Care of patient with MSK injury
advertisement
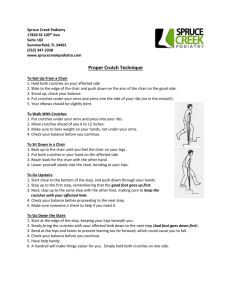
EMERGENCY DEPARTMENT PATIENT INFORMATION FOR YOUR CARE Care of the Patient with a Musculoskeletal Injury (Sprain, Strains, Casts, Splints, and Crutches) □ Sprains and Strains 1. A sprain is an injury that causes a stretch or tear in a ligament. Ligaments are strong bands of tissue that attach bones to each other. 2. A strain is an injury that causes a stretch or tear in a muscle or tendon. Tendons are strong bands of tissue that attach muscles to bones. 3. You may notice swelling, redness, and/or bruising. Sometime the bruising and/or swelling seems to spread down your arm or leg over the next few days – this is normal. The blood under the skin that causes the bruise is simply running “downhill”. 4. The general approach to treatment is R.I.C.E.: a. R – rest: at first you should avoid activities that cause pain. This may require the use of crutches or a sling b. I – ice: apply ice to the injured area for a maximum of 15 minutes out of every half-hour. You can continue icing this way for as long as the joint is swollen and sore c. C – compression: using a compression (e.g. Tensor) bandage can help reduce swelling and discomfort. It does not, however, give you extra support so you can do more activity. Compression bandages should only be tight enough to feel snug, and should not be worn when you are sitting or lying down. d. E – elevate: when you are sitting or lying down, elevate the injured part above the level of your heart. This helps reduce swelling and discomfort e. E – exercise: most sports specialists recommend early (after the first 24-48 hours) movement of the injured area to speed recovery. This should be done gently, within your limits of pain. At the beginning, this may be as simple as bending the injured part up and down. You may see a physiotherapist to help with early mobilization. 5. For additional pain relief, you may use ibuprofen (Advil, Motrin) or acetaminophen (Tylenol). Your doctor may give you stronger medicine if needed. 6. Returning to activity should be done in a graduated, step-by-step manner. For example, after a sprained ankle, you must be able to walk comfortably before you can run, and run comfortably before you can jump. 7. Return to the ED or call your primary care provider if the pain is worsening at any time, or if it has not improved after 7-10 days. Sometimes a small, hairline fracture can be present, but it can’t be seen on the first day. An x-ray may show it after it begins to heal. These instructions are not intended to be all-inclusive, and may not cover all possibilities. If a new problem develops, or if you have any further concerns or questions please contact your primary care provider, Telehealth Ontario at (866) 797-0000, or return to the ER. Royal Victoria Hospital of Barrie, 201 Georgian Drive, Barrie, Ontario L4M 6M2 (705) 728-9802 www.rvh.on.ca RVH-3295 (Rev Nov 28, 2006) EMERGENCY DEPARTMENT PATIENT INFORMATION FOR YOUR CARE □ Casts and Splints 1. You should keep the affected limb elevated above the level of your heart as much as possible for the next 48 hours. This will reduce swelling in the injury, which will make it feel better, and lessen the chances that your cast or splint will get too tight. 2. Do not get your splint or cast wet. After it has hardened, plaster is ruined by water. Even if your cast is made of fiberglass, getting it wet will soak the padding and cause it to rot. This generally means that you will be unable to shower with a cast on. 3. For pain relief, you may use ibuprofen (Advil, Motrin). If you can’t take ibuprofen, or need additional pain relief, you may use acetaminophen (Tylenol). Your doctor may give you stronger medicine if needed. 4. Return the ED at any time if you develop any of the following: a. increasing or severe pain, despite taking your pain medication b. numbness or loss of feeling in the affected limb c. severe swelling of the immobilized limb d. noticeable change in temperature at the ends (e.g. fingers, toes) of the immobilized limb e. your cast or splint breaks. 5. Never put anything inside the cast for any reason (e.g. to scratch an itch). If an object does get lost inside the cast, come to the ED to get it removed. □ Crutches 1. The nurse that gives you your crutches should show you how to use them properly. Here are some additional pointers and reminders: a. The crutches should rest against the side of your body, not in your armpits. Your weight should be held on your hands. b. You should not crutch-walk on stairs. Hold the crutches in one hand and the handrail with the other. Step down with the bad leg and crutches first, then the good leg. When climbing stairs, step up with the good leg, and then the bad leg and crutches. “Up with the good – down with the bad.” c. Be very careful outside, especially on wet, snowy, or icy ground. d. If the crutches are rubbing against your hands or your side, you may use hand lotion or put extra padding on the crutch. These instructions are not intended to be all-inclusive, and may not cover all possibilities. If a new problem develops, or if you have any further concerns or questions please contact your primary care provider, Telehealth Ontario at (866) 797-0000, or return to the ER. Royal Victoria Hospital of Barrie, 201 Georgian Drive, Barrie, Ontario L4M 6M2 (705) 728-9802 www.rvh.on.ca RVH-3295 (Rev Nov 28, 2006)