Drugs used
advertisement

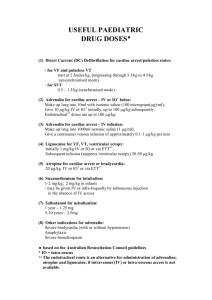
DRUGS USED IN EMERGENCIES The higher coronary blood flow increases the frequency of the VF waveform and should im- DRUGS USED IN CARDIAC ARREST prove the chance of restoring a circulation Drugs delivery in the treatment when defibrillation is attempted of cardiac arrest Peripheral venous drug delivery. Drugs injected peripherally must be followed by Bronchodilation Increases myocardial contractility The alpha-adrenergic actions of adrenaline a flush of at least 20 ml of fluid and elevation of cause vasoconstriction, which increases myo- the extremity for 10—20 s to facilitate drug deliv- cardial and cerebral perfusion pressure. ery to the central circulation. Tracheal route. Is not further recommended Intraosseous route. Amiodarone If VF/VT persists after three shocks, give 300 mg amiodarone by bolus injection. If intravenous access is difficult or impossible. A further dose of 150 mg may be given for recur- Although normally considered as an alternative rent or refractory VF/VT, followed by an infusion route for vascular access in children, it can also be of 900 mg over24. effective in adults. Membrane-stabilising anti-arrhythmic drug Intraosseous injection of drugs achieves adequate increases the duration of the action potential plasma concentrations in a time comparable with and refractory period in atrial and ventricular my- injection through a central venous catheter. ocardium. Atrioventricular conduction is slowed, and a simi- Shockable rhythms lar effect is seen with accessory pathways. Ventricular fibrillation/pulseless ventricular tach- Amiodarone has a mild negative inotropic action ycardia) and causes peripheral vasodilation through non- adrenaline is the first drug used in cardiac ar- competitive alpha-blocking effects. rest 1 mg is given the first time after 3 first electrical shocks and than 1 mg every 3—5 min of CPR (every second loop of CPR) Lidocaine 1mg/kg - may be used as an alternative if amiodarone is not available. Do not give lidocaine if amiodarone has been given already Epinephrine Lidocaine is indicated in refractory Alfa, beta-mimetic VF/VT The alpha-adrenergic actions of adrenaline cause vasoconstriction, which increases myocardial and cerebral perfusion pressure. 1 Non-shockable rhythms (PEA and asystole) hospital cardiac arrests) or after return of sponta- Severe bradyarrhythmias, asystole neous circulation is not recommended. Pulseless Electrical Activity (PEA) Give sodium bicarbonate (50 mmol) if cardiac absence of a palpable pulse or other signs arrest is associated with hyperkalaemia or tricyclic of circulation despite the presence on the antidepressant overdose; ECG monitor of recognisable complexes repeat the dose according to the clinical condition which normally produce a pulse. and result of repeated blood gas analysis. mechanical myocardial contractions are to Bicarbonate causes generation of carbon weak to produce a detectable pulse or dioxide, which diffuses rapidly into cells. blood pressure. This has the following effects. • It exacerbates intracellular acidosis. Management: • It produces a negative inotropic effect on causes elimination ischaemic myocardium. start CPR 30:2 and give adrenaline 1mg as soon as • It presents a large, osmotically active, sodium intravascular access is achieved load to an already compromised circulation and Atropine is not further recomennded for therapy brain. of non-shockable rythms in cardiac arrest • It produces a shift to the left in the oxygen dissociation In cardiac arrest – if possible – curve, further inhibiting release of oxygen ventilation with 100% concentrated oxygen to the tissues. Other drugs Calcium salts- only when indicated specifically, Magnesium (8mmol=4ml 50% magnesium sul- i.e. in pulseless electrical activity phate or 2 g) - initial intravenous dose of 2 g pe- caused by ripherally over 1—2 min; it may be repeated after • hyperkalaemia 10—15 min. • hypocalcaemia for refractory VF/VT if there is any suspi- • overdose of calcium channel-blocking drugs cion of hypomagnesaemia (e.g., patients The initial dose of 10 ml 10% calcium chloride on potassium-losing diuretics) (6.8 mmol Ca2+) may be repeated if necessary. torsades de pointes digoxin toxicity HYPERVENTILATION Treatment of the underlying cause Bicarbonates Low concentration of CO2 can be beneficial Administering sodium bicarbonate routinely dur- For patients with psychogenic hyperventila- ing cardiac arrest and CPR (especially in out-of- tion careful explanation of the basis of their 2 symptoms can be reassuring and is often sufficient Others have benefited from beta-blockers or anxiolytics hydrocortisone 100-500 mg i.v. or prednisolone 50-100 mg i.v. or methyloprednisolone 1,0-2,0 mg i.v. Inhibit anaphylactic/inflammatory reaction Inhibit phospholipase A2 (PG, TXA, PI), ANAPHYLACTIC SHOCK stablize membranes-inhibit release of his- Oxygen tamine and its congeniers, decrease mem- Horizontal position branes permeability, decrease leukocytes Cuff on the arm migration and antibodies production, in- Fluids – 0.9% saline or 5% glucose i.v. creases sensitivity of adrenergic receptors to epinephrine Epinephrine 0.5-1.0 mg given s.c. or i.m. (rarely i.v.) Increases blood pressure – constricts small blood vessels in the skin and mucosa and renal arteries Stimulates beta1 –receptors: causes increased cardiac output (ino- and chronotropic positive effects) Antihistaminics Clemastine 2 mg i.v. or antazoline 100 mg i.v. Block histamine receptors H1 in tissues and protect them against histamine released in anaphylactic reaction Ranitidine 50 mg i.v. Relaxes bronchi and decreases edema in mucosa ASTHMA Increases blood flow in the liver, skeletal muscles, coronary arteries Beta2-mimetics – inhalation/nebulization Decreases blood volume Prednisone – 10-20 mg orally Increases oxygen demand Oxygen Is arrhytmogenic Hydrocortisone – 500 mg, followed by infusion 200-400 mg in 500 ml of glucose Beta2-mimetics Dilate bronchi Ipratropium Theophyline - 5 mg/kg in slow injection Albuterol or fenoterol i.v. within 10-15 min, followed with infu- In mild to moderate bronchospasm in inha- sion of 0,5-0,6 mg/kg/h. lation/nebulization – albuterol 2,5 – 5 mg In severe bronchospasm – albuterol 0.5 mg s.c HYPERTENSIVE EMERGENCY Drugs given s.l. or orally Captopril 12.5-25 mg s.l. Glucocorticosteroids Nifendypine – 10 mg s.l. 3 Nitroglycerine/isosorbide dinitrate – 0.5 mg s.l./10 mg s.l. Clonidine 0.2 orally Prazosine 1 mg orally Drugs given parenterally Labetalol PULMONARY EDEMA Nitroglycerine 0.5 mg s.l. repeated every 10 min Furosemide 40-60 mg i.v. Morphine 5 mg i.v. Nitroglycerine 0.5-1 mg/h in infusion Diazoxide Furosemide EPILEPTIC SEIZURES Nitroprusside sodium Diazepam 10 mg i.v. Phentolamine Barbiturates: phenobarbithal, thopental Hydralazine Phenytoin Trimetaphan ANGINAL PAIN/MI Nitroglycerine 0.5 mg s.l. repeated 3 times (every 15 min) under blood pressure and heart rate control Morphine 5 mg i.v. ASA 150 mg (300 mg) or ticlopidine 250 mg Oxygen 4