New General Surgery Patient Intake Forms
advertisement

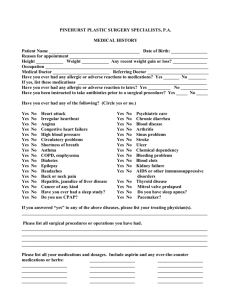
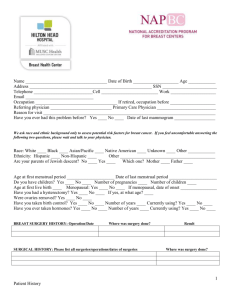
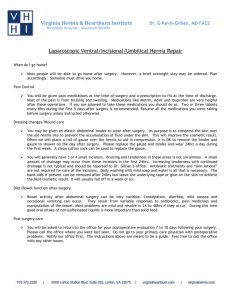
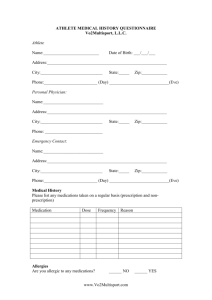
BMI of Texas 9910 Huebner Rd, Suite 250 San Antonio TX 78240 (210)615-8500 Phone (210)615-8501 Fax New General Surgery Patient Intake Questionnaire In order to minimize your wait time and maximize your experience at BMI of Texas, please take a moment to complete this questionnaire. We realize this is a lengthy form but assure you it is all important information and will be kept confidential. Please Print First Name: ________________________Last Name: _______________________DOB:_________________ Preferred Surgeon (circle one): Michael Seger, MD Terive Duperier, MD Richard Englehardt, MD What are you here for today? _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ ________________________________________________________________________________ Who referred you to our practice? _____________________________________________________ Please list all Doctor’s you follow up with: _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ _________________________________________________________________________________ CONTINUE TO NEXT PAGE For office use only: Appointment date: ___________________________ Time: ________________ Medications: Please list below any and all medications/vitamins you are currently taking. Example: Lipitor 10mg one tablet daily at bedtime 1.____________________________________________________ 2.____________________________________________________ 3.____________________________________________________ 4.____________________________________________________ 5.____________________________________________________ 6.____________________________________________________ 7.____________________________________________________ 8.____________________________________________________ 9.____________________________________________________ 10. ___________________________________________________ Not currently taking any medications Allergies: Do you have allergies to any of the following: Medications, if so, please list medication and reaction: __________________ _______________________________________________________________ _______________________________________________________________ Latex Iodine, when: ____________________________________________________ IV Contrast, when: ________________________________________________ Adhesives, type: _________________________________________________ No Known Allergies Medical History Please carefully review the list of medical conditions/problems listed below and check any that apply to you: Angina Glucose Intolerance Allergic Rhinitis Gout Anxiety Heartburn/Indigestion Asthma Hemorrhoids Breast Cancer High Cholesterol Heart Disease w/bypass surgery Hypertension (high blood pressure) Heart Disease without bypass surgery High triglycerides Cardiomyopathy Hypothyroidism (Underactive thyroid) Carpal Tunnel Syndrome Infertility Chest pain with exertion/exercise Insomnia Gallstones Intermittent Claudication Chronic Back Pain Intertriginous Dermatitis (irritation of the skin folds) Congestive Heart Failure Irritable Bowel Syndrome Stroke Joint Pain DVT (Blood Clot) Menstrual Irregularity Degenerative Disk Disease Migraine Headaches Depression Myocardial Infarction (Heart Attack) Type I Diabetes/Insulin Dep (controlled) Swelling of the legs (edema) Type I Diabetes/Insulin Dep (Uncontrolled) Peripheral Vascular Disease Type II Diabetes/Adult Onset (Controlled) Stomach Ulcers Type II Diabetes/Adult Onset (Uncontrolled) Polycystic Ovarian Syndrome (PCOS) Abnormal Uterine Bleeding Pseudotumor Cerebrii Dysmenorrhea (Excessively painful menses) Pulmonary Embolus (blood clot to lungs) Shortness of breath with exertion/exercise Seasonal Allergies Abnormally elevated liver function tests Sleep Apnea Fatigue Sleeping Disorder Fatty liver (due to alcohol) Stress Urinary Incontinence (leaking urine with Fatty liver (NOT related to alcohol) cough/straining) Fibrocystic breast disease Thrombophlebitis Fibromyalgia Urinary Urge Incontinence (can’t hold urine) Acid Reflux Disease/GERD Varicose Veins Gestational Diabetes (diab w/pregnancy) Venous Insufficiency *Note to patient: We apologize for the length of this form but we feel that all of this information is very important to enable our office and staff to provide you with excellent care. Surgical History: Please list non-bariatric surgeries (surgeries not related to weight loss) you have had or indicate if No prior non-bariatric surgeries you have not had any. Example: Open Hysterectomy w/ ovaries removed, 1/25/99, no complications Procedure/Surgery: Date: **specify laparoscopic or Open Complications: Please list previous bariatric (weight loss) surgeries: No prior bariatric surgeries Procedure/Surgery: (laparoscopic/Open) Date: Original Weight: Lowest Weight Complications: Family History: (Please include only parents, grandparents, and siblings) Illness/Medical Condition Family Member _________________________________ __________________________________ _________________________________ __________________________________ _________________________________ __________________________________ _________________________________ __________________________________ _________________________________ __________________________________ _________________________________ __________________________________ _________________________________ __________________________________ Social History: Do you currently smoke? Yes No If yes, how many years have you been smoking? ___________ Packs per day? _______________ For past smokers, what year did you quit? ____________How many years did you smoke? _______ Do you drink alcohol? Yes No If yes, how many times/week or month? __________________________ Do you use illicit/street drugs? Yes No If yes, what type did/do you use and how often? _________________________________________ Review of Systems General: Please check any/all that apply to you: Functional Status: Check any/all that apply to you: No impairment Able to walk 200 ft with assist device (cane/crutch) Cannot walk 200 ft with assist device (cane/crutch) Requires wheelchair Bedridden Pseudotumor Cerebri: Check any/all that apply to you: No Symptoms Headaches with dizziness, nausea, and/or pain behind eyes Headaches with visual symptoms, and/or controlled with diuretics MPI confirmed diagnosis of PTC Well controlled with stronger medications Requires narcotics, surgical intervention done or recommended Abdominal Hernia: Check any/all that apply to you: No hernia Asymptomatic hernia, no prior operation Successful repair Recurrent hernia or size >15cm Chronic evisceration through large hernia or multiple failed repairs Stress Urinary Incontinence: Check any/all that apply to you: No Symptoms Minimal and intermittent Frequent but not severe Daily occurrence, requires sanitary pad Disabling Failed surgery General (Continued): Abdominal Skin / Pannus No Symptoms Intertriginous irritation Pannus is large enough to interfere with ambulation Recurrent cellulitis or ulceration Surgical treatment \ Skin Please check any/all that apply to you: Rash under folds /breasts Keloids/large scars Poor Wound Healing Blood: Please check any/all that apply to you: Anemia (Iron deficiency) Anemia (B12 deficiency) HIV / AIDS Low Platelets Swollen Lymph Nodes Superficial clot in leg Endocrine / Metabolic Gout: Check any/all that apply to you: No gout present Hyperuricemia present but no symptoms Hyperuricemia present, on medications Arthropathy present Destructive joints present Disabled, no walking Diabetes: Check any/all that apply to you No Diabetes Elevated fasting glucose Oral meds only Insulin only Insulin and oral meds Complications present Hair/Nail Changes Rosacea Bleeding Disorder Lymphoma Blood Transfusion Use of Blood Thinners Easy Bruisability Endocrine/Metabolic Continued: Dyslipidemia: (abnormal cholesterol/triglycerides) Check any/all that apply to you: No Dyslipidemia No treatment required Lifestyle change Single medication Multiple medication Poorly controlled Please check any/all that apply to you: Excessive urination Excessive thirst Low blood sugar Endocrine gland tumor Elevated Calcium level Abnormal facial hair growth Hypothyroid (low thyroid) Hyperthyroid (overactive) Parathyroid Problems Goiter Other: _________________________________________________ _________________________________________________ _________________________________________________ Respiratory Sleep Apnea-please check any/all that apply to you: No history of sleep apnea Symptoms but sleep study/test negative Positive sleep study/test Require appliance/CPAP at night Have hypoxia (low oxygen) or dependent on oxygen Have complications related to sleep apnea Pulmonary Hypertension, check any/all that apply to you: No history of Pulmonary Hypertension Symptoms only (tiredness, shortness of breath, dizziness) Confirmed diagnosis Well controlled on medications Require oxygen or stronger meds Pt needs/requires or has had lung transplant Respiratory (continued): Asthma, check any/all that apply to you: No history of Asthma Occasional Mild Symptoms, not on any meds Symptoms controlled on oral meds or inhalers Well controlled with daily medications Poorly controlled, requiring steroids or anticholinergics Hospitalization in the last 2 years/history of intubation Obesity Hypoventilation Syndrome: Check any/all that apply to you: No history of OHS Low oxygen on room air Severely low oxygen Pulmonary Hypertension Right Heart Failure Right heart failure/Left Ventricular Dysfunction Please check any/all that apply to you: Chronic cough Shortness of Breath at rest Emphysema/COPD Bronchitis Pneumonia Suspicious of Sleep Apnea but not ever diagnosed Psychosocial Psychosocial Impairment: Check any/all that apply to you: No impairment Mild impairment, able to perform primary tasks Moderate impairment, able to perform most primary tasks Moderate impairment, unable to perform most primary tasks Severe impairment, unable to function Confirmed Mental Health Disorder: Check any/all that apply to you: None Bipolar Anxiety/Panic Disorder Personality Disorder Psychosis Psychosocial (continued): Depression: Check any/all that apply to you: No Symptoms Episodic, no treatment required Moderate with some impairment, may require treatment Moderate with significant impairment, treatment indicated Severe, intensive treatment indicated Severe, hospitalization required Check any/all that apply to you: Alcohol Use: Tobacco Use: Substance Abuse: No alcohol No tobacco No Rarely Rarely Rarely Occasionally Occasionally Occasionally Frequently Frequently Frequently Neurologic Please check any/all that apply to you: Migraine Balance disturbance Seizure or Convulsions Weakness Recurrent headaches Numbness and Tingling Dizziness Stroke Multiple sclerosis Restless Leg Knocked unconscious Musculoskeletal Disease Back Pain: Check any/all that apply to you: No Back Pain Intermittent symptoms Non narcotic treatment Degenerative changes, narcotic treatment Surgical treatment done or recommended Failed surgical treatment Musculoskeletal Disease (continued): Fibromyalgia: Check any/all that apply to you: No fibromyalgia Treatment with exercise Treatment with non narcotic medications Treatment with narcotics Surgical Treatment done or recommended Disabled, surgery failed Musculoskeletal Disease: Check any/all that apply to you: No musculoskeletal disease Pain with community ambulation Non narcotic analgesia Pain with household ambulation Surgical intervention required Joint replacement done or recommended Please check any/all that apply to you: Neck Pain Shoulder Pain Wrist Pain Hip Pain Knee Pain Ankle Pain Foot Pain Heel Pain Ball of foot / Toe Pain Lupus Scleroderma Autoimmune Disease Muscle Pain Sciatica Plantar fasciitis Carpal Tunnel Rheumatoid arthritis Broken Bones Other: ________________________________________________ ________________________________________________ Bladder: Check any/all that apply to you: Kidney Stones Blood in Urine Prostate Problems Burning on urination Urinary Urgency Kidney Failure / Renal Insuff Leaking Urine when Sneezing Previous PSA test (males only) Trouble Starting Gastrointestinal Please check any/all that apply to you: Abdominal Pain Heartburn Stomach Ulcers Hiatel Hernia Incisional Hernia Diarrhea Blood in stool Change in Bowel Habits Constipation Irritable Bowel Colitis Crohn’s Disease Hemorrhoids Rectal Bleeding Black tarry stools Colon Polyps Pancreatic Disease Barrett’s Esophagus Difficulty Swallowing Nausea /Vomiting Other: _____________________________________________________ _____________________________________________________ _____________________________________________________ GERD (Gastroesophageal Reflux Disease): Check any/all that apply to you: No GERD Variable symptoms Require only intermittent medications H2 blockers (pepcid, zantac) or low dose PPI (Prevacid, Prilosec, Nexium, etc) High dose PPI Criteria for or history of anti-reflux surgery Gallstones: Check any/all that apply to you: No Gallstones Asymptomatic (stones present) Intermittent symptoms Severe symptoms, previous cholecystectomy Immediate GB surgery prior to weight loss surgery Previous cholecystectomy with unresolved complications Liver Disease: Check any/all that apply to you: No Liver Disease Mild hepatomegaly, normal LFT’s, cat. 1 fatty liver Mod. hepatomegaly, altered LFT’s, cat. 2 fatty liver Marked hepatomegaly, cat. 3 fatty liver, mild fibrosis NASH, cirrhosis, hepatic dysfunction Failure, need for or previous transplant Cardiac Hypertension: Check any/all that apply to you: No Hypertension Borderline HTN Positive diagnosis Controlled with single medication Multiple Medications Poorly Controlled Angina: Check any/all that apply to you: No Angina Angina with extreme exertion Angina with moderate exertion Angina with minimal exertion Unstable Angina Previous MI by history or work-up Congestive Heart Failure: Check any/all that apply to you: No CHF Class I – exertion only Class II – ordinary activity Class III – minimal activity Class IV – at rest Peripheral Vascular Disease: Check any/all that apply to you: No PVD Asymptomatic with bruit Claudication, anti-ischemic meds Transient ischemic attack, rest pain Previous procedure for PVD Stroke, loss of tissue Deep Venous Thrombosis: Check any/all that apply to you: No Previous DVT Resolved with medications History of recurrent DVT’s Previous PE History of recurrent PE’s Has Vena Cava Filter Cardiac (continued): Ischemic Heart Disease: Check any/all that apply to you: No IHD Abnormal EKG History of MI/anti-ischemic meds Previous CABG/catheterization Active ischemia Lower Extremity Edema: Check any/all that apply to you: No edema No treatment Treatment Stasis ulcers present Disability, hospitalization Please check any/all that apply to you: Pacemaker Rapid Heart Rate Varicose Veins Heart Murmur / Atrial Fibrillation Irregular / Skipped heart beats Rheumatic fever / Valve Damage / MVP Other: ______________________________________________________ ______________________________________________________ ______________________________________________________ Constitutional: Please check any/all that apply to you: Fevers Chills Night Sweats Anemia Hair Loss Fatigue Weight Gain Insomnia Appetite Change Other: _______________________________________________________ _______________________________________________________ Head and Neck: Please check any/all that apply to you: Wears Contacts / Glasses Blurred / Double Vision Glaucoma Hearing Problems Chronic Allergies Sinus Drainage Dentures (partial/full) Ear Infections Nose Bleeds Hoarseness