to a copy of this information in Microsoft Word format
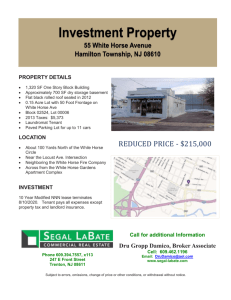
advertisement

LONG GREEN ANIMAL DERMATOLOGY CENTER Dr. Joseph A. Bernstein, DVM, DACVD ALLERGY TREATMENT IN HORSES As with humans and small companion animals, there has been increasing awareness of allergic diseases in the horse. As with other species, equines may suffer from one or more allergic diseases such as insect hypersensitivity, atopy, food allergy and contact allergy. In the diagnosis and treatment of these allergies in horses, the veterinary dermatologist keeps in mind the “summation of effect”. In other words, more than one condition may have an additive effect resulting in the clinical signs of the horse. Therefore, as in the small animal patient, the diagnostic and therapeutic protocol must proceed in an orderly step-by-step fashion in which the patient’s environmental and predisposing influences are examined in conjunction with treatment of secondary perpetuating factors like bacterial and yeast infections. Typically we recommend ruling out or treatment of secondary infections or parasitic disease prior to proceeding with allergy testing. As in the small animal patient, THERE IS NO CURE FOR ALLERGIES. The goal is control of the horse’s symptoms to provide a good quality of life often through multiple forms of therapy. The following are components of a safe program for the treatment of allergies in the equine patient: Environmental Control Avoidance or reduction of exposure to offending allergens is the ideal treatment for allergy. In practical application, however, this may be problematic. We typically attempt to identify and control these environmental influences in conjunction with systemic and topical therapies. 1. Environmental insect control: Examples of typical recommendations include the following: Moving the horse away from standing water, compost, manure piles and cattle; Using fly sheets and masks sprayed with permethrin as a repellent; Stabling during the dusk and dawn hours when gnats are typically at their worst; Employing box fans within stalls, time-released insect sprays, and 32 x 32 per 2.5 cm meshing. 2. Minimizing dust exposure in barns: This may involve the installation of rubber mats and/or bedding that generates less dust. Switching to wet-down hay, pelleted rations, or grass silage may also be of benefit. 3. Moving the horse from the environment entirely: This may be impossible for the owner but can be the ideal avoidance therapy if practical for the individual patient. This move could involve restriction of activity depending on the cause identified by the dermatologist. For example; if mold or dust are identified by allergy skin testing as offending allergens, the patient may be moved out into pasture. If symptoms are related to pollen allergens in summer pasture, stabling during peak pollen times may be recommended. For some horses, movement to a different barn or farm may be recommended. 4. Miscellaneous: Miscellaneous allergens that may be easily overlooked include: topical medications (ointments, sprays and powders), vitamin supplements and dewormers, and laundry detergents used in cleaning blankets and saddle pads. DIETARY TRIALS Food allergy or hypersensitivity is a disease of the horse associated with the ingestion of one or more substances in the horse’s diet. For the dermatologist, differentiating a food intolerance (non-allergic) from true food allergy is difficult. At the current time the only means of definitively diagnosing food allergy in the horse (as in the small animal patient) is through elimination diets and provocative testing. This usually involves a 4-6 week trial ideally consisting of food sources novel to the individual patient and elimination all unnecessary vitamins, supplements or drugs. A bulk food not previously used is then fed for the duration of the trial (i.e. timothy, alfalfa, rolled oats or barley). If grain must be fed, a switch from sweet feed to a pure grain like oats or corn. Confirmation of the diagnosis is made by rechallenging with individual elements of the ration every 7 days and monitoring for return of symptoms. Strict and accurate dietary trial are more difficult to perform in the horse than in dogs and cats. TOPICAL THERAPIES 1. Fly control: Fly control is a mandatory part of a treatment regimen for the allergic horse. Recommended repellents include: Flypel® from Virbac- this spray contains a permethrin, sunscreen and silicon Avon Skin-So-Soft® bath oil diluted 50:50 with water Avon Skin-So-Soft Big Guard Plus IR3535® lotion with sunscreen Products with DEET (N,N-diethyl-m-toluamide) solution at approximately a 15% concentration 2. Shampoo therapy: The selection of both medicated and non-medicated shampoos are made based on the individual symptoms of the allergic horse. Cool water should always be used for the itchy patient. For itchy horses, shampoos containing oatmeal with or without the topical anesthetic pramoxine may be valuable. Shampoos containing steroids can also be valuable. Antiseborrheic shampoos are recommended for horses with excessive scale, and antimicrobial shampoos for those with secondary infections. 3. Leave-on Topical Therapies: These are topical products which are not rinsed off. They include dips, sprays, ointments and leave-on conditioners. Products are chosen based on the individual patient needs, antiparasitic, anti-itch, antiseborrheic or antimicrobial. SYSTEMIC THERAPY 1. Corticosteroids: Steroids have long been the mainstay of treatment of allergic disease in both companion animals and equines. They work by broad suppression and prevention of inflammatory chemical products and by-products involved in allergic responses. Though generally well tolerated in the horse, rarely seen adverse side-effects may be a consequence of repeated, chronic or aggressive use of steroids in the horse as in the small animal. These include behavioral changes, increased susceptibility to infection and poor wound healing. Laminitis and hyperadrenocorticism caused by steroid use have been poorly documented but have been mentioned anecdotally. The two most commonly used systemic steroids in the equine patient for short-term allergy treatment are: prednisolone tablets or compounded syrup and dexamethasone tablets or injectable. 2. Antihistamines: Antihistamines are often prescribed for the allergic horse as a safer alternative to steroids for longer term control of symptoms. The most common antihistamine we choose is hydroxyzine, but other options include doxepin, amitriptyline, chlorpheniramine, and diphenhydramine. As with the small animal allergy patients, there is great variation in response to different anthistamines, so it is sometimes necessary for different antihistamines to be tried for an individual patient. Despite having less sideeffects than corticosteroids, some side-effects may be noted, the most common of which include light sedation and personality changes. 3. Allergen Specific Immunotherapy (ASIT): We employ intradermal skin testing for offending allergens in the atopic horse. These allergens include pollens from weeds, trees, and grasses as well as insects, mites, molds and danders. Positive reactions to the injections indicate the presence of skin-sensitizing antibody, a type of inflammatory cell known as mast cells that degranulate on exposure, and tissue that responds to the released inflammatory mediators. Positive skin test reactions viewed in conjunction with the clinical history and environmental exposure of the horse are used to formulate allergenspecific immunotherapy (ASIT) “vaccines”, which are used to hyposensitize the horse. ASIT has been used for the control of urticaria (hives) and dermatitis secondary to atopy, insect hypersensitivities,and allergen-induced recurrent airway obstruction. Although in some cases, improvement may be seen as early as 2 months into immunotherapy, a minimum of 12 months is necessary to determine the efficacy in any given equine patient. Injections are given subcutaneously.