Correction of Optical Aberration in KC
advertisement
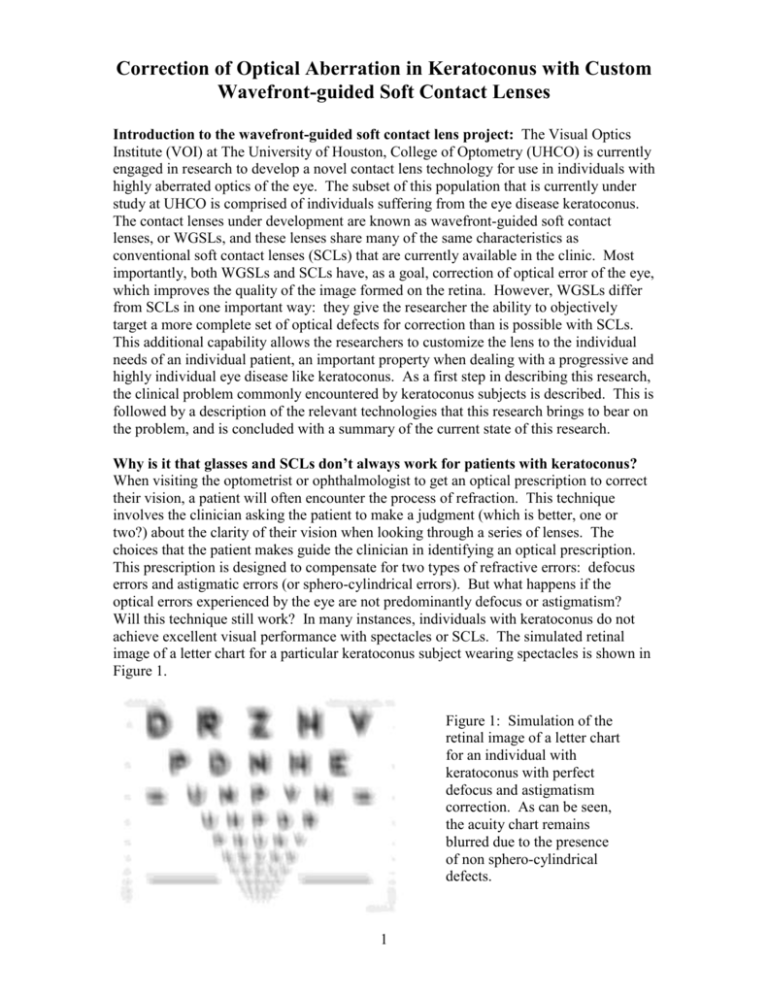
Correction of Optical Aberration in Keratoconus with Custom Wavefront-guided Soft Contact Lenses Introduction to the wavefront-guided soft contact lens project: The Visual Optics Institute (VOI) at The University of Houston, College of Optometry (UHCO) is currently engaged in research to develop a novel contact lens technology for use in individuals with highly aberrated optics of the eye. The subset of this population that is currently under study at UHCO is comprised of individuals suffering from the eye disease keratoconus. The contact lenses under development are known as wavefront-guided soft contact lenses, or WGSLs, and these lenses share many of the same characteristics as conventional soft contact lenses (SCLs) that are currently available in the clinic. Most importantly, both WGSLs and SCLs have, as a goal, correction of optical error of the eye, which improves the quality of the image formed on the retina. However, WGSLs differ from SCLs in one important way: they give the researcher the ability to objectively target a more complete set of optical defects for correction than is possible with SCLs. This additional capability allows the researchers to customize the lens to the individual needs of an individual patient, an important property when dealing with a progressive and highly individual eye disease like keratoconus. As a first step in describing this research, the clinical problem commonly encountered by keratoconus subjects is described. This is followed by a description of the relevant technologies that this research brings to bear on the problem, and is concluded with a summary of the current state of this research. Why is it that glasses and SCLs don’t always work for patients with keratoconus? When visiting the optometrist or ophthalmologist to get an optical prescription to correct their vision, a patient will often encounter the process of refraction. This technique involves the clinician asking the patient to make a judgment (which is better, one or two?) about the clarity of their vision when looking through a series of lenses. The choices that the patient makes guide the clinician in identifying an optical prescription. This prescription is designed to compensate for two types of refractive errors: defocus errors and astigmatic errors (or sphero-cylindrical errors). But what happens if the optical errors experienced by the eye are not predominantly defocus or astigmatism? Will this technique still work? In many instances, individuals with keratoconus do not achieve excellent visual performance with spectacles or SCLs. The simulated retinal image of a letter chart for a particular keratoconus subject wearing spectacles is shown in Figure 1. Figure 1: Simulation of the retinal image of a letter chart for an individual with keratoconus with perfect defocus and astigmatism correction. As can be seen, the acuity chart remains blurred due to the presence of non sphero-cylindrical defects. 1 This deficit in image quality and resulting visual performance occurs because the changes in corneal shape that accompany keratoconus induce refractive errors (or aberrations) which traditional spectacles and SCLs are simply not designed to correct. In other words, keratoconus induces optical errors in addition to defocus and astigmatism. So, even when defocus and astigmatism in the keratoconic eye are well corrected, these “other aberrations” remain uncorrected and can lead to blurred vision. What are these “other aberrations”: In order to quantitatively understand these other aberrations, it is important to adopt a language to discuss them. The use of the Zernike polynomial has become increasingly common in the ophthalmic community and has been adopted as a standard for describing ocular aberration (ANSI Z80.28). Its utility can be seen in the fact that the Zernike polynomial can describe not only defocus and astigmatism, but these “other aberrations” as well. For the purposes of this discussion, it is sufficient to know a few key concepts related to the Zernike polynomial. As seen in Figure 2 the Zernike polynomial is often used to define aberration over the pupil. Figure 2: The Zernike polynomial is commonly used to describe aberration over the pupil (dark hole) of the eye. In this figure, the pupil of the eye is identified by a yellow circle inside the iris (colored part) of the eye. The fact that the pupil is round gives wavefront aberration maps their characteristic round shape. These aberration terms can be coarsely grouped into lower order aberrations and higher order aberrations. Lower order aberrations include the defocus and astigmatism errors while the “other aberrations” described above are classified as higher order aberrations. Quantifying ocular aberrations with the Zernike polynomial allows one to talk about a single aberration (defocus for example) a subset of aberrations (lower order aberrations, higher order aberrations, etc) a large set of aberrations (66 Zernike terms are often measured for a given eye) or aberrations for different pupil sizes (data describing 5mm and 6mm pupils are commonly reported). Figure 3 is an example of how the Zernike polynomial is used to report optical error. Here the first 15 Zernike terms for a measurement of an individual with keratoconus are presented. 2 Figure 3: A table reporting a subset of the Zernike terms measured on an eye with keratoconus. Here, the field “N” is a unique identifier for the individual Zernike terms being reported. Term 4 reports the low order aberration of defocus. Terms 614 report a subset of the higher order aberration terms. The field “Coeff (microns)” reports the amount of that particular aberration term that is present in the eye using the units of microns. How are higher order aberrations quantified clinically? The development of WGSLs is, to a large degree, possible due to a relatively new clinical technology that allows for the quick, objective quantification of the optical defects of the eye. This technology is known as wavefront sensing. Wavefront sensing is currently used in a therapeutic manner with state-of-the-art refractive surgery platforms. However, the wavefront sensor is finding expanded clinical relevance as a diagnostic instrument in evaluating eyes that suffer from elevated levels of optical distortion, such as keratoconus. Figure 4 shows a wavefront sensor in the clinical environment. There are a variety of types of wavefront sensors, with one common type being the Shack-Hartmann wavefront sensor (SHWS). The wavefront sensor objectively collects information on the optical performance of the eye that can be used to calculate the amount of individual Zernike terms that are present (Figure 3). The aberration data can also be displayed in a graphical format (Figure 5 below). Figure 4: A Shack Hartmann Wavefront Sensor in a clinical setting. A wavefront sensor is capable of quickly and objectively quantifying the optical properties of an eye. To record data with this instrument, the patient places their head in the forehead and chin rest (A). The instrument operator aligns the eye under study to the measurement head (B). After acquiring an image, the data is processed, stored on a computer (C) and displayed on the screen (D). 3 What kinds of aberrations are present in keratoconus? All eyes, including normal eyes, have some level of both lower and higher order aberration. And every eye will have a unique quantity of these individual lower and higher order aberrations. Depending on the severity of the disease, eyes with keratoconus may be accompanied by elevated levels of both lower and higher order aberration. The aberration data shown in Figure 3 can be mathematically combined and graphically represented as shown in Figure 5 below. Figure 5 shows two color-coded maps that describe the higher order aberration measured in a normal eye (Figure 5A) and a keratoconic eye (Figure 5B). A majority of the map in Figure 5A is green, representing a relatively flat wavefront. However, the map in Figure 5B displays a much larger variation in color. This variation signifies the presence of higher order aberration in this individual keratoconic eye in a greater quantity than the normal eye shown in Figure 5B. The circular nature of the map denotes the boundary of the measurement, which is defined by the pupil of the eye. The goal of a WGSL is to correct these optical aberrations. Figure 5: A wavefront aberration map of the “other aberrations” or higher order aberrations of two individual eyes. Figure 5A reports data for a normal eye and Figure 5B reports data for a keratoconic eye. The keratoconic eye exhibits elevated levels of higher order aberration (seen as increased levels of red and blue in the map) as compared to the normal eye in Figure 5A. Note that the circular nature of the map denotes the boundary of the measurement, which is defined by the pupil of the eye. How is this wavefront data used to design a wavefront-guided soft contact lens? The coefficients of the Zernike polynomial, which are derived from measurement data collected by the wavefront sensor, can be used to derive an optical prescription (or a correction) for an eye. However, unlike the prescription provided by the process of refraction described above, the Zernike prescription is more complete, providing both lower order and higher order aberration data. In the case of keratoconus, the ability to measure higher order aberrationsallows the wavefront sensor to quantify a more accurate and complete representation of the optical performance of the eye. This gives the researcher and contact lens designer a more complete description of the optical properties of the eye. It is precisely this data that is needed to define an optimal correction for keratoconus, and it is this data that is used in development of WGSLs. 4 Figure 6a shows a simplified cartoon of a wavefront exiting the eye as it would during wavefront sensor measurement. Light scatters from a point source at the retina (red dot) and travels back through and out of the eye. If the eye were optically perfect, the tips of the light rays (arrows) would form a straight line, as is shown by the green line. However, aberration in the eye leads to distortion in the wavefront, as seen by the red and blue lines. In this figure, the red portion of the wavefront is in front of, or leading, the blue portion. The goal of the WGSL is to get all portions of the wavefront lined up, so that no portion is leading or lagging behind. This is shown in Figure 6b. A threedimensional representation of wavefront maps in this process, defined over the pupil of the eye, are shown in Figure 7 below. wavefront error negated by WGSL wavefront error measured by a wavefront sensor direction of light propagation direction of light propagation A Figure 6: Simple schematic demonstrating the concept of a WGSL. This cartoon shows a picture of how the wavefront sensor would quantify aberration in the eye. Light scatters from a point source at the retina (red dot) and travels back through and out of the eye. The WGSL is designed to account for both the lower order aberrations and higher order aberrations of the eye. Here Figure 6A shows an uncorrected keratoconic eye suffering from ocular aberration. The red portion of the wavefront is in front of, or leading, the blue portion. Figure 6B shows the correction of that eye with a WGSL. Unlike conventional SCLs, this WGSL is designed to correct both the lower and higher order aberration present in this eye. 5 B Figure 7: The concept of a WGSL is shown. Figure 7A shows the wavefront error of the keratoconic eye. Figure 7B shows the compensating wavefront that is incorporated into the WGSL forming a unique correction for the aberration structure in Figure 7A. Note that where the ocular wavefront is red, the correcting wavefront is blue and vice versa. Figure 7A was captured in a real eye and Figure 7B is a measurement of an actual WGSL. Figure 7C shows the resulting on-eye performance of the lens, which has reduced the higher order aberration experienced by the eye. What is the process involved in designing a WGSL? The process for the design of a WGSL is shown in Figure 8. It differs from a typical contact lens dispensation algorithm in that the result is a contact lens tailored to the unique needs of an individual patient, a WGSL. The algorithm also allows investigators at the VOI to define and ask research questions regarding WGSLs. 1. Subject identification 2. Clinical examination/ev aluation of subject 10. Exit criterion achieved 9. Optically profile contact lens n 3. Develop correction strategy y 8. On-eye evaluation of contact lens 11. Report results 4. Generate contact lens design y 7. stability satisfactory n 6. Sterilize/ evaluate bulk contact lens 5. Manufacture contact lens 6 Figure 8: Generalized form of the algorithm used to design, manufacture and evaluate WGSL at the Visual Optics Institute, University of Houston, College of Optometry. This algorithm supports the active study of WGSL design for keratoconus subjects. Summing up: Wavefront sensing is an exciting technology allowing clinicians and researchers to better understand the optical performance of the eye. Unlike refraction, wavefront sensing allows the measurement of a full range of refractive errors, not simply defocus and astigmatism. This becomes important in ocular conditions where higher order aberrations play a visually significant role. The language of wavefront aberration affords a way to describe both lower and higher order aberrations. While wavefront sensors are not universally available in the clinical setting, their numbers are increasing and will continue to increase as clinicians and scientists find more utility for the information they produce. Such utility may come in the form of assistance in disease detection, tracking disease progression, assistance in evaluating a conventional contact lens correction, gaining better understanding about a patient’s vision and customization of an optical correction to a patient’s individual needs. The description above focused on this last application, which is an area of active research at the VOI. To date, researchers are capable of designing, manufacturing and evaluating these lenses in the clinical setting. However, challenges exist that currently limit their effectiveness. First, these lenses are very sensitive to movement, and significant movements reduce visual performance. In some instances of extreme movement, optical performance falls to levels where the correction actually INDUCES new aberrations instead of correcting aberrations. In this case, the correction is useless. Another challenge exists in the highly custom nature of the lens. Each lens is uniquely manufactured for a particular eye, making the process time consuming and expensive. Methods are currently under investigation at The VOI to reduce the complexity of the design and manufacture process and to make these lenses more successful more of the time. This latter work is seen as a method to make the lenses more clinically relevant. These lenses currently remain in the research domain and are not available for dispensation. The VOI and other research groups believe they do hold future promise for providing the clinician with an additional method to treat the optical defects of the highly aberrated eye. Please direct questions regarding this work to: Jason D. Marsack Research Assistant Professor 505 J Davis Armistead Bldg. University of Houston, College of Optometry Houston TX 77204 P: 713 743 0661 F: 713 743 2053 jmarsack@optometry.uh.edu 7