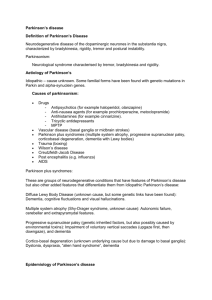
Drug treatments for Parkinson`s booklet Word version
advertisement

Drug treatments for Parkinson’s 1 While there is no cure yet for Parkinson’s, there are many different drugs that can help manage the symptoms.1 This booklet is for people with Parkinson’s and their families. It provides information about the drugs most commonly used to help manage the condition. This booklet starts with some practical points about the drugs used for treating Parkinson’s, then gives further details about each individual drug, including: its name how it works how it’s used advantages disadvantages There is also a section that explains more about clinical trials and possible new drug treatments, and a glossary to explain the meaning of unfamiliar medical words or terms and how to say them phonetically. No booklet is a substitute for advice from your specialist or Parkinson’s nurse. Choosing the right medication is always a decision you should make with them. With this in mind, you can show this booklet to your specialist or Parkinson’s nurse and ask them questions about the information here. You may find it a useful starting point when you are talking about the next steps in your treatment. The content in this booklet is designed to be dipped in and out of – don’t feel like you need to read everything in one go. 2 Contents Disclaimer 5 Drugs used to treat Parkinson’s – an overview Individual treatment Getting it right How the drugs work Managing other (non-motor) symptoms 6 6 6 7 7 Practical points Dos and don’ts Taking special care with Parkinson’s drugs If you have other conditions or take other medications Get It On Time Drugs to avoid 8 8 10 10 11 11 Types of Parkinson’s drugs 12 Levodopa Other names: co-beneldopa (Madopar, Madopar CR) co-careldopa (Caramet CR, Duodopa, Sinemet, Sinemet Plus, Sinemet CR, Half Sinemet CR, Lecado, (Stalevo/Sastravi) 13 Dopamine agonists 17 Other names: pramipexole (Mirapexin, Mirapexin prolonged release), ropinirole (Ralnea XL, Requip, Requip XL, Spiroco XL), apomorphine (APO-go PEN, APO-go PFS), bromocriptine (Parlodel), cabergoline (Cabaser), pergolide, rotigotine (Neupro), Monoamine oxidase type B (MAO–B) inhibitors Other names: rasagiline (Azilect), selegiline (Eldepryl, Zelapar) 23 Catechol-O-methyltransferase (COMT) inhibitors 25 Other names: entacapone (Comtess), co-careldopa plus entacapone (Stalevo/Sastravi), tolcapone (Tasmar), Glutamate antagonist Other names: amantadine 27 Anticholinergics Other names: orphenadrine (Disipal, Biorphen), procyclidine (Arpicolin, Kemadrin), trihexyphenidyl (benzhexol) (Broflex) 29 Managing your medication 31 Developing new drugs 32 More information and support 35 Summary of drugs used to treat Parkinson’s 37 3 Glossary 39 Non-motor symptoms questionnaire 45 4 Disclaimer We’ve made every effort to make sure the information in this booklet is correct at the time of printing. But Parkinson’s UK cannot take responsibility for the correctness, sufficiency or completeness of this information or any recommendation. You should speak to a medical professional about your individual healthcare needs. Because everyone with Parkinson’s is different, Parkinson’s UK cannot advise on ideal combinations or provide details about the strengths or duration of action for each medication. Your specialist or Parkinson’s nurse (if you have one) will be able to give advice or information that’s relevant to your particular circumstances. You can also speak to a pharmacist for more information about your medication. Please remember that information about drugs can change. This booklet does not list all the uses and side effects of these drugs. For full details, please see the drug information leaflet that comes with your medication. “My Parkinson’s nurse has been marvellous – very knowledgeable, encouraging and helpful about medication. He has seen my condition progress and has been able to make appropriate suggestions.” Caroline, diagnosed in 2003 5 Drugs used to treat Parkinson’s – an overview “No two people with Parkinson’s have the same symptoms, so at first, it’s a case of trial and error. But once the right combination is found for your symptoms, the drug treatment for Parkinson’s is very good.” Steve, diagnosed in 1999 Research has led to a range of different medications that are now available for Parkinson’s that can help manage or reduce symptoms, such as tremor or problems with co-ordination, balance and movement.1 Since the 1960s, the standard drug to treat Parkinson’s has been levodopa.1 It works by boosting the levels of dopamine in the brain and can help to manage the symptoms (see page 13 for more information). Other drugs have been developed since then that also work to increase dopamine levels. These include MAOB-inhibitors,1 which first became available in the 1970s and dopamine agonists1 that were developed in the 1980s, 1990s and 2000s. More recently, drug companies have been working to refine the way Parkinson’s medications can be delivered to provide longer lasting symptom control. 1 But while current medications can help to manage symptoms, we don’t yet have any treatments that can cure, slow, stop or reverse the development of Parkinson’s.1 This means the condition continues to progress as do the symptoms and side effects of taking more medication. Individual treatment Every person with Parkinson’s has a different experience of the condition. Some symptoms may trouble you more or less than they do another person. Your specialist or Parkinson’s nurse will work with you to find the treatment that is best for you as an individual.1 Finding the best medicine, dose and timing may take some time and will need some changes along the way. Because the symptoms of Parkinson’s change over time, your medication may have to change, too.1 While you may be able to talk to your GP about any side effects of your medication or issues that aren’t related to your condition, ideally, you should discuss Parkinson’s medication with your specialist, Parkinson’s nurse or pharmacist. It is important not to make any changes to your medication, or to stop taking it, without talking to your specialist or Parkinson’s nurse first.2 Getting it right When you are diagnosed with Parkinson’s you will have a consultation with your specialist to discuss whether you need to start treatment immediately. For a lot of people who have just been diagnosed, Parkinson’s drugs can be a great help. Carefully introducing the best drug for treating Parkinson’s can often improve the symptoms.2 6 Drug treatment for Parkinson’s is often started at low doses and increased gradually, stepping up the doses, the frequency, or adding new drugs until your symptoms are as controlled as possible.3 If your symptoms are mild, you might decide, together with your specialist, to postpone drug treatment until your symptoms increase.1 “My specialist is very easy to talk to and allows me to take an active part in my treatment. He makes sure that I have the relevant information to decide on medication – I am in the driving seat.” Josie, diagnosed in 2007 How the drugs work The symptoms of Parkinson’s appear when dopamine levels – a chemical messenger in your brain – become too low. This is because many of the cells in your brain that produce dopamine have died or are dying.1 When dopamine levels in your brain get low, you will find that your movement slows down and it takes you longer to do things. You may lack co-ordination or your hands or other parts of your body may shake.1 This is known as tremor and can make everyday activities difficult or frustrating. You may find it difficult to move freely and that your muscles might become stiff. Some people with Parkinson’s freeze suddenly and this leaves them unable to move.4 This is a Parkinson’s symptom, but can also be a sign that medication is not working as effectively as before.4 Sometimes a person’s symptoms will recur before the next dose of medication is due. This is sometimes called ‘wearing off’.4 When the effects of wearing off happen quickly, this is called ‘on/off’.5 Being ‘on’ describes when a person’s symptoms are controlled and they are feeling at their most capable. Being ‘off’ is when Parkinson’s symptoms recur and are at their most debilitating. Some people have described this as like a light switch being turned on and off, or going up-anddown like a yo-yo. Most drug treatments for Parkinson’s aim to ease these symptoms by:3 increasing the amount of dopamine in the brain, or acting as a substitute for dopamine by stimulating the parts of the brain where dopamine works, or blocking the action of other factors (enzymes) that break down dopamine Managing other (non-motor) symptoms People with Parkinson’s can also have non-motor symptoms – symptoms that aren’t connected to movement problems. These include anxiety and depression, pain and constipation.6 Parkinson’s drugs are not always used to treat these types of symptoms.1 Some types of non-motor symptoms will be treated separately, depending on the problems you 7 experience. Constipation and depression, for example, may be treated with drugs designed to treat those symptoms. There are too many different treatment options to include all of the drugs for other symptoms in this booklet. Also, people with Parkinson’s will often receive the same or similar treatment for other symptoms as people without Parkinson’s, for example sleeping problems (as long as the medication is compatible with their Parkinson’s medication and other factors of their condition). Some people may experience side effects of Parkinson’s medication.3 These are explained throughout the booklet. It is important to speak to your specialist or Parkinson’s nurse about anything you experience. We have a range of free information sheets about particular symptoms and side effects. See the inside back cover for details of how to order these. Always tell your specialist or Parkinson’s nurse about any other symptoms you have. This can be done by giving them a copy of our non-motor questionnaire that you’ve filled in. The questionnaire is available on page 45. You can also download it from our website at parkinsons.org.uk/publications It’s also important to remember that not every health issue you experience will be related to Parkinson’s. So try not to worry that every symptom is caused by Parkinson’s or is a sign that your condition is getting worse. Just make sure you talk to your healthcare professional about any concerns you may have. Practical points Whatever treatment you and your specialist or Parkinson’s nurse decide on, you may find it helpful to bear these tips in mind. Do: Keep a record of all the medications you are taking for Parkinson’s and what time you take each drug. Do this for medication you take for other conditions as well. Ask questions or have your specialist, Parkinson’s nurse or pharmacist explain something again if you don’t understand. They won’t mind. You can also ask for written information. Keep a diary or chart when your specialist or Parkinson’s nurse starts you on a new drug, changes your drugs or adjusts the dose or frequency. Record the dose and time you took the drug and what happened to your symptoms. This information can help the healthcare professional who is adjusting your medication. Tell your specialist or Parkinson’s nurse if you think you could be pregnant. 8 Take your Parkinson’s drugs as recommended by your specialist or Parkinson’s nurse. Make sure you understand what to do if you forget a dose. Tell your specialist or Parkinson’s nurse straight away if you experience any side effects from the drugs you take to treat Parkinson’s, but don’t stop taking your Parkinson’s drugs until you are advised to do so.2 Tell your specialist or Parkinson’s nurse about how your treatment is working for you. Making notes before your appointment can help you remember what you want to say. Remember that your pharmacist can also be a very good source of advice. They will also help you dispose of all your unused drugs if necessary. Keep your medication out of the reach of children or other people who might be confused and take it by mistake. Store it as advised on the packet. Don’t: Assume that you will have serious side effects from the drugs you take to treat Parkinson’s. Not everyone does. However, if you think you are having side effects or if you are worried about them, talk to your specialist, Parkinson’s nurse or pharmacist right away. Assume that your treatment, dose or the timing of your medication should be the same as other people with Parkinson’s. Everyone is different. Change the dose or how often you take your medication on your own. You should speak to your specialist or Parkinson’s nurse if you think your medication needs changing in any way.2 Forget to tell the doctors and nurses you are taking drugs to treat Parkinson’s, if you go to hospital. You should make sure staff understand that you need your medication on time. Some hospitals will allow you to look after your own medication, so that you can self-administer medication outside of the usual drugs round.1 Find out more: see our booklet Going into hospital when you have Parkinson’s. Forget to wear a medical alert bracelet or necklace if you want to make health professionals aware of your condition and the drugs you are taking in the event of an emergency. These are items of jewellery that can be inscribed with important medical information and are widely available. You can also order our medication card, on which you can write down the drugs you are taking, and store this in your purse or wallet. You can download the medication card from parkinsons.org.uk/publications or use the details on page 48 to order a print copy. 9 Do not stop taking your Parkinson’s medication unless your specialist or Parkinson’s nurse tells you to. This can be dangerous and should only be done or stopped gradually with medical supervision.2 “It is important that other people realise the ‘on/off’ nature of Parkinson's, otherwise they may not give the help needed because they believe the person with Parkinson’s is 'putting it on'.” Beryl, diagnosed in 1996 Taking special care with Parkinson’s drugs It’s important that you tell your specialist or Parkinson’s nurse about any other medical conditions you have and any other medications you are taking. If you are pregnant, breastfeeding, or suspect you may be pregnant tell your specialist or Parkinson’s nurse. Some Parkinson’s drugs can make you very sleepy.1 Sometimes this happens suddenly and without warning. Make sure you understand what safety precautions you need to take – whether you can drive, for example.7 Sometimes it can be hard to know whether your sleep problems are part of the condition or whether they are a side effect of your Parkinson’s medication. It’s important to talk to your healthcare professional to find out the cause of these problems. Find out more: see our booklets Driving and Parkinson’s and Sleep and night-time problems in Parkinson’s. Some Parkinson’s drugs can make your blood pressure fall very quickly1, causing you to feel dizzy or faint.8 Again, find out what safety precautions you should take in case this happens. With some Parkinson’s drugs, particularly dopamine agonists (see page 17) and in a small number of cases levodopa (see page 13), some people have problems with impulsive or compulsive behaviour (see page 21).9 Examples include gambling, becoming a ‘shopaholic’, binge eating or focusing on sexual feelings and thoughts, which may get in the way of everyday life.4 This behaviour can have a huge impact on people’s lives, so if you think this is happening to you or the person you are caring for, tell your GP, specialist or Parkinson’s nurse straight away. Find out more: see our information sheet Impulsive and compulsive behaviour in Parkinson’s. If you think you are experiencing any side effects (you can find examples of these in each section of this booklet), tell your specialist or Parkinson’s nurse right away, but do not stop taking your Parkinson’s drugs unless they tell you to.2 10 If you have other conditions or take other medication If you take medication for other medical conditions, they may have an effect on your Parkinson’s symptoms and how effective your Parkinson’s drugs are. Some medications for other conditions can make Parkinson’s symptoms worse.10 Speak to your GP, specialist, Parkinson’s nurse or pharmacist if you have any concerns about this. Also, if you have a problem with your digestive system, such as constipation (which is often experienced by people with Parkinson’s), this may affect how well your drugs enter your bloodstream. This may reduce the effectiveness of your medication.11 Parkinson’s drugs can interact with the drugs used for other conditions.10 The different drugs can make each other weaker or stronger. This can be dangerous. Herbal or complementary treatments, for example St John’s Wort, may also affect your Parkinson’s drugs.12 If you want to take a non-prescription medicine, check with your pharmacist first that it is safe. It’s important that you give every healthcare professional who treats you details of the drugs you are taking for Parkinson’s. Your specialist, Parkinson’s nurse or pharmacist can give you advice on specific interactions with different medications. Get It On Time Our Get It On Time campaign aims to raise awareness of the importance of people with Parkinson’s getting their medication on time, every time, with hospital and care home staff. It is important for them to be aware that drug timings will vary from person to person and may be different to ward drug rounds. If people with Parkinson’s don’t get their medication at the right time, it leads to their symptoms becoming uncontrolled, and it can take some time for this to be put right again.1 Find out more at parkinsons.org.uk/getitontime “We had some trouble with getting medication on time when mum was first admitted to hospital. But then we had one fabulous nurse who picked up on the importance of mum’s medication on her admission to the ward. Mum was put as a priority on the drugs round.” Julie, whose mum has Parkinson’s Drugs to avoid Some drugs can bring on Parkinson’s-like symptoms or react badly with Parkinson’s drugs and should be avoided unless they’re recommended by a specialist.10 These are some (but not all) of the drugs to avoid in Parkinson’s: chlorpromazine13 (Largactil) fluphenazine13 (Modecate) 11 perphenazine13 (Fentazin/Triptafen) trifluoperazine13 (Stelazine) flupenthixol13 (Fluanxol/Depixol) haloperidol13 (Serenace/Haldol) metoclopramide10 (Maxalon) prochlorperazine10 (Stemetil) Decongestants or cold remedies can affect some Parkinson’s medications 10. If you need to use these, it’s very important to check with your pharmacist which one is safest to use. Anti-sickness drugs Domperidone14 (Motilium) is the anti-sickness drug of choice to prevent and treat nausea and vomiting caused by levodopa. Domperidone can cause heart rhythm problems (arrhythmia) in some people over the age of 60.14 If you are prescribed this medication, your specialist, Parkinson’s nurse or pharmacist should talk to you about how to recognise signs of irregular heart rhythms.14 You may also have an electrocardiogram (ECG) before starting treatment. An electrocardiogram measures heart rhythm and electric activity and can identify problems,15 which may mean domperidone is not suitable for you to take. 16 Other anti-sickness drugs that are generally considered useful include cyclizine (Valoid)17 and 5-HT3 receptor antagonists like ondansetron.18 If you have any queries about medication, contact your specialist, Parkinson’s nurse or pharmacist. Types of Parkinson’s drugs There are many different drug treatments for Parkinson’s. The tables in each of the following sections give you a summary of the main types, their names and how they are used. Drug names Sometimes, the same drug goes by a number of different names – even if the ingredients are the same and they do the same job.19 Class Each drug belongs to a class – a wider group of drugs that work in the same way. Unbranded (generic) and brand name All types of drug have a common or generic name. Every drug that has the same active ingredient will have this name, no matter who it is made by. In addition to its common name, some drugs will also have a brand name, decided by the company who makes it. 12 For example, in the levodopa class of drugs, co-beneldopa is an unbranded or generic, name of a drug. Roche, one of the companies that makes co-beneldopa, sells it under the brand name Madopar. Many medications used to treat Parkinson’s are available under their generic name. The active ingredient of the unbranded drug is the same as the branded version and lots of people won’t have any problems using the generic medication. But some people may find they respond a bit differently to different versions. It is advised that you don’t regularly switch between branded and unbranded versions as in some cases this can have negative effects. If you have any concerns you should discuss these with your specialist or Parkinson’s nurse. Levodopa20 This section explains what levodopa is and how it works, and looks at other considerations, including possible side effects. How levodopa works How levodopa is used Advantages of levodopa Disadvantages of levodopa Diet Side effects 14 14 15 16 16 17 Levodopa is always given combined with either benserazide or carbidopa. 20 These help the levodopa get into the brain where it’s needed. Unbranded (generic) name Co-beneldopa (benserazide plus levodopa) Co-careldopa Brand names Forms available Madopar Capsules, dispersible tablets Madopar CR Controlled release (CR) capsules (see page 15) Available in unbranded form capsules Caramet CR Controlled release tablets 13 (carbidopa plus levodopa) Co-careldopa plus entacapone (see page 25 for information about entacapone) Duodopa Intestinal gel Sinemet Tablets Sinemet Plus Tablets Sinemet CR Controlled release tablets Half Sinemet CR Controlled release tablets Lecado21 Prolonged release tablets Available in unbranded form Tablet Stalevo/Sastravi22 Tablets Taking special care with levodopa If you are prescribed this drug for Parkinson’s, please make sure you read the important safety advice that comes with it and the general information on page 10. How levodopa works The symptoms of Parkinson’s appear when levels of dopamine – a chemical messenger in your brain – become too low. This is because many of the cells in your brain that produce dopamine have died or are dying.1 Unfortunately, taking dopamine as a drug doesn’t help as it can’t cross into your brain where it’s needed.23 Doctors can get around this by using levodopa. Levodopa is a chemical building-block that your body converts into dopamine.1 Levodopa already occurs naturally in your body and taking it as a drug treatment boosts the supply, meaning the nerve cells can make more dopamine. How levodopa is used Levodopa has been used to treat Parkinson’s since the 1960s. 24 Later, it was found that adding benserazide or carbidopa could allow more levodopa to get into the brain and 14 make it work better. Levodopa is now always given with one of these, combined in the same pill.20 Levodopa can be used at all stages of Parkinson’s, however, it can have side effects that build up as symptoms progress.1 One side effect of levodopa is fluctuations, or ‘on/off’.5 During ‘off’ periods your body can become stiff and slow so you are unable to move. During ‘on’ periods your symptoms will be controlled and you’ll feel at your most capable.3 Another side effect that can happen with long-term use of levodopa is involuntary movements (dyskinesia).3 Although levodopa may be taken at any time during your condition, based on current scientific evidence, there is no particular time to start taking levodopa that is right for everyone.25,1 You and your specialist or Parkinson’s nurse will need to talk about it and agree what is the best choice for you. Treatment will usually start with a low dose. This is gradually increased until you and your specialist or Parkinson’s nurse agree that your symptoms are under control.3 If you have problems with swallowing, you may be able to take a different form of medication. There may be a suitable option that is easier to swallow, if you can’t easily take tablets, for example.20 There are some options that release the active ingredients slowly (controlled or prolonged release capsules or tablets), which allow you to take fewer tablets in a day.20 However, these will not be suitable for everyone who takes levodopa. The different forms of levodopa are:20 Tablets These come in different strengths, depending on the dose your specialist or Parkinson’s nurse thinks you need. Controlled release (CR) or prolonged release capsules or tablets These let the levodopa enter your body slowly instead of all at once. Involuntary movements (dyskinesia) can be a side effect of taking high doses of levodopa. Controlled release options can sometimes reduce the number of times this happens. They are particularly helpful if they are taken before going to bed to reduce stiffness during the night.1 Dispersible tablets This form can be mixed with water to make a drink. It takes effect more quickly than capsules because it doesn’t need to be broken down in your stomach to release the active ingredient. It can also be used if you have trouble swallowing tablets or capsules. If you are prescribed non-dispersible tablets or capsules, these should not be crushed or put into water. Intestinal gel26 This option is only suitable for a very small number of people whose symptoms can’t be controlled with the more common forms of treatment. The drug is pumped continuously through a tube that is surgically inserted into the intestine. If you are prescribed this option you are less likely to experience involuntary movements. You might also have fewer ‘off’ periods. It may also help to control your symptoms at night. 15 Advantages of levodopa Levodopa is an effective treatment for Parkinson’s symptoms. You may experience a big improvement in your symptoms when taking it, especially with stiffness and slowness of movement.3 Disadvantages of levodopa Becomes less effective over time as symptoms progress3 After a while, you may have a less predictable response to levodopa. This happens as more of the nerve cells in the brain that produce dopamine die. You may get ‘off’ periods when you feel weak and can’t move well. The effect of your dose may wear off more quickly, maybe even before your next one is due or has begun to work. When this happens, sometimes your specialist or Parkinson’s nurse will change or increase your dose, the form of drug or how often you take it. They may also add other Parkinson’s drugs to take alongside levodopa. This will help it to be more effective in treating your Parkinson’s symptoms. Movement problems One of the main problems with levodopa is dyskinesia.3 These are spasms or muscle movements that you can’t control. Dyskinesia may increase over time, although not everyone will have this side effect. Sleepiness and fainting Levodopa drug treatment can make you feel very sleepy. Sometimes this happens quite suddenly and without warning.20 Levodopa can also make you faint or feel dizzy.20 Impulsive and compulsive behaviour A small number of people taking levodopa have problems with impulsive or compulsive behaviour.9 This can also be called impulse control disorder. It affects fewer people taking levodopa than those taking dopamine agonists9 (see page 17), but it is still a possible side effect. Find out more: see our information sheet Impulsive and compulsive behaviour in Parkinson’s. Withdrawal syndrome with levodopa Research has shown that withdrawal symptoms can happen when someone stops taking levodopa very suddenly, perhaps because they are experiencing impulsive and compulsive behaviour. It can lead to symptoms including depression, anxiety or pain. 29 Any withdrawal from Parkinson’s drugs needs to be done gradually, under the supervision of a health professional, to avoid the risk of developing this syndrome. Diet 16 Taking levodopa with food can sometimes help to reduce feelings of sickness. However, for some people, protein (which is found mainly in meat, fish, eggs, cheese and beans) seems to interfere with the way levodopa medication works, by affecting how well the drug is absorbed by the body.27 Your body needs protein, so it’s important not to stop eating it. However, some people may benefit from taking their medication at least 30 minutes before they eat.28 Your specialist or Parkinson’s nurse can advise you on timing your doses and this should be discussed with them when you are first prescribed the drug. They can also refer you to a dietitian. Find out more: see our booklet Diet and Parkinson’s. “If I have food and particularly if I have protein, I find that levodopa doesn’t work and I experience freezing. I’m amazed when I hear that other people with Parkinson’s haven’t always been told that this can happen. It has a huge effect on me.” Paul, diagnosed in 2001 Side effects20 We can’t list all the possible side effects of all Parkinson’s drugs in this booklet. However, some of the most common side effects that can happen with levodopa include nausea and vomiting, low blood pressure (hypotension), loss of appetite, psychological problems, hallucinations (seeing, hearing, feeling and smelling things that aren’t there), and sleep problems. Dopamine agonists30 This section explains what dopamine agonists are and how they work, and looks at other considerations, including possible side effects. How dopamine agonists work How dopamine agonists are used Advantages of dopamine agonists Disadvantages of dopamine agonists Impulsive and compulsive behaviour Side effects Unbranded (generic) name Brand names Pramipexole Available in unbranded form 19 19 20 21 21 23 Forms available Tablets 17 Ropinirole Rotigotine Mirapexin prolonged release Prolonged release tablets Mirapexin Tablets Available in unbranded form Tablets Ralnea XL Prolonged release tablets Requip Tablets Requip XL Prolonged release tablets Spiroco XL Prolonged release tablets Adartrel tablets Eppinix XL Prolonged release tablets Neupro Skin patch APO-go PEN Pre-filled pen for intermittent injection31 APO-go PFS Pre-filled syringe for infusion. Can be used with a continuous infusion pump31 Parlodel Tablets, capsules Apomorphine Bromocriptine 18 Available in unbranded form Tablets Cabaser Tablets Available in unbranded form Tablets Available in unbranded form Tablets Cabergoline Pergolide Taking special care with dopamine agonists If you are prescribed these drugs for Parkinson’s, please make sure you read the important safety advice that comes with them and the general information on page 10. How dopamine agonists work Dopamine is a chemical messenger made in the brain. The symptoms of Parkinson’s appear when dopamine levels become too low. This is because many of the cells in your brain that produce dopamine have died or are dying.1 One treatment option is to use levodopa, which is converted into dopamine in the brain (see page x). Another possible approach is to use dopamine agonist drugs, which act like dopamine to stimulate your nerve cells.3 How dopamine agonists are used Dopamine agonists are used at all stages of Parkinson’s.1 You might take them alone when treatment is being started or alongside levodopa to help the levodopa work better. 3 Treatment with dopamine agonists has to be started carefully, with the dose gradually being increased until you and your specialist or Parkinson’s nurse are happy that your symptoms are under control.3 Some dopamine agonists are now available as ‘one-a-day’ tablets.32 These can be a convenient option for people and may help both movement and other symptoms of Parkinson’s. 19 Several different forms are available: Tablets and capsules These come in different strengths, depending on the dose your specialist or Parkinson’s nurse thinks you need. Prolonged release tablets These can be taken less frequently and they work longer in the body, compared to normal capsules and tablets. Skin patch A dopamine agonist patch is also available (Neupro).33 It may be useful if you have trouble swallowing tablets. The patch should be held in place for 30 seconds, but it is left on for 24 hours.34 The patch may cause a skin reaction, such as reddening or itching, but this is usually mild or moderate.34 It will only affect the area the patch has been and will normally disappear after a few hours when you remove the patch. Moving the patch to a different part of your body every day will help to avoid irritation.34 Some, but not all, patches may need to be stored in a refrigerator – check the instructions included with your medication or speak to your pharmacist. Injection or infusion Apomorphine is a strong dopamine agonist that is given by injection or infusion pump.35 It is saved for more advanced Parkinson’s that does not respond as well to oral drug treatments or when most oral Parkinson’s medication becomes less effective or does not work.1 If you continue to have unpredictable changes in your symptoms that aren’t controlled by other Parkinson’s medications, apomorphine may help.4 Apomorphine injections are taken in a similar way to insulin for diabetes. There is a readyto-use injection pen that works within 10 minutes36 and is often used as a ‘rescue’ measure.37 This is very useful if you have a sudden ‘off’ period. If you need more than 10 injections a day, you may be changed to a syringe driver.38 This is a small, battery-driven pump that delivers a continuous dose of medication from a syringe through a needle under the skin.38 Ideally, apomorphine will be started in hospital, under the guidance of a specialist or Parkinson’s nurse.1 Once you are settled on this treatment, you and your carer (if you have one) can be trained in how to use it. If you or a carer are unable to do this, district nurses will be able to help you with this treatment.39 APO-go nurse advisors can also start you on treatment. They are registered general nurses with specialist experience in APO-go injections and infusions as well as the general management of Parkinson’s. Apomorphine can cause severe short-term nausea and sickness,1 so an anti-sickness drug called domperidone (Motilium) will also be given at least two days before this treatment is started1 and continued for at least two weeks or more, once your treatment is underway (see page 12 for more information). 20 Soreness or nodules can develop at the place where the needle enters your skin.38 If this happens, do not stop the treatment and make sure to get advice from your specialist or Parkinson’s nurse. It is important to change the injection site each time to minimise skin becoming sore or nodules forming. Simple massage,40 silicone gel patches41 or ultrasound38 can help to reduce any nodules that form. Find out more: see our information sheet Apomorphine. Advantages of dopamine agonists Delaying levodopa treatment Dopamine agonists may be effective treatments for several years when used alone.1 However, this will not be the case for everyone. Lowers levodopa needs Taking dopamine agonists may mean you can take lower doses of levodopa as your condition progresses. This can reduce the risk of experiencing involuntary movements (dyskinesia) or reduce how severe they are.3 Fewer movement problems Your symptoms may be controlled for longer than is usually the case with levodopa. You may also be less prone to long-term side effects such as dyskinesia (movements that you can’t control).3 Helping levodopa work better Dopamine agonists can also be taken with levodopa, at all stages of Parkinson’s. They can help when the effect of levodopa wears off or doesn’t work as well. Dopamine agonists may help to smooth out the ‘on/off’ effect that you may have with levodopa.1 Fewer tablets to take (in some cases) There are now some once-daily preparations that could make a big difference by reducing the number of tablets you take.32 But this option may not suit everyone. Positive effects on non-movement symptoms Some dopamine agonists have recently been shown to have a good effect on the symptoms of Parkinson’s not related to movement, including sleep problems, pain and mood.42 Disadvantages of dopamine agonists Heart problems Some of the older dopamine agonists increase the risk of heart problems.1 As a group, these are known as the ‘ergot’ types and they include bromocriptine, pergolide and cabergoline.1 Because of this risk, these Parkinson’s drugs are not commonly used. 21 All newer dopamine agonists are non-ergot in type. These are apomorphine, pramipexole, ropinirole and rotigotine. They have not been associated with an increased risk of heart damage. Doctors prefer to use these if possible.30 Sleepiness and fainting Dopamine agonist drugs can make you feel very sleepy, faint or dizzy.3 This is most likely to happen when you start taking the drugs. Once a stable dose is reached, this effect often wears off. In a few people, sleepiness happens quite suddenly. Sudden onset of sleep, without any warning, has been reported.30 If this happens, it’s important that you tell your specialist or Parkinson’s nurse. Impulsive and compulsive behaviour Some people taking dopamine agonists have problems controlling compulsive and impulsive behaviour. It may also affect people taking levodopa, but more frequently it affects people taking dopamine agonists.9 Impulsive behaviour is when a person can’t resist the temptation to carry out certain activities that could lead them to harm themselves or others. This includes a strong urge to gamble, shop or binge-eat.4 Some people with Parkinson’s experience hypersexuality, where they become so preoccupied with sex that it can cause problems with their work or personal life.4 Compulsive behaviour is when a person has an overwhelming drive or urge to act in a certain way, often repetitively, to reduce the worry or tension that they get from their drive or urge. This can include collecting, sorting and organising objects. 43 In a lot of cases, this behaviour is out of character. The person experiencing this behaviour may or may not experience distress, and may not realise the effects their behaviour will have.44 If you think this is happening to you or the person you are caring for, tell your GP, specialist or Parkinson’s nurse right away. It is important that everyone with Parkinson’s is assessed for any potential risk of impulsive and compulsive behaviour before they start taking their medication. There are certain factors that may mean you’re more likely to experience this behaviour. These include a family history of gambling or alcohol abuse, a personal history of addictive behaviour, being male, being a younger person with Parkinson’s, being a smoker, being single and living alone.45 Even if you do not fit any of these categories, your treatment should be monitored over time. People with Parkinson’s, their carers, friends and family members should work with healthcare professionals to monitor any changes in behaviour. Find out more: see our information sheet Impulsive and compulsive behaviour in Parkinson’s. 22 “If you’re aware that you, or a friend or relative, may be experiencing impulsive and compulsive behaviour, use the information available. Don’t live in denial. Speak with a healthcare professional. I don’t want anyone else to go through what I’ve been through with impulsive and compulsive behaviour.” Stephen, diagnosed in 2001 Dopamine dysregulation syndrome When people have the compulsion to take more medication than is needed to control their Parkinson’s symptoms this is known as dopamine dysregulation syndrome. 1 This is a type of impulsive and compulsive behaviour. If you think this is happening to you or the person you are caring for, tell your GP, specialist or Parkinson’s nurse right away. Dopamine Agonist Withdrawal Syndrome46 This happens when a person’s dopamine agonist treatment is stopped or reduced. This could be when a person is experiencing impulsive or compulsive behaviour as a side effect and needs to stop taking (or reduce the amount of) the medication causing the behaviour.46 Symptoms of dopamine agonist withdrawal syndrome can include anxiety, panic attacks, depression, insomnia, irritability and drug cravings.46 Stopping or reducing treatment should always take place in consultation with your specialist and must be done gradually. Side effects We can’t list all the possible side effects of all Parkinson’s drugs in this booklet. However, some of the most common side effects that can happen with dopamine agonists include nausea, constipation, low blood pressure (hypotension), headaches, psychological problems, hallucinations (seeing, hearing, feeling and smelling things that aren’t there) and movement problems.1,3,30 MAO–B (Monoamine oxidase type B) inhibitors47 This section explains what MAO–B inhibitors are and how they work, and looks at other considerations, including possible side effects. How MAO-B inhibitors work How MAO-B inhibitors are used Advantages of MAO-B inhibitors Disadvantages of MAO-B inhibitors Side effects 24 24 24 25 25 23 Unbranded (generic) name Brand names Forms available Rasagiline Azilect Tablets Available in unbranded form Tablets Selegiline Zelapar Tablets that dissolve on the tongue Eldepryl Tablets Taking special care with MAO–B inhibitors If you are prescribed these drugs for Parkinson’s, please make sure you read the important safety advice that comes with them, and the general information on page 10. How MAO–B inhibitors work Dopamine is a chemical messenger made in the brain. The symptoms of Parkinson’s appear when dopamine levels become too low. This is because many of the cells in your brain that produce dopamine have died or are dying.1 Unfortunately, taking dopamine as a drug treatment for Parkinson’s can’t help because it can’t cross into your brain where it’s needed.23 MAO–B inhibitors can help your nerve cells make better use of the dopamine that it does have. They do this by blocking an enzyme called monoamine oxidase type B (MAO–B), which breaks down dopamine in your brain. This helps to increase the amount of dopamine that the brain can use, which helps to relieve the symptoms of Parkinson’s. 3 How MAO–B inhibitors are used A MAO–B inhibitor can be used on its own in early Parkinson’s, or in combination with other drugs at all stages of Parkinson’s.47 These drugs are mainly available as tablets.47 There is also a form that dissolves on the tongue.47 This may help if you have trouble swallowing. Advantages of MAO–B inhibitors 24 Improving Parkinson’s symptoms On its own, an MAO–B inhibitor can help with some Parkinson’s symptoms,47 but effects are modest and may become less effective over time. Not all have to be stepped up gradually Many drug treatments for Parkinson’s have to be started gradually, with the dose slowly being increased over time. This is not the case for MAO-B inhibitors.48 Delaying levodopa treatment By taking an MAO–B inhibitor at an early stage of Parkinson’s, you may be able to delay taking levodopa until your symptoms become more difficult to manage.47 Helping levodopa work better When you have been taking levodopa for a while, you may find that its effects wear off too quickly. An MAO–B inhibitor can help with this.47 Taking an MAO–B inhibitor may also reduce the dose of levodopa you need and lengthen the time between your doses of levodopa.49 Disadvantages of MAO–B inhibitors Combination with antidepressants If you’re taking some types of antidepressant, you might not be able to take MAO–B inhibitors, as these drugs can interact with each other to raise blood pressure to a dangerous level.48 If you are taking antidepressants, your specialist should be able to advise you on how to take these alongside your Parkinson’s medication. Combination with decongestants Decongestants or cold remedies can affect some types of MAO–B inhibitors.50 If you need to use one of these products, check with your pharmacist to find out which one is safest to use. Worse levodopa side effects Because MAO–B inhibitors strengthen levodopa, the side effects of levodopa, including unwanted movements and sickness, may get worse, too.50 If this happens, your specialist or Parkinson’s nurse can help you reduce the dose of levodopa. Side effects We can’t list all the possible side effects of all Parkinson’s drugs in this booklet. However, some of the most common side effects that can happen with MAO–B inhibitors include headache, aching joints, indigestion, flu-like symptoms and depression.47 COMT (Catechol-O-methyltransferase) inhibitors51 25 This section explains what COMT inhibitors are and how they work, and looks at other considerations, including possible side effects. How COMT inhibitors work How COMT inhibitors are used Advantages of COMT inhibitors Disadvantages of COMT inhibitors Side effects 26 26 26 27 27 Unbranded (generic) name Brand names Forms available Entacapone Comtess Tablets Co-careldopa plus entacapone22 Stalevo/Sastravi Tablets Tolcapone Tasmar Tablets Taking special care with COMT inhibitors If you are prescribed these drugs for Parkinson’s, please make sure you read the important safety advice that comes with them, and the general information on page 10. How COMT inhibitors work Dopamine is a chemical messenger made in the brain. The symptoms of Parkinson’s appear when dopamine levels becomes too low. This is because many of the cells in your brain that produce dopamine have died or are dying.1 Unfortunately, taking dopamine as a drug treatment for Parkinson’s doesn’t help, because it can’t cross into your brain where it’s needed.23 However, you can boost the supply in your brain by taking levodopa, a drug that acts as a chemical building-block to help your body produce more dopamine.1 COMT inhibitors can block an enzyme that breaks down levodopa.1 How COMT inhibitors are used These drugs are used alongside levodopa, to help it work more smoothly.1 They can be tried if your dose of levodopa is not working for long enough (end-of-dose deterioration) or it ‘wears off’.51 COMT inhibitors do not help to manage Parkinson’s symptoms on their own – they have to be used with levodopa.51 COMT inhibitors come as tablets.51 If you take entacapone, you should take it at exactly the same time as your levodopa medication to get the best results.52 There is also a 26 combined tablet that includes levodopa, carbidopa (one of the ‘helper’ drugs that are always given alongside levodopa) and the COMT inhibitor entacapone. Brands include Stalevo and Sastravi (see page 13). Advantages of COMT inhibitors Helping levodopa work more smoothly COMT inhibitors can help when levodopa is not working long enough and starts to wear off between your doses.51 It can help to reduce the ‘off’ time when you have more trouble with your Parkinson’s symptoms and it can increase the amount of ‘on’ time when your symptoms are better controlled.1 Taking less levodopa In many cases, levodopa can be taken less often and at a lower dose. 53 Improving Parkinson’s symptoms Sometimes, adding a COMT inhibitor to your medication regimen may help your Parkinson’s symptoms.53 Disadvantages of COMT inhibitors Liver damage With tolcapone, there is a risk of liver damage that can be fatal. It is rare, but for this reason, it is a second choice, only used if you can’t take entacapone, where the risk of liver damage has not been seen. If you take tolcapone, you will need regular blood tests to check the health of your liver.1 Worse levodopa side effects Because COMT inhibitors strengthen levodopa, the side effects of levodopa, including unwanted movements and sickness, can get worse, too. 52 If this happens, your specialist or Parkinson’s nurse can help you reduce the dose of levodopa. Side effects51 We can’t list all the possible side effects of all Parkinson’s drugs in this booklet. However, some of the most common side effects that can happen with COMT inhibitors include sleeping problems, loss of appetite, diarrhoea, dizziness, fainting, falls, hallucinations (seeing, hearing, feeling and smelling things that aren’t there), headache, confusion, dry mouth, chest pain and sleepiness. These drugs can also discolour your urine. “Parkinson’s is a progressive condition. Medicines can help, and over the years I will take newer and stronger types. I know that some will make me feel sick and a lot of adjustments will need to be made along the way.” Keith, diagnosed in 2001 Glutamate antagonists54 27 There is only one glutamate antagonist that can be prescribed. This section explains what a glutamate antagonist is and how it works, and looks at other considerations, including possible side effects. How a glutamate agonist works How is a glutamate agonist used Advantages of a glutamate agonist Disadvantages of a glutamate agonist Side effects 28 28 28 28 28 Unbranded (generic) name Brand name Forms available Amantadine N/A Capsules, syrup Taking special care with a glutamate antagonist If you are prescribed this drug for Parkinson’s, please make sure you read the important safety advice that comes with it, and the general information on page 10. How a glutamate antagonist works It’s not known exactly how this drug works for Parkinson’s.1 It may affect how the brain reacts to certain chemicals.54 How a glutamate antagonist is used Amantadine can be used to treat tremor and stiff muscles. 55 It isn’t used very often and it is unlikely to be prescribed alone. It is usually given with other drug treatments for Parkinson’s56 and can be used at all stages of Parkinson’s.1 It is started at a lower dose and the amount is stepped up gradually.56 Amantadine is available as capsules and syrup.56 Advantages of a glutamate antagonist Fewer movement side effects The SIGN guidelines for the NHS in Scotland and the NICE guidelines for the NHS in England and Wales (which are also recommended for use in Northern Ireland), say there is not enough scientific evidence to support this drug as a first choice in early Parkinson’s.1 But for some people, amantadine may reduce dyskinesia (involuntary movements) caused by your other Parkinson’s drugs, without making your Parkinson’s symptoms worse. 1 Disadvantages of a glutamate antagonist 28 Limited effects on Parkinson’s Amantadine is not a first choice for the treatment of Parkinson’s1 and it may have only a mild effect. Over time, amantadine can become less effective.54 Blurred vision, fainting, confusion or dizziness54 If you have these side effects, it is not safe to drive or use machinery. Side effects54 We can’t list all the possible side effects of all Parkinson’s drugs in this booklet. However, some of the most common side effects that can happen with a glutamate antagonist include feeling nervous, anxious or overexcited, poor concentration, headache, hallucinations (seeing, hearing, feeling and smelling things that aren’t there), movement problems, sleep problems such as insomnia, fast or irregular heartbeat, loss of appetite, nausea and vomiting, constipation, sweating, swollen hands and ankles, and skin reactions. Anticholinergics57 This section explains what anticholinergics are and how they work, and looks at other considerations, including possible side effects. How anticholinergics work How anticholinergics are used Advantages of anticholinergics Disadvantages of anticholinergics Side effects Unbranded (generic) name 30 30 30 31 31 Brand names Forms available Biorphen Liquid Orphenadrine 29 Procyclidine Trihexyphenidyl (benzhexol) Available in unbranded form Tablets, liquid Arpicolin Syrup Kemadrin Tablets, injection Available in unbranded form Tablets Broflex58 Syrup Available in unbranded form Tablets, syrup Taking special care with anticholinergics If you are prescribed these drugs for Parkinson’s, please make sure you read the important safety advice that comes with them, and the general information on page 10. How anticholinergics work These drugs block the action of acetylcholine, a chemical messenger that is found in your brain and body. Acetylcholine helps to send messages in the brain and from your nerves to your muscles.59, 57 How anticholinergics are used These drugs are old and are not used very often for Parkinson’s today. Sometimes they are prescribed for reducing tremor and muscle stiffness.1 They can be used on their own, especially in the early stages of Parkinson’s, before levodopa is prescribed. 1 Anticholinergics can also be used with levodopa or a glutamate antagonist. 1 They are taken as tablets or as a liquid.57 Advantages of anticholinergics 30 Possible effect on mild movement symptoms Older medical studies have found some benefits from taking anticholinergics for Parkinson’s symptoms. They can be effective for younger people in the early stages of Parkinson’s.1 Possible effect on other Parkinson’s symptoms Anticholinergics may also be used to reduce saliva production if you have a problem with drooling.57 Oxybutynin is an anticholinergic that is used in people without Parkinson’s to reduce bladder contractions that can cause a strong, frequent urge to urinate. It is only used very cautiously in people with Parkinson’s as it may reduce how much levodopa your body can be absorb.60 Disadvantages of anticholinergics Limited effect on movement symptoms These drugs are not recommended in guidelines for the NHS in Scotland. The authors of these guidelines say the advantages do not outweigh the disadvantages.4 Memory problems Anticholinergics are not very often given to people with Parkinson’s because they can cause memory problems or make them worse. This can happen at any age, but particularly for older people.57 If you’re taking anticholinergics, your specialist or Parkinson’s nurse must closely monitor your situation.1 Side effects57,61 We can’t list all the possible side effects of all Parkinson’s drugs in this booklet. However, some of the most common side effects that can happen with anticholinergics include dry mouth, blurred vision, constipation, dizziness and trouble urinating, confusion, hallucinations (seeing, hearing, feeling and smelling things that aren’t there) and forgetfulness. Managing your medication If you have Parkinson’s, it is important to take your Parkinson’s medication as advised by your specialist or Parkinson’s nurse. Do not stop taking your Parkinson’s medication unless your specialist or Parkinson’s nurse tells you to.2 Taking your medication for Parkinson’s at the right time will help you to manage your symptoms better.1 Keep a chart 31 Having a written record of all your medications, including when and how you take your drugs may help you to keep track of what you take – especially if you have a complicated regimen with a number of tablets. We have free resources to help you with this, including a medication record and medication card. See page 48 for more information on how to order these. Taking it on time From using alarms on a digital watch to setting the oven timer, we hear of many tools people with Parkinson’s use to remind them to take their medication on time. The trick is to find a solution to suit you. Pill timers A pill timer is a box that you can store your Parkinson’s drugs in to remind you when to take each dose. They are useful if you have to take lots of different tablets or if you have trouble remembering to take your medication. There are many different types and sizes of pill timer. Some have sections for different times of day, so you can store all of your Parkinson’s drugs for one day. Others are big enough to hold your tablets for a whole week, with sections for each day. Some weekly pill timers are also split into times of day. When you choose a pill timer, make sure it has enough space for the number and size of the tablets you have to take. Some pill timers have labels on each section that show days or times. Others have a timer or a digital clock face with an alarm to remind you to take your medication. Pill timers vary in cost, depending on the type and who it is made by. An occupational therapist or pharmacist can help you to choose the right option. The Disabled Living Foundation, an organisation that provides information on a range of equipment for disabled and older people, can also advise you on options available. Contact them at: Disabled Living Foundation Helpline: 0300 999 0004 (10am to 4pm Mondays to Fridays) helpline@dlf.org.uk www.dlf.org.uk Help from your pharmacist If you have difficulty taking your medication, your pharmacist can arrange an assessment and see how they can help. For example, they can offer large-print labels, non ‘click top’ bottles or a medication reminder chart. Developing new drugs 32 Every drug, treatment and therapy available today is the result of a long and expensive development process.62 It starts in the lab when researchers identify a promising idea for a new treatment. These ideas must first be turned into drug-like molecules, that can then be tested in the lab to see how effective they might be and how safely they might be used. Of every 5,000 drugs initially tested, around five make the leap to clinical trials. 62 Clinical trials are the way that new treatments are tested on people. They are often sponsored by the manufacturer of a drug. Sometimes they are funded by public organisations such as the NHS or a government research council. 63 Parkinson’s UK also funds some clinical trials that examine the effects of new treatments and is committed to delivering new and improved treatments, faster. Before a trial can go ahead, it has to be approved for safety and ethics by an independent committee of experts.64 During thorough testing, researchers can understand whether a drug may work, check it is safe and understand possible side effects. Only then may a new treatment be approved and made available to the wider public. A new treatment may take more than 10 years to make its way through clinical trials.62 And only around one in five that enter clinical trials is eventually approved for use. 62 This means that clinical trials are the most costly and time-consuming part of bringing new treatments to patients, but they are crucial to ensure we get new and better treatments. Joining a clinical trial You may be invited to join a clinical trial or take part in other research studies by your specialist or Parkinson’s nurse. You can also ask your doctor if you can take part in research. Details of clinical trials and research studies are posted on the Parkinson’s UK website at parkinsons.org.uk/research, with details of who to contact for further information. Before you decide to take part in a trial or study, you should always ask for written information about it. You should also have time to talk about the pros and cons with your specialist or Parkinson’s nurse and your family before you decide whether to take part. You should never feel under any pressure to take part or to continue in a clinical trial. Saying no or leaving the trial will not affect the way you are treated – it is your right to do this and your specialist or Parkinson’s nurse will continue to do their very best for your care. 33 Clinical trials for drugs generally go through four phases:65 Phase 1 Phase 2 Phase 3 Phase 4 Healthy volunteers take the drug. In some cases, people with the condition may take part in this stage of the trial. People with the condition volunteer to take the drug. A larger number of people with the condition volunteer to take the drug – some may get a ‘dummy’ treatment. Once the drug is approved for doctors to prescribe, people with the condition volunteer for follow-up studies. Why? Assesses the safe dose, side effects and how it works in the body. Why? Studies how well the drug works, how safe it is, what an effective dose is and if there are side effects. Why? Studies safety, effectiveness and side effects over a longer period and compares the new drug to other treatments. Why? Continues to study safety and effectiveness over a longer period. What treatments are currently being developed for Parkinson’s? It can take many years before a treatment is ready to be tested in clinical trials. The following is just a small example of some of the most promising new treatments currently being explored for Parkinson’s. Drug repurposing66 Finding new uses for old drugs shows lots of promise for quickly bringing new treatments to people with Parkinson’s. As these drugs are already widely used for other conditions, we know they’re safe to use – an important element of a clinical trial. One promising example is exenatide – a drug already used by people with type 2 diabetes. Lab studies funded by Parkinson’s UK helped to show that exenatide could improve symptoms and even rescue dying nerve cells. Exenatide is being tested in people with Parkinson’s in London and the first results are expected in 2016. We are funding studies and initiatives to search for more current drugs that may have untapped potential for Parkinson’s. 34 Growth factors Growth factors are special proteins that are naturally produced inside the brain. They support the growth and survival of many types of brain cell.67 Harnessing the power of growth factors to protect or even restore the cells that are lost in Parkinson’s is an exciting prospect. Parkinson’s UK is currently funding a trial of one growth factor called GDNF, which is testing the therapy in people with Parkinson’s. We hope that our trial will show that GDNF can slow the course of Parkinson’s. Results are expected in late 2016. Gene therapy Gene therapies work by inserting genes into cells that aren’t working properly. The genes provide instructions that change the way the cells behave. 68 There are currently a number of gene therapy treatments being developed for Parkinson’s. One of these is being developed by a British company and uses three genes that help nerve cells in the brain make their own dopamine – the chemical that is lost in the brain in Parkinson’s. Vaccines Researchers are working to develop vaccines that can be used to treat Parkinson’s. The aim is that these vaccines will help the immune system to identify and remove proteins that are thought to be involved in brain cell death in Parkinson’s. It would then be able to slow or stop the development of the condition. Small trials have so far been carried out and suggest this approach is safe but more research is needed to see how effective it could be. Find out more: to keep up to date with the latest research, see the research pages on our website, parkinsons.org.uk/researchnews More information and support If you have more questions about your drug treatment, talk to your specialist or pharmacist. Parkinson’s nurses Parkinson’s nurses provide expert advice and support to people with Parkinson’s and those who care for them. They can also make contact with other health and social care professionals to make sure your needs are met. The role of the Parkinson’s nurse varies. Each will offer different services, aiming to meet local needs. Some nurses are based in the community, whereas others are based in hospital settings. Many Parkinson’s nurses are independent prescribers. This means they can prescribe and make adjustments to medication, so someone with Parkinson’s doesn’t always need to see their specialist for changes to or queries about their Parkinson’s drugs. Parkinson’s nurses may not be available in every area, but your GP or specialist can give you more details on local services. 35 You can find out more at parkinsons.org.uk/nurses Reporting a side effect The Medicines and Healthcare products Regulatory Authority (MHRA) is the government body that makes sure that drugs work and are safe. It is keen to receive feedback about medication side effects. To report a side effect, you should complete a Yellow Card form, available from your pharmacist, GP, specialist or via the Yellow Card information service (0808 100 3352). You can also complete this form online, or download and print it out from yellowcard.mhra.gov.uk Speak to your pharmacist, GP, specialist or Parkinson’s nurse if you need any help to fill in this form. You can also report any side effects from your Parkinson’s medication directly to your GP, specialist or Parkinson’s nurse. Information and support from Parkinson’s UK You can call our free confidential helpline for general support and information. Call 0808 800 0303 (calls are free from UK landlines and most mobile networks) or email hello@parkinsons.org.uk. We run a peer support service if you’d like to talk on the phone with someone affected by Parkinson’s who has faced similar issues to you. The service is free and confidential – ring the helpline to talk to someone about being matched with a volunteer. Our helpline can also put you in touch with one of our local information and support workers, who give one-to-one information and support to anyone affected by Parkinson’s. They can also provide links to local groups and services. We also have a self-management programme for people with Parkinson’s, partners and carers. It is an opportunity to reflect on life with the condition, learn about self-management and think about the future. To find out if there is a group near you visit parkinsons.org.uk/selfmanagement Our website parkinsons.org.uk has a lot of information about Parkinson’s and everyday life with the condition. You can also find details of your local support team and your nearest local group meeting at parkinsons.org.uk/localtoyou You can also visit parkinsons.org.uk/forum to speak with other people in a similar situation on our online discussion forum. More resources More information on Parkinson’s is available from Parkinson’s UK. We produce a wide range of free booklets, information sheets and cards about every aspect of living with the condition. Details of how to order resources are available on page 48. 36 Summary of drugs used to treat Parkinson’s Unbranded (generic) name Brand names Levodopa20,21 (see page 13) Levodopa is always given combined with either benserazide or carbidopa.20 It can be used at all stages of Parkinson’s.1 Co-beneldopa (benserazide plus levodopa) Available in unbranded form Madopar Madopar CR Co-careldopa (carbidopa plus levodopa) Available in unbranded form Caramet CR Duodopa Sinemet Sinemet Plus Sinemet CR Half Sinemet CR Lecado Co-careldopa plus entacapone (see page 25) Stalevo Sastravi Dopamine agonists 30 (see page 17) These drugs may be given on their own or prescribed alongside levodopa or other drugs.1 Pramipexole Available in unbranded form Mirapexin Mirapexin prolonged release (available form)form Availableininunbranded unbranded Ropinirole Rotigotine Adartrel Ralnea XL Requip Requip XL Spiroco XL Neupro 37 Apomorphine (Unlike other dopamine agonists, apomorphine is usually reserved for late Parkinson’s when symptoms are severe and levodopa is not working well all the time.)1 APO-go PEN APO-go PFS Bromocriptine Available in generic form Parlodel Cabergoline Available in generic form Cabaser Pergolide Available in unbranded form MAO–B inhibitors47 (see page 23) These drugs are sometimes used alone in early Parkinson’s, or with levodopa and sometimes other drugs, in late Parkinson’s.3 Rasagiline Azilect Selegiline Available in unbranded form Eldepryl Zelapar COMT inhibitors51 (see page 25) In late Parkinson’s, COMT inhibitors are used alongside levodopa to help it work more smoothly.1 Entacapone Comtess Stalevo Co-careldopa plus entacapone Stalevo Sastravi Tolcapone Tasmar 38 Glutamate antagonist54 (see page 27) This is usually used with other Parkinson’s medication and has an effect on tremor and stiff muscles.1,55 Amantadine N/A Anticholinergics57 (see page 29) These drugs are not used very often for Parkinson’s but sometimes they are used for reducing tremor and stiff muscles. 57,1 Orphenadrine Procyclidine Trihexyphenidyl (benzhexol) Available in unbranded form Disipal Biorphen Available in unbranded form Arpicolin Kemadrin Available in unbranded form Broflex58 Glossary Here you can find the meaning of the some of the medical and unfamiliar words used in this booklet. We have also included, in brackets, how to say the names of the most common drugs prescribed for Parkinson’s as they sound. Acetylcholine59 (AH–suh-tile-KOH-leen) A chemical messenger found in the body that sends messages between nerve cells and muscles. These messages can affect the way muscles work. Anticholinergic drugs work on acetylcholine. Amantadine56 (a–MAN–ta–deen) A glutamate antagonist only rarely prescribed to help treat tremor and stiff muscles in people with Parkinson’s. Anticholinergics57 (AN-tee-koh-lin-ER-jiks) These drugs block the action of acetylcholine, a chemical messenger that helps to send messages from your nerves to your muscles. APO-go PEN/APO-go PFS31 (A-poh–go) 39 A branded type of dopamine agonist that is given by injection or infusion pump. (Unbranded name: apomorphine). Apomorphine1 (A-poh-MOR-feen) An unbranded type of dopamine agonist given by injection or infusion pump. It is saved for more advanced Parkinson’s that does not respond as well to oral drug treatments or when most oral Parkinson’s medication becomes less effective or does not work. Arpicolin57 (AA–pee–KO-lin) A branded type of anticholinergic taken as a syrup. (Unbranded name: procyclidine). Azilect47 (A-zih-lekt) A branded type of MAO–B inhibitor taken as tablets. (Unbranded name: rasagiline). Benserazide20 (BEN-zur-a–zide) A drug given alongside levodopa to help get the levodopa into the brain where it is needed. Biorphen57 (bi–OR–fen) A branded type of anticholinergic taken as a liquid. (Unbranded name: orphenadrine). Broflex58 (BRO–fleks) A branded type of anticholinergic taken as a syrup (Unbranded name: trihexyphenidyl (benzhexol)). Bromocriptine30 (bro–mo–KRIP-teen) An unbranded form of dopamine agonist. Cabaser30 (ka-BA-suh) A branded form of dopamine agonist taken as tablets. (Unbranded name: cabergoline). Cabergoline30 (ka–BER–go– leen) An unbranded type of dopamine agonist. Caramet CR20 (KA-ra–met) A branded form of levodopa. (Unbranded name: co-careldopa). Carbidopa20 (kar–be–DOH-puh) A drug given alongside levodopa to help get the levodopa into the brain where it is needed. Co-beneldopa20 (koh–BEN–el –DOH-puh) An unbranded form of levodopa – levodopa with benserazide. It is available in the branded forms of Madopar (capsules, dispersible tablets) and Madopar CR (controlled release tablets). Co-careldopa20 (koh–KA-rul-DOH-puh) An unbranded form of levodopa – levodopa with carbidopa. It is available in unbranded form as tablets and branded as Caramet CR (controlled release tablets), Duodopa (intestinal gel), Sinemet/Sinemet Plus (both tablets), Sinemet CR (controlled release 40 tablets), Half Sinemet CR (controlled release tablets) and Lecado (prolonged release tablets. COMT inhibitors1 (KOMT in-HIH-bit-ers) Drugs which block an enzyme that breaks down levodopa. Controlled release tablets/capsules Tablets and capsules which release a drug over time, rather than all at once. Comtess51 (KOM–tess) A branded type of COMT inhibitor taken in tablet form. (Unbranded name: entacapone). Dispersible tablets This form can be mixed with water to make a drink. It takes effect more quickly than capsules because it doesn’t need to be broken down in your stomach to release the active ingredient. Dopamine (DOH–puh-meen) A chemical messenger made in the brain. It transmits messages from the brain to other parts of the body, mainly to the ones that control movement. People with Parkinson’s have less dopamine because the brain cells that make it have died or are dying. Parkinson’s symptoms are caused by this loss of dopamine. 1 Dopamine agonists30 (DOH-puh-meen-A-gu-nists) Drugs which act like dopamine to stimulate the nerves cells in the brain. Dopamine agonist withdrawal syndrome46 When someone very suddenly stops taking dopamine agonists, perhaps because they are experiencing impulsive and compulsive behaviour. It can lead to symptoms including depression, anxiety or pain. Dopamine deregulation syndrome1 Where someone with Parkinson’s takes more of their Parkinson’s medication than they are prescribed. Duodopa20 (DO-o-doh-puh) A branded type of levodopa – levodopa with carbidopa. It is a gel which is fed into the intestine with a continuous pump. It is mainly used for the treatment of advanced Parkinson’s with severe motor fluctuations. Dyskinesia4 (dis-keye-NEE-zih-uh) Involuntary or unusual movements, such as jerking, twitches or spasms. They can affect any part of the body. Dyskinesia happens because of the combination of the condition and Parkinson’s medication. It is most common in people who have been taking levodopa for many years. Their prescription often has to be adjusted to find a balance between enough medication to control the symptoms, and a dose that does not bring on too much dyskinesia. Eldepryl47 (EL-duh-pril) 41 A branded type of MAO–B inhibitor taken as tablets or as a liquid. (Unbranded name: selegiline). Entacapone51(en-TA-kuh–pone) An unbranded type of COMT inhibitor. There is only one form of entacapone that is prescribed for people with Parkinson’s. Its branded name is Comtess and its taken in tablet form. Enzyme (EN-zime) Complex proteins made by living cells, which speed up chemical reactions in the body, such as breaking down drugs. Some Parkinson’s drugs work by acting on enzymes in the body. Ergot dopamine agonists1(ER-got DOH-puh-meen-A-gu-nists) Older types of dopamine agonists that are only used to treat people with Parkinson’s if more modern, non-ergot versions do not work well. They are not prescribed as a firstchoice drug because they can increase the risk of heart problems. Ergot dopamine agonists include bromocriptine, pergolide and cabergoline. Glutamate antagonist56 (GLOO-tuh-mate AH-guh-nist) A type of drug rarely prescribed that may help with tremor and stiffness. It’s not known they work in people with Parkinson’s – it’s thought they may modify levels of certain chemicals in the brain. The only glutamate antagonist prescribed for people with Parkinson’s is Amantadine. Half Sinemet CR20 (SI-nuh-met) A brand of levodopa – levodopa with Carbidopa. The tablets are controlled release meaning they slowly release the drug over time. (Unbranded name: co-careldopa). Impulsive and compulsive behaviour Impulsive behaviour is when a person can’t resist the temptation to carry out activities that could lead them to harm themselves or others.4 Compulsive behaviour is when a person has an overwhelming drive or urge to act in a certain way, often repetitively, to reduce the worry or tension that they get from that urge.43 Intestinal gel26 (in-teh-STY-nul-JEL) This option is only suitable for a very small number of people, whose symptoms can’t be controlled with the more common forms of treatment. The drug is pumped continuously through a tube that is surgically inserted into the intestine (See Duodopa) . Kemadrin57 (KEH-muh-drin) A branded type of anticholinergic, which is taken as tablets or given as injections (Unbranded name: procyclidine). Lecado20 (LEH–kah–doh) A brand of levodopa – levodopa with carbidopa. The tablets are prolonged release meaning they slowly release the drug over time. (Unbranded name: co-careldopa). Levodopa20 (LEE-vuh-DOH-puh) 42 Levodopa is one of the main ways of treating Parkinson’s and has been used since the 1960s. It is a chemical building-block that your body converts into dopamine – it replaces the dopamine that is lost in Parkinson’s. Levodopa is always given combined with either benserazide or carbidopa. These help the levodopa get into the brain where it’s needed. Madopar/Madopar CR20 (MAH-doh-par) A brand of levodopa – levodopa with benserazide. Madopar is taken as capsules or as dispersible tablets. The tablets for Madopar CR are controlled release meaning they slowly release the drug over time. (Unbranded name: co-beneldopa). MAO–B inhibitors47 (MAU-bee-in-HIH-bi-tuz) MAO–B inhibitors are drugs that can help your nerve cells to make better use of the dopamine that they have. They do this by blocking an enzyme called monoamine oxidase type B (MAO–B), which breaks down dopamine in your brain. This helps to increase the amount of dopamine that the brain can use, which helps to relieve the symptoms of Parkinson’s.3 Mirapexin/Mirapexin prolonged release30 (MIH-ruh-pek-sin) A branded form of dopamine agonist taken as tablets. (Unbranded name: pramipexol). Neupro30 (NEW-pro) A branded type of dopamine agonist. It comes as a skin patch that is held in place for 30 seconds, but it is left on for 24 hours. Non-ergot dopamine agonists30 (non-ER-gut-DOH-puh-meen AH-gu-nists) Newer types of dopamine agonists that aren’t associated with an increased risk of heart damage, unlike the older, ergot dopamine agonists. Non-ergot versions are preferred for treatment for Parkinson’s. The unbranded names of these drugs are apomorphine, pramipexole, ropinirole and rotigotine. Non-motor symptoms1 Symptoms of Parkinson’s that aren’t related to movement, for example, constipation, fatigue or depression. ‘On/off’3 Describes changes in the ability to move, which happens in some people with longstanding Parkinson’s who take levodopa. In the ‘on’ state, the person can move, while in the ‘off’ state they can stop moving altogether. People can switch from one state to the other in minutes. Orphenadrine57 (or-FEN-ah-dreen) An unbranded type of anticholinergic. It is available in unbranded form as a tablet or liquid or branded as Disipal (tablets) or Biorphen (liquid). Oxybutynin60 (OK-sih-BEW-tin) Oxybutynin is an anticholinergic that is used in people without Parkinson’s to reduce bladder contractions that can cause a strong, frequent urge to urinate. It is only used very cautiously in people with Parkinson’s as it may reduce how much levodopa your body can absorb. Parlodel30 (PAR-luh-del) 43 A branded type of dopamine agonist taken as tablets or capsules. (Unbranded name: bromocriptine). Pergolide30 (PER-guh-lied) An unbranded type of dopamine agonist taken as tablets. (No branded versions available). Pramipexole30 (PRA-me-PEK-sol) An unbranded type of dopamine agonist. It is available in unbranded form as tablets and branded as Mirapexin (tablets) and Mirapexin prolonged release (tablets). Procyclidine57 (pro–SIGH-klih-deen) An unbranded form of anticholinergic available in unbranded form as tablets. In branded form it is available as Arpicolin (syrup) and Kemadrin (tablet and injection). Prolonged release (tablets/capsules) Tablets and capsules which release a drug over time, rather than all at once. Ralnea XL30 (RAL–nee– a) A branded type of dopamine agonist given as prolonged released tablets. (Unbranded name: ropinirole). Rasagiline47 (ra-SAH-ji-leen) An unbranded form of MAO–B inhibitor taken as tablets. These can, unusually, be taken at full dose straight away. Rasagiline is only available under the brand Azilect. Requip/Requip XL30 (RE–kwip) Requip is a branded form of dopamine agonist taken as tablets. Requip XL comes as prolonged release tablets. (Unbranded name: Ropinirole). Ropinirole30 (roh-PIH-nih-roll) An unbranded form of dopamine agonist. It is available in unbranded form as tablets as well as branded as Adartrel (tablets), Eppinex XL (prolonged release) Ralnea XL (prolonged release tablets), Requip (tablets), Requip XL (prolonged release tablets) and Spiroco XL (prolonged release tablets). Rotigotine30 (ra-TIH-goh-teen) An unbranded form of dopamine agonist. It is available as the Nuepro-branded skin patch. Selegiline47 (seh-LEH-ji-leen) An unbranded form of MAO–B inhibitor available in unbranded form as tablets. Also available branded as Eldepryl (tablets and liquid) and Zelapar (tablets that dissolve on the tongue). Sinemet/Sinemet CR/Sinemet Plus20 (SIH-nuh-met) A brand of levodopa – levodopa with carbidopa – available in several forms. Sinemet and Sinemet come as tablets and Sinemet CR is taken as controlled release tablets. (Unbranded name: co-careldopa). 44 Skin patch An adhesive (sticky) patch that is put on the skin and gradually delivers medication into the body. Dopamine agonist patches are used to treat people with Parkinson’s (See Neurpro and Rotigotine). Spiroco XL30 (SPY-roh-koh) A branded type of dopamine agonist available as prolonged release tablets. (Unbranded name: ropinirole). Stalevo22 (sta-LE-voe) A branded drug made up of levodopa (co-careldopa) and the COMT inhibitor entacapone. (Unbranded name: co-careldopa plus entacapone). Tasmar51 (TAZ–mar) A branded form of COMT inhibitor taken as tablets. (Unbranded form: tolcapone). Tolcapone51 (TOLL-kuh-pone) An unbranded type of COMT-inhibitor. It is available in the branded form of Tasmar (tablets). Trihexyphenidyl57 (Benzhexol) (try–HEK-see-fen-ee-dill) An unbranded type of anticholinergic. Available in unbranded form as tablets or syrup and as the branded Broflex (syrup). Unbranded (generic name) (jeh-NEH-rik) All types of drug have a common or generic name. Every drug that has the same active ingredient will have this name, no matter who it is made by. Withdrawal syndrome Research has shown that withdrawal symptoms can happen when someone stops taking Parkinson’s medication very suddenly, perhaps because they are experiencing impulsive and compulsive behaviour.46 It can lead to symptoms including depression, anxiety or pain. Any withdrawal from Parkinson’s drugs needs to be done gradually, under the supervision of a health professional, to avoid the risk of developing this syndrome. ‘Wearing-off’4 An effect experienced by many people who have been taking Parkinson’s drugs for some time. The dose does not work for as long as it used to and the beneficial effects wear off before it is time to take the next dose. Zelapar47 (ZEH-luh-par) An branded type of MAO inhibitor. It comes as tablets that dissolve on the tongue. (Unbranded name: selegiline). 45 Non-motor symptoms questionnaire69 Assessing the full range of Parkinson’s symptoms – especially those not related to movement – can be difficult. It may be helpful to fill in this questionnaire. This questionnaire should be completed and given to your GP, specialist or Parkinson’s nurse at your next appointment. Please do not return it to Parkinson’s UK. Thank you. 1 Dribbling of saliva during the daytime. □ 2 Loss or change in your ability to taste or smell. □ 3 Difficulty swallowing food or drink or problems with choking. □ 4 Vomiting or feelings of sickness (nausea). □ 5 Constipation (less than three bowel movements a week) or having to strain to pass a stool. □ 6 Bowel (faecal) incontinence. □ 7 Feeling that your bowel emptying is incomplete after having been to the toilet. □ 8 A sense of urgency to pass urine makes you rush to the toilet. □ 9 Getting up regularly at night to pass urine. □ 10 Unexplained pains (not due to known conditions such as arthritis). □ 11 Unexplained change in weight (not due to change in diet). □ 12 Problems remembering things that have happened recently or forgetting to do things. □ 13 Loss of interest in what is happening around you or in doing things. □ 14 Seeing or hearing things that you know or are told are not there. □ 15 Difficulty concentrating or staying focused. □ 16 Feeling sad, ‘low’ or ‘blue’. □ 17 Feeling anxious, frightened or panicky. □ 18 Feeling less interested in sex or more interested in sex. □ 19 Finding it difficult to have sex when you try. □ 20 Feeling light-headed, dizzy or weak standing from sitting or lying. □ 21 Falling. □ 22 Finding it difficult to stay awake during activities such as working, driving or eating. □ 23 Difficulty getting to sleep at night or staying asleep at night. □ 24 Intense, vivid or frightening dreams. □ 46 25 Talking or moving about in your sleep, as if you are ‘acting out’ □ a dream. 26 Unpleasant sensations in your legs at night or while resting, and a feeling that you need to move. □ 27 Swelling of the legs. □ 28 Excessive sweating. □ 29 Double vision. □ 30 Believing things are happening to you that other people say are not. □ You can also download a copy of this questionnaire at parkinsons.org.uk/publications 47 Thank you to everyone who contributed to and reviewed this booklet: Uzma Chaudhry, Pharmacist, Oxford University Hospitals NHS Trust Tom Foltynie, Senior Lecturer and Honorary Consultant Neurologist in Movement Disorders, University College London Paul Hughes, Senior Pharmaceutical Advisor, NHS Kernow Clinical Commissioning Group, Cornwall Lucy Partington, Movement Disorders Nurse Specialist, Salford Royal Hospital, Greater Manchester Thanks also to our information review group and other people affected by Parkinson’s who provided feedback. Parkinson’s UK makes every effort to make sure that its services provide up-to-date, unbiased and accurate information. We hope that this will add to any professional advice you have had and will help you to make any decisions you may face. Please do continue to talk to your health and social care team if you are worried about any aspect of living with Parkinson’s. How to order our resources 0845 121 2354 resources@parkinsons.org.uk Download them from our website at parkinsons.org.uk/publications Can you help? At Parkinson’s UK, we are totally dependent on donations from individuals and organisations to fund the work that we do. There are many ways that you can help us to support people with Parkinson’s. If you would like to get involved, please contact our Supporter Services team on 020 7932 1303 or visit our website at parkinsons.org.uk/support. Thank you. 48 Every hour, someone in the UK is told they have Parkinson’s. Because we’re here, no one has to face Parkinson’s alone. We bring people with Parkinson’s, their carers and families together via our network of local groups, our website and free confidential helpline. Specialist nurses, our supporters and staff provide information and training on every aspect of Parkinson’s. As the UK’s Parkinson’s support and research charity we’re leading the work to find a cure, and we’re closer than ever. We also campaign to change attitudes and demand better services. Our work is totally dependent on donations. Help us to find a cure and improve life for everyone affected by Parkinson’s. Parkinson’s UK Free confidential helpline 0808 800 0303 (Monday to Friday 9am–7pm, Saturday 10am–2pm). Interpreting available. Text Relay 18001 0808 800 0303 (for textphone users only) hello@parkinsons.org.uk parkinsons.org.uk Last updated August 2015. Next update available August 2017. © Parkinson’s UK, August 2015. Parkinson’s UK is the operating name of the Parkinson’s Disease Society of the United Kingdom. A charity registered in England and Wales (258197) and in Scotland (SC037554). 49 Drug treatments for Parkinson’s (2015) If you have comments or suggestions about this information sheet, we’d love to hear from you. This will help us ensure that we are providing as good a service as possible. We’d be very grateful if you could complete this form and return it to Resources and Diversity, Parkinson’s UK, 215 Vauxhall Bridge Road, London SW1V 1EJ. Or you can email us at publications@parkinsons.org.uk. Thanks! Please tick.. I have Parkinson’s. When were you diagnosed? ……………………………………………………... I’m family/a friend/a carer of someone with Parkinson’s I’m a professional working with people with Parkinson’s Where did you get this information sheet from? GP, specialist or Parkinson’s nurse Information and support worker Parkinson’s UK local group or event Ordered from us directly Our website Other How useful have you found the information sheet? (1 is not useful, 4 is very useful) 1 2 3 4 Have you found the publication easy to read/use? Yes No Has this resource given you information that might help you manage your condition better? NA It hasn’t helped It has helped a little It has helped a lot What aspects did you find most helpful?.............................................................................................. …………………………………………………………………………………………………………… Were you looking for any information that wasn’t ……... covered?................................................................. …………………………………………………………………………………………………………… Do you have any other …….. comments?..................................................................................................... …………………………………………………………………………………………………………… If you would like to become a member of Parkinson’s UK, or are interested in joining our …….. information review group, please complete the details below and we’ll be in touch. Membership Information review group (People affected by Parkinson’s who give us feedback on new and updated resources) Name…………………………………………………………………………………………………… …….. Address………………………………………………………………………………………………… …….. Telephone………………………………………… Email………………………………………………….. What is your ethnic background? Asian or Asian British Chinese Black or Black British Mixed White British White other Other (please specify) ..................................... B013 50 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. National Institute of Health & Clinical Excellence. Parkinson’s disease: National clinical guideline of diagnosis and management in primary and secondary care (2006) http://guidance.nice.org.uk/CG35/Guidance/pdf/English [Accessed: January 2014] CKS Parkinson’s disease - Role of primary care (2009) http://cks.nice.org.uk/parkinsons-disease#!scenariorecommendation:1 [Accessed: March 2014] Choices N (2014) 'Parkinson’s disease - Treatment' http://www.nhs.uk/Conditions/Parkinsons-disease/Pages/Treatment.aspx [Accessed: April 2014] Scottish Intercollegiate Guidelines Network: Diagnosis and pharmacological management of Parkinson’s disease (2009) http://www.sign.ac.uk/pdf/sign113.pdf [Accessed: February 2014] CKS Parkinson’s disease - Worsening motor symptoms and motor complications (2009) http://cks.nice.org.uk/parkinsons-disease#!scenariorecommendation:3 [Accessed: March 2014] Choices N (2014) 'Parkinson’s disease - Symptoms' http://www.nhs.uk/CONDITIONS/PARKINSONS-DISEASE/Pages/Symptoms.aspx [Accessed: March 2014] CKS Parkinson’s disease - Advice about driving http://cks.nice.org.uk/parkinsonsdisease#!scenariorecommendation:2 [Accessed: July 2015] Choices N (2013) 'Low blood pressure (hypotension) - Symptoms' http://www.nhs.uk/Conditions/Blood-pressure-(low)/Pages/Symptoms.aspx [Accessed: February 2014] Averbeck BB & O’Sullivan SS et al. (2014) 'Impulsive and compulsive behaviors in Parkinson’s disease.' Annu Rev Clin Psychol; 10:553–80 CKS Parkinson’s disease - Drugs to avoid (2009) http://cks.nice.org.uk/parkinsonsdisease#!scenariorecommendation:28 [Accessed: March 2014] Sakakibara R & Uchiyama T et al. (2008) 'Bladder and bowel dysfunction in Parkinson’s disease.' J Neural Transm; 115:443–60 St John’s Wort: British National Formulary http://www.medicinescomplete.com/mc/bnf/current/bnf_int905-st-johns-wort.htm [Accessed: March 2014] CKS Parkinson’s disease - Differential diagnosis (2009) http://cks.nice.org.uk/parkinsons-disease#!diagnosissub:1 [Accessed: March 2014] CKS Parkinson’s disease - Nausea and vomiting (2009) http://cks.nice.org.uk/parkinsons-disease#!scenariorecommendation:13 [Accessed: March 2014] Choices N (2014) 'Coronary heart disease - Diagnosis' http://www.nhs.uk/conditions/coronary-heart-disease/pages/diagnosis.aspx [Accessed: May 2015] Motilium®: British National Formulary (2015) https://www.medicinescomplete.com/mc/bnf/current/PHP2546motilium.htm?q=domperidone&t=search&ss=text&p=4#PHP2546-motilium [Accessed: May 2015] Valoid®: British National Formulary (2015) https://www.medicinescomplete.com/mc/bnf/current/PHP2523- 51 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. valoid.htm?q=valoid&t=search&ss=text&p=1#PHP2523-valoid [Accessed: February 2015] Ondansetron: British National Formulary (2014) https://www.medicinescomplete.com/mc/bnf/current/PHP2562-ondansetron-nonproprietary.htm?q=ondansetron&t=search&ss=text&p=1#PHP2562-ondansetronnon-proprietary [Accessed: September 2014] Choices N (2014) 'Medicines information - brand names and generics' http://www.nhs.uk/Conditions/Medicinesinfo/Pages/brandnamesandgenerics.aspx [Accessed: March 2014] Levodopa: British National Formulary (2014) http://www.medicinescomplete.com/mc/bnf/current/PHP3089-levodopa.htm [Accessed: March 2014] SPC Lecado 100/25 mg Modified-release Tablets https://www.medicines.org.uk/emc/medicine/22548 [Accessed: July 2015] Stalevo®: British National Formulary https://www.medicinescomplete.com/mc/bnf/current/PHP3109stalevo.htm?q=stalevo&t=search&ss=text&p=1#PHP3109-stalevo [Accessed: July 2015] Garbayo E & Ansorena E et al. (2013) 'Drug development in Parkinson’s disease: from emerging molecules to innovative drug delivery systems.' Maturitas; 76:272–8 Katzenschlager R & Lees AJ (2002) 'Treatment of Parkinson’s disease: levodopa as the first choice.' J Neurol; 249 Suppl :II19–24 Fahn S (2005) 'Does levodopa slow or hasten the rate of progression of Parkinson’s disease?' J Neurol; 252 Suppl :IV37–IV42 eMC - SPC for Duodopa intestinal gel (2013) http://www.medicines.org.uk/emc/medicine/20786/SPC/Duodopa+intestinal+gel/ [Accessed: February 2014] Cereda E & Barichella M et al. (2010) 'Low-protein and protein-redistribution diets for Parkinson’s disease patients with motor fluctuations: a systematic review.' Mov Disord; 25:2021–34 Barichella M & Cereda E et al. (2009) 'Major nutritional issues in the management of Parkinson’s disease.' Mov Disord; 24:1881–92 Chaudhuri KR & Schapira AH V (2009) 'Non-motor symptoms of Parkinson’s disease: dopaminergic pathophysiology and treatment.' Lancet Neurol; 8:464–74 British National Formulary - Dopamine-receptor agonists (2014) http://www.medicinescomplete.com/mc/bnf/current/PHP3057-dopamine-receptoragonists.htm [Accessed: February 2014] British National Formulary: APO-go® (2014) http://www.medicinescomplete.com/mc/bnf/current/PHP3065-apo-go.htm [Accessed: February 2014] Mirapexin® Prolonged Release: British National Formulary (2014) http://www.medicinescomplete.com/mc/bnf/current/PHP3079-mirapexin-prolongedrelease.htm#PHP3079-mirapexin-prolonged-release [Accessed: March 2014] Neupro®: British National Formulary http://www.medicinescomplete.com/mc/bnf/current/PHP3088-neupro.htm#PHP3088neupro [Accessed: March 2014] eMC - SPC for transdermal patch (2013) http://www.medicines.org.uk/emc/medicine/27412/SPC/Neupro+2mg+24h+,+4mg+2 4h+,+6mg+24h+,+8mg+24h+Transdermal+patch-Parkinsons+disease/ [Accessed: February 2014] 52 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. CKS Parkinson’s disease - Apomorphine (2009) http://cks.nice.org.uk/parkinsonsdisease#!scenariorecommendation:36 [Accessed: February 2014] eMC - SPC for APO-go pen solution for injection (2013) http://www.medicines.org.uk/emc/medicine/12941/SPC/APOgo+Pen+10mg+ml+Solution+for+Injection [Accessed: February 2014] Gunzler SA (2009) 'Apomorphine in the treatment of Parkinson disease and other movement disorders.' Expert Opin Pharmacother; 10:1027–38 eMC - SPC for APO-go solution for infusion in pre-filled syringe (2013) http://www.medicines.org.uk/emc/medicine/15992/SPC/APOgo+PFS+5mg+ml+Solution+for+Infusion+in+Pre-filled+Syringe/ [Accessed: February 2014] Henriksen T (2014) 'Clinical insights into use of apomorphine in Parkinson’s disease: tools for clinicians.' Neurodegener Dis Manag; 4:271–82 APO-go Apomorphine FAQs (2015) http://www.apo-go.asia/faqs.html [Accessed: July 2015] Lees A & Turner K (2002) 'Apomorphine for Parkinson’s Disease' Pract Neurol; 2:280–287 Maass A & Reichmann H (2013) 'Sleep and non-motor symptoms in Parkinson’s disease.' J Neural Transm; 120:565–9 Choices N (2012) 'Obsessive compulsive disorder (OCD) - Symptoms' http://www.nhs.uk/Conditions/Obsessive-compulsivedisorder/Pages/Symptoms.aspx [Accessed: April 2014] Antonini A & Cilia R (2009) 'Behavioural adverse effects of dopaminergic treatments in Parkinson’s disease: incidence, neurobiological basis, management and prevention.' Drug Saf; 32:475–88 Weintraub D & Koester J et al. (2010) 'Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients.' Arch Neurol; 67:589–95 Nirenberg MJ (2013) 'Dopamine agonist withdrawal syndrome: implications for patient care.' Drugs Aging; 30:587–92 Monoamine-oxidase-B inhibitors: British National Formulary http://www.medicinescomplete.com/mc/bnf/current/PHP3113-monoamine-oxidase-binhibitors.htm [Accessed: March 2014] RASAGILINE: British National Formulary (2014) http://www.medicinescomplete.com/mc/bnf/current/PHP3114-rasagiline.htm [Accessed: March 2014] Pagonabarraga J & Rodríguez-Oroz MC (2013) '[Rasagiline in monotherapy in patients with early stages of Parkinson’s disease and in combined and adjunct therapy to levodopa with moderate and advanced stages].' Rev Neurol; 56:25–34 Azilect 1 mg Tablets - Summary of Product Characteristics (SPC) - (eMC) http://www.medicines.org.uk/emc/medicine/16273/SPC/Azilect+1+mg+Tablets/#PR ODUCTINFO [Accessed: March 2014] Catechol-O-methyltransferase inhibitors: British National Formulary http://www.medicinescomplete.com/mc/bnf/current/PHP3121-catechol-omethyltransferase-inhibitors.htm [Accessed: March 2014] ENTACAPONE: British National Formulary http://www.medicinescomplete.com/mc/bnf/current/PHP3122-entacapone.htm [Accessed: March 2014] Gershanik OS (2015) 'Improving L-dopa therapy: the development of enzyme inhibitors.' Mov Disord; 30:103–13 53 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. Symmetrel Capsules - Summary of Product Characteristics (SPC) - (eMC) http://www.medicines.org.uk/emc/medicine/4358/SPC/Symmetrel+Capsules/ [Accessed: March 2014] PIL Symmetrel Capsules - eMC (2011) https://www.medicines.org.uk/emc/medicine/3195 [Accessed: July 2015] Amantadine: British National Formulary http://www.medicinescomplete.com/mc/bnf/current/PHP3126-amantadine.htm [Accessed: March 2014] 4.9.2 Antimuscarinic drugs used in parkinsonism: British National Formulary http://www.medicinescomplete.com/mc/bnf/current/PHP3134-antimuscarinic-drugsused-in-parkinsonism.htm [Accessed: March 2014] PIL Broflex (2009) http://xpil.medicines.org.uk/fileserver.aspx?file=11898/current/resources/64864.pdf Shirahata M & Balbir A et al. (2007) 'Role of acetylcholine in neurotransmission of the carotid body.' Respir Physiol Neurobiol; 157:93–105 OXYBUTYNIN HYDROCHLORIDE: British National Formulary http://www.medicinescomplete.com/mc/bnf/current/PHP5086-oxybutyninhydrochloride.htm?q=Oxybutynin&t=search&ss=text&p=1#_hit [Accessed: March 2014] Arpicolin Procyclidine Hydrochloride Syrup 2.5mg/5ml - Summary of Product Characteristics (SPC) - (eMC) http://www.medicines.org.uk/emc/medicine/8069/SPC/Arpicolin+Procyclidine+Hydro chloride+Syrup+2.5mg+5ml/#UNDESIRABLE_EFFECTS [Accessed: March 2014] Urbig D & Burger R et al. (2011) 'Investor Reactions to New Product Development Failures: The Moderating Role of Product Development Stage' J Manage; 39:985– 1015 Hudson J & Khazragui HF (2013) 'Into the valley of death: research to innovation.' Drug Discov Today; 18:610–3 Meinert CL (2012) 'ClinicalTrials: Design, Conduct and Analysis' (Oxford University Press, USA); 720 https://books.google.com/books?hl=en&lr=&id=Y1NpAgAAQBAJ&pgis=1 [Accessed: July 2015] Choices N (2015) 'Clinical trials and medical research - Phases of trials' http://www.nhs.uk/Conditions/Clinical-trials/Pages/Phasesoftrials.aspx [Accessed: March 2014] Barker RA & Stacy M et al. (2013) 'A new approach to disease-modifying drug trials in Parkinson’s disease.' J Clin Invest; 123:2364–5 Arámburo C & Alba-Betancourt C et al. (2014) 'Expression and function of growth hormone in the nervous system: a brief review.' Gen Comp Endocrinol; 203:35–42 Genes and Gene Therapy (2014) Medlin Plus http://www.nlm.nih.gov/medlineplus/genesandgenetherapy.html [Accessed: May 2015] Chaudhuri KR & Martinez-Martin P et al. (2006) 'International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study.' Mov Disord; 21:916–23 54