondrocytes. Find these invading blood vessels. #37 ENDOCHONDRAL BONE FORMATION (epiphysis) (Rhodin, Fig. 10-17) In the epiphyseal growth plate, continuous growth of hyaline cartilage, break-down of calcified cartilage, ingrowth of blood vessels, bone formation on the calcified cartilage matrix, and finally resorption of this bone and formation of bone marrow occurs. Make sure that you identify each of these steps and that you understand what happens. #38 ENDOCHONDRAL BONE FORMATION (Rhodin, Fig. 10-18) In this enlargement of rectangular area in chart #37, study the transition that occurs in the chondrocytes as they change from very active to hypertrophied and dying. Why do the chondrocytes die? (BO8) #39 OSTEOCLAST (Rhodin, Fig. 9-19) The osteoclast is a very large cell (multinucleated) that sits on the surface of bone matrix. Note the many lysosomes and phagocytic vacuoles. What is the functional significance of these structures? (BO9) Note the proximity of the osteoblast. Remember that bone deposition can take place very near bone resorption. This explains the juxtaposition of osteoclast and osteoblast. Most osteoclasts are thought to arise by fusion of monocyte-macrophages. #40 HAVERSIAN CANAL (Rhodin, Fig. 9-22) Note the "inactive" appearance of endosteal cells. The presence of a macrophage in the Haversian canal indicates the potential eroding function of the endosteal lining of the canal. Why are blood vessels so important in bone? (BO10) Respiratory Sysytem #100 TRACHEA (Rhodin Fig. 31.21) Look at the pseudostratified epithelium with numerous goblet cells, which will be observed at higher power in the next wall chart (#101). Beneath the epithelium, note the region which corresponds to the basement membrane we looked at with the light microscope (this is a good illustration of why "basal lamina" and "basement membrane" are not synonymous). Below that, note the connective tissue, with fibroblasts and blood vessels. #101 RESPIRATORY EPITHELIUM (TRACHEA) (Rhodin Fig. 31.22) Compare the morphology of the goblet cells with that of the other cells of the epithelium. Note that most of them are filled with secretory product (mucus), and that they do not have cilia. The line indicates the plane of section on the next wall chart, #102. #102 CROSS SECTIONED CILIA (TRACHEA) (Rhodin Fig. 31.25) The dashed line indicates the outline of one cell (see previous wall chart #101 for plane of section). Review the fine structure of the cilium. Note the tops of the goblet cells protruding between the cilia. #103 BRONCHUS (similar to Rhodin Fig. 31.34) Note that the epithelium, although still pseudostratified, is not as tall as in the trachea (wall chart #100). Smooth muscle separates the lamina propria from the submucosa. There are numerous glands in the submucosa. Hyaline cartilage, with perichondrium, can be seen. #104 BRONCHIOLE (Rhodin Fig. 31.39) The smooth muscle layer is relatively thick, and again separates lamina propria from submucosa. No cartilage is present in bronchioles. #105 ALVEOLI (Rhodin Fig. 31.46) Study the organization of the alveolus. Note that individual alveoli border on each other and therefore share the wall which is referred to as alveolar septum. Within the septum are found capillaries. Be able to recognize type I cells , type II cells, and macrophages: There is a macrophage filled with inclusions in this picture. There is also a type II cell, which secretes surfactant, and can be identified on the basis of its lamellar or multilamellate bodies, which cannot be seen well at this magnification (also see B&F pg 236). The type I cell lining the alveolus is also better identified at higher magnification. Lymphatic System These micrographs should help you to understand the organization of lymphoid organs, they are among the best available anywhere. #89 LYMPH NODE - NODULE IN CORTEX The nodule has a central germinal center and a peripheral corona of small lymphocytes. Find the subcapsular sinus and the reticular cells of the node. Identify several macrophages in the nodule (Rhodin, Fig. 17-14). #90 LYMPH NODE - MEDULLARY SINUSES Observe the loose arrangement of lymphoid tissue in the medulla of lymph nodes. The sinuses interconnect and their lumens are traversed by reticular cells, some of which can trap antigens and some of which are true phagocytes. Blood vessels are restricted to the medullary cords. Plasma cells occur abundantly in the cords. Review the function and origin of plasma cells. Note that the free, circulating lymphocytes are either small or medium size. Where are the large lymphocytes? (LY 3) Did you see free macrophages in the medullary sinuses of your sections? (LY4) They frequently accumulate in this region. (Rhodin, Fig. 17-19). #93 THYMUS Note that the thymus does not have lymph nodules. However, the small lymphocytes (thymocytes) are aggregated in the cortex, and the larger, epithelial reticular cells are concentrated in the center (medulla), giving the appearance of a "nodular" area. Remember Hassall's corpuscles are found only in the thymus. (no Rhodin counterpart). #91 SPLEEN - RED & WHITE PULP Note the very dense arrangement of lymphoid cells in the white pulp, and the loose arrangement of reticular cells, some lymphoid cells and extravasated erythrocytes in the pulp cords among the venous sinuses. Note the marginal zone. (Rhodin, Fig. 18-6). #92 SPLEEN - DETAIL OF RED PULP In this unique micrograph of the red pulp, one blood capillary is seen to have an open end, discharging formed elements of the blood into the extravascular space (pulp cords). Find the venous sinuses and observe the movement of erythrocytes across the wall. The presence of many macrophages in the interstitial space of the red pulp is obvious. What are the functions of the red pulp? (LY5) (Rhodin, Fig. 18-13). Urinary System #126. Survey view of kidney cortex. Note that the brush border is present in proximal convoluted tubules, but not in distal convoluted tubules or in collecting ducts. There are numerous peritubular capillaries. This section of the renal corpuscle does not happen to include either the vascular or urinary poles. Note the abundant glomerular capillaries. (Rhodin 32-3). #127. Renal corpuscle. Study the architecture of the glomerulus in this section of renal corpuscle. Review the organization and function of the glomerular endothelium, basement membrane and the podocytes. What is the location of mesangial cells relative to the basal lamina? (UR1) (The vascular pole is included in the plane of section, but not the urinary pole. The juxtaglomerular cells are secretory cells, derived from smooth muscle cells of the afferent arteriole. The macula densa shown here is cut in tangential section passing only through its wall, and does not include the lumen (the rest of the tubule is out of the plane of section). You can at least see the closely-packed nuclei that are characteristic of this modified portion of the distal tubule. (Rhodin 32-9). #128. Proximal convoluted tubule. Note the brush border, composed of closely packed microvilli. Note the numerous mitochondria, in association with basal infoldings of the plasma membrane. Lateral cell membranes are not clearly visible because of extensive interdigitation of neighboring cells (Rhodin 32-13). #129. Distal convoluted tubule. Compare this with the proximal tubule seen in the previous micrograph. (Rhodin 32-19). Integumentary System #18 EPIDERMIS Review the layering of the epidermis. Remember that there is a continuous process of cell migration and differentiation from the basal cell layer to the most superficial layer. Review the features of the epidermal-dermal junction. (Rhodin, Fig. 25.4). #83 EPIDERMIS - BASAL CELL Observe the abundance of tonofibrils (= keratin intermediate filaments) and ribosomes and the small number of mitochondria and absence of Golgi apparatus and granular endoplasmic reticulum. Epidermal cells do contain these organelles but in reduced amount. The bulk of synthesis is for structural proteins not exportable ones. What is the function of the numerous desmosomes? (IN3) The function of the tonofibrils? (No Rhodin counterpart) (alt. Fig. 25-7). #84 EPIDERMIS - SUPERFICIAL CELL LAYERS Note the keratohyalin granules in the cells of the stratum granulosum. The keratinization process is completed in the cell layers above the stratum granulosum, indicated by the disappearance of nuclei and cell organelles. Note that the cornified cells are of variable appearance (some "dark" and some "light") a reflection of processing rather than from a functional difference. Where would the contents of membrane coating granules be found? (Rhodin, Fig. 25-9). #85 MELANOCYTE These cells are located within the basal cell layer of the epidermis. Note absence of tonofibrils within the melanocyte. Find the premelanosomes. The melanosomes of the melanocyte are passed to the adjacent basal cells of the epidermis. (No Rhodin counterpart) (alt. Fig. 25-18). #86 SEBACEOUS GLAND The purpose of reviewing this micrograph is to make sure that you realize that sebum is composed of cell fragments and lipid (sebaceous) droplets, that are discharged by a process referred to as holocrine secretion. The accumulation of sebaceous (lipid) droplets in the cell is a gradual process, starting in the peripheral cells of the sebaceous alveolus. (No Rhodin counterpart) (alt. Figs. 2542, 25-43). #87 SWEAT GLANDS Note the difference in size between ordinary and odoriferous (apocrine) sweat glands. What is the function of the numerous myoepithelial cells? (IN4) (No Rhodin counterpart) (alt. Figs. 25-47, 25-48). Mammary Gland 88 MAMMARY GLAND (lactating) (Rhodin 34-68) Review the difference in releasing mechanisms between milk lipid droplets and milk protein particles. One occurs through exocytosis, the other through apocrine secretion. Make sure you know which mechanism relates to what product. DIGESTIVE SYSTEM 1: THE ORAL CAVITY AND SALIVARY GLANDS #94 ORAL EPITHELIUM (NON-KERATINIZED) The basal lamina (basement membrane) is not seen in this view, but the lower cells of this epithelium do represent basal cells. Note the change in cell shape as the cells move from basal to superficial layers. Nuclei are present in the surface cells. #95 TASTE BUD Note the difference in cell shape and cell aggregation of the taste bud and the oral epithelium. The nerve endings are sensory nerves. #99 LINGUAL GLAND (von Ebner's gland) (No Rhodin figure) The acinar lumen (serous) is always quite small and narrow, and is not always seen in electron micrographs. Find one here. The nuclei of serous secretory cells are usually round in contrast to those in mucous acini, which are often compressed and flattened against the base of the cell. Note the great abundance of secretory granules. The intralobular duct cells may, occasionally, also contain secretory granules. Find the myoepithelial cell of the duct wall. Try to follow the peripheral border of one serous acinus. The interacinar connective tissue is very thin and delicate. #98 SUBLINGUAL GLAND (No Rhodin figure) Note the difference in number between the mucous acini and the serous demilunes. Find the lumen of an acinus. Observe that the cells of the serous demilunes do not always border directly on the acinar lumen. If they do not border on this lumen, how does the secretory product reach the lumen? Note that the intercalcated ducts are small, narrow channels in comparison to interlobular and striated ducts (not seen in this micrograph). Although not marked on the micrograph, can you find blood capillaries in the connective tissue spaces? DIGESTIVE SYSTEM 2: PHARYNX, ESOPHAGUS AND STOMACH #115 STOMACH Note that there is only one cell type, a mucous cell, in the surface epithelium of the stomach. The gastric pits lead into the gastric glands proper, where there are several cell types present (see chart #116). As always, the lamina propria consists of loose connective tissue. There is a rich capillary network in the lamina propria. (Rhodin Fig. 28-11). #116 GASTRIC GLAND PROPER The section of this tubular gland is made in a plane parallel to the long axis of the gland, but para-centrally. As you already could see in the light microscope, the parietal cells are large and bulge out toward the lamina propria. Find the chief (zymogenic) cells. What is their secretory product(s)? (DG3) (Rhodin Fig. 2816). #117 GASTRIC GLAND PROPER - chief & parietal cells (detail) Note the abundant vesicles and tubules of the parietal cell which are involved in HCl production. Note the numerous giant mitochondria in the parietal cell as opposed to the small and sparse mitochondria in the chief cells. Study the intracellular secretory canaliculi of the parietal cell. Review the structure of the chief cell. It is essentially that of an exocrine gland cell - as seen in the salivary glands and the pancreas. The dashed lines are drawn to facilitate your finding the borderline between the two cell types. (Rhodin Fig. 28-17). DIGESTIVE SYSTEM 3: SMALL AND LARGE INTESTINE #118 SMALL INTESTINE - villus The villus is covered by a simple columnar epithelium. Note that cells are sloughed at the tip of the villus. Find the other two cell types present in this epithelium (goblet cell; endocrine cell). The small lymphocyte is transient, and is not a permanent component of the epithelium. Find the "striated border" and realize that you cannot resolve the individual microvilli at this magnification. Study the composition of the connective tissue core of the villus. (Rhodin Fig. 29-5) #119 SMALL INTESTINE - DEEP PORTION OF INTESTINAL WALL This chart is excellent for the study of the general architecture of the lamina propria, the muscularis mucosae, the submucosa, and the muscularis externa. (Rhodin Figs. 29-12 & 29-41). #120 INTESTINAL GLAND (CRYPT OF LIEBERKUHN) In this simple tubular gland, the Paneth cells are found near the end, whereas mucous cells and undifferentiated cells take up the major portion of the gland. Review the reasons for the high rate of cell mitosis in the upper part of the intestinal gland. (Rhodin Fig. 4-2). #121 LARGE INTESTINE Goblet cells are particularly numerous in the large intestine. If you look closely at the labeled goblet cell, you can see that the apex is packed with mucuscontaining secretory vesicles (the narrow base of this sell is out of the plane of section). Several crypts are seen in the section; the lumens don't stay in the plane of section all the way to the base of the crypts. DIGESTIVE SYSTEM 4: LIVER, GALL BLADDER and PANCREAS #122. PORTAL AREA, LIVER. In the center of the field observe the portal vein, hepatic artery and bile duct that make up the portal "triad", and note the connective tissue that surrounds them. In the liver tissue around the portal area you will see plates of hepatocytes, with sinuoids between them. Bile canaliculi can be seen as small white spots between hepatocytes. The sinusoids are lined by endothelial cells and occasional Kupffer cells. (Rhodin, Fig. 30-6). #123. LIVER SINUSOID In the Kupffer cell note occasional lysosomes, which are involved in the phagocytic activities of this cell type. The endothelial lining of the sinusoid is discontinuous, allowing free passage of materials into the space of Disse (note the numerous short microvilli extending from the surface of hepatocytes into this space). There is no organized basal lamina along the endothelial cells or hepatocytes. (Rhodin, Fig. 30-9). #124. CYTOPLASM OF LIVER CELLS. Most of the typical organelles are well developed in liver cells, reflecting the many functions of these cells. Note the nucleus, rough (granular) endoplasmic reticulum, smooth endoplasmic reticulum (not labeled here), mitochondria, Golgi complex, lysosomes, peroxisomes and occasional lipid droplets. The liver cell stores glycogen and lipid. The cytoplasm contains clusters of glycogen particles (black), which can be metabolized to glucose for release into the blood when needed by the body. The glycogen occurs primarily in areas rich in smooth endoplasmic reticulum. The diverse secretory and absorptive functions of the hepatocyte take place primarily across two surfaces, shown clearly here: (1) The cell surface facing the blood in the space of Disse and adjacent sinusoid. (2) The cell surface involved in the bile canaliculus. Note the junctional complexes that seal the two sides of the bile canaliculus, and keep the bile products isolated from the blood. (Rhodin, Fig. 30-10). #125 EXOCRINE PANCREAS (Rhodin Figure 30-23). In this low power electron micrograph, observe the organization of the acini, composed of acinar cells. Within the acinar cells you will see the basal rough endoplasmic reticulum, and the numerous secretory granules in the apical region of the cells, facing the small lumen of the acinus. Note the centroacinar cell in one of the acini. The intercalated duct shown here is of intermediate size. ENDOCRINE SYSTEM: PITUTARY GLAND #109. ANTERIOR PITUITARY, SURVEY VIEW. Here you see pituitary cells of various size clustered between capillaries. The main cell types are somatotropes (GH), mammotropes (prolactin), gonadotropes (FSH and LH), thyrotropes (TSH), and corticotropes (ACTH). You will not be required to identify these cell types in electron micrographs, but should note that the cells differ in size, shape, and in the number, size and distribution of their secretory granules (small black structures in the cytoplasm). When the content of a secretory granule is released from the cells, the hormones diffuse to nearby capillaries. The endothelium of capillaries is very thin, and in fact contains fenestrations (not seen clearly in this micrograph). #110. ANTERIOR PITUITARY CELLS. This electron micrograph shows two of the pituitary cell types in more detail. A gonadotrope occupies most of the upper left side of the figure, while another gonadotrope is at upper right. There is a somatotrope extending across the bottom of the figure, and cytoplasm of another somatotrope is at middle right. Hormones are synthesized on the rough endoplasmic reticulum (RER) of the two cell types. The RER in somatotropes (at right) has the usual appearance, while the gonadotrope RER is distended with recently-synthesized hormone. The hormone subsequently passes through the Golgi complex and is then formed into secretory granules. Since FSH and LH are glycoproteins, terminal sugars are added to the oligosaccharide chains as the hormone passes through the Golgi stack. When the cell is stimulated by the appropriate releasing hormone from the hypothalamus, the content of granules is released from the cell by exocytosis. (Rhodin, Fig. 20-8). #111. POSTERIOR PITUITARY, SURVEY VIEW. The nerve fibers (axons) that comprise the posterior lobe carry small secretory granules containing oxytocin and antidiuretic hormone (ADH, vasopressin), as well as their carrier proteins (neurophysins). The granules accumulate in nerve endings that can be seen in this figure (for example in the area below the capillary in the center; also note the process labeled "nerve ending"). When appropriate neural stimulation arrives from the hypothalamus, the content of granules in the endings is released and the hormones pass to nearby capillaries and then out to the body. Large accumulations of the granules, probably no longer functional, are called "Herring bodies". Most of the large nuclei seen here belong to pituicytes, the glial cells in this portion of the brain. Other nuclei belong to capillary endothelial cells and fibroblasts (Rhodin, Fig. 2016). ENDOCRINE SYSTEM (con’t.): THYROID AND PARATHYROID GLANDS #106 THYROID GLAND, SURVEY VIEW. The gland is made up of follicles, with epithelial cells forming their walls, and containing a lumen full of colloid. The follicles vary in size. Note the parafollicular cells, which secrete calcitonin. These cells can be distinguished at the EM level, although it is difficult to recognize them at the LM level. Also note the numerous capillaries closely apposed to the follicles, which is a characteristic of endocrine tissues. (Rhodin 21-2) #107 THYROID FOLLICULAR CELL. Remember that the follicular cells secrete thyroglobulin into the colloid, and subsequently resorb it and break it down to produce thyroid hormones. In this electron micrograph, try to identify the various organelles and cellular structures involved in these functions. (Rhodin 21-4) #108 PARATHYROID GLAND. The gland consists of cords of chief cells. Oxyphil cells contain very abundant mitochondria. (Rhodin 22-4) ENDOCRINE GLAND (con’t): ADRENAL GLAND #112 ADRENAL CORTEX. Notice the connective tissue capsule and the zona glomerulosa beneath the capsule. The boundary between the zona glomerulosa and zona fasciculata is not distinct even at the E.M. level. Notice the numerous large capillaries. Clear circles in the cytoplasm are lipid droplets. (Rhodin 23-3) #113 ZONA FASCICULATA OF ADRENAL CORTEX. Note the ultrastructure of these steroid-hormone secreting cells, source of glucocorticoids. The cells contain numerous lipid droplets. Notice also that the cells have numerous mitochondria with tubular cristae. Mitochondria with this structure are often found in steroid synthesizing cells. What other organelle, which is not seen well in this micrograph, is also abundant in cells that synthesize steroids? The cell borders on two capillaries, which have the fenestrated endothelium that is characteristic of capillaries in endocrine tissues. (Rhodin 235) #114 ADRENAL MEDULLA. Notice that the cells of the adrenal medulla, in contrast to the cells of the cortex as seen in micrograph 113, have smaller mitochondria and contain numerous, distinct secretory granules. Two types of cells are found, one secreting epinephrine (adrenalin), the other secreting norephinephrine (noradrenalin). Locate nerve endings in contact with the medullary cells. (Rhodin 23-12) MALE REPRODUCTIVE SYSTEM #131. SEMINIFEROUS TUBULE, RAT. In this electron micrograph, showing a seminiferous tubule and adjacent interstitial tissue, you can see in more detail the same structures you have been viewing with the light microscope in the previous slides. In the seminiferous tubule, the large, round nuclei belong to more mature primary spermatocytes. Toward the lumen from these are the nuclei of spermatids, which are all at the same phase of development, namely at an early phase in the shaping of the head. Remember, this is a rat seminiferous tubule--if it were human the germ cell population would appear much more heterogeneous, since the cycle of the seminiferous epithelium is not as clearly organized in human testes. Most of the smaller, oval or round nuclei at the base of the epithelium belong to young primary spermatocytes. Note the occasional Sertoli cell nuclei, and try to follow the extensive Sertoli cell cytoplasm as it passes up to enfold the spermatocytes and spermatids. In the interstitial tissue, observe the Leydig cells and capillaries (the latter are somewhat swollen because the testis was fixed for electron microscopy by perfusion of the fixative through the blood vessels). (Rhodin, Fig. 33-3). FEMALE REPRODUCTIVE SYSTEM 1: OVARY AND OVIDUCT Ovary #132 (Rhodin 34-3) Note the considerable difference in size between primordial follicles and the secondary follicle. What changes in the structure of the follicle increase its size? Note also the presence of several capillaries in the thecal layer, and the highly organized appearance of the follicle. Ovary #133 (Rhodin 34-6) In this low magnification view of a secondary follicle, examine the characteristics of the thecal layer, granulosa cells, corona radiata, and the ooplasm. Note particularly the basal lamina which separates the thecal and granulosa cell layers and the acellular zona pellucida that surrounds the oocyte. Ovary #134 (Rhodin 34-7) Higher magnification view of another secondary follicle. Note the penetration of the zona pellucida by processes from the oocyte and from the granulosa cells of the corona radiata. One current theory regarding follicular atresia suggests that contact of the ooplasm by granulosa cells is required for continued follicular development and, that if lost, atresia results. FEMALE REPRODUCTIVE SYSTEM 2. UTERUS, UTERINE CERVIX, AND VAGINA None FEMALE REPRODUCTIVE SYSTEM 3. PLACENTA PLACENTA--Terminal Villus #135 (Rhodin 34-58) Examine the ultrastructure of the syncytiotrophoblast cells, particularly their external surface. Note the paucity of cytotrophoblast cells at this stage of development. Be certain that you know the components of the placental barrier, how they may change during pregnancy and why.