5year_nih - De Montfort University
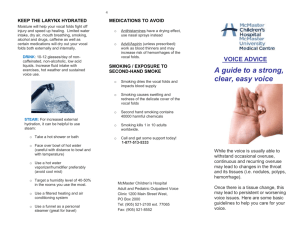
advertisement

Introduction to Revised Application The project investigators have carefully considered the study section reviewers’ critiques. Reviews by the 5 experts were thoughtful and comprehensive, and we have incorporated their ideas into this resubmission. We are grateful for the many positive comments noted in the reviews. The strengths of the original proposal, as cited in the reviews, have been maintained in our revised application. These strengths include: 1) the highly innovative work proposed in Aims #1 and #2, 2) the highly-qualified, excellent collaborative team with complementary skills, 3) a research environment that is wellsuited to the proposed work, and 4) proposed studies that capitalize on the foundation laid by the productive record of the investigators. The most substantive changes in this grant application are a reduction in scope, clarification of productivity and use of animals/experiment. Most importantly all 5 reviewers suggested that the original proposal was overly ambitious and the clinical arm (Aim 3) was not sufficiently well developed. The clinical arm of the original proposal has been eliminated to enable the project investigators to more carefully focus on the other aims. It is our impression that this reduction in proposed work takes care of most of questions raised in the critiques. Based on the initial 5 years of funding we are confident we can accomplish the remaining aims. Responses to critiques not concerned with the clinical study or ambitiousness are addressed below: Critique #1 No timeline provided & needed for clinical studies. No clinical studies but timeline now included. Critique #3 The physical model described in section C.1.2 and D.2.2.1 was borrowed by the subcontractor. In the former Section C.1.2, we tried to explain that because of limitations of the original physical model proposed, we chose to focus our efforts on other aspects of scarring not included in the original proposal, including the determination of appropriate scaffolds, cells and growth factors to regenerate the scarred vocal fold, as well as an examination of their therapeutic effects.” In particular, we explained that “in the previous physical model of the vocal fold mucosa (Titze et al, 1995; Chan et al., 1997), the epithelium was made of silicone, and the superficial layer of the lamina propria was made of water.” Accordingly, “in that model, it was not possible for the scar to extend further into the vocal fold tissues than the epithelium. Thus, it was not possible to duplicate conditions commonly seen in the clinic, or the conditions previously studied in the finite element model. However, in the new physical model (Thomson, 2004), the scar can extend much further into the vocal fold mucosa, allowing us to simulate scarring conditions observed clinically, and conditions previously tested in the finite element model.” [Quotes are from previously reviewed grant submission]. Also, in the former section C.1.2., our intent was to propose the revival of the physical model component of the grant using a new physical model supplied to Dr. Berry by the author (Thomson, 2004). However, in his most recent peer-reviewed journal article [Thomson, S.L., Mongeau, L., Frankel, H.F. (2005). Aerodynamic transfer of energy to the vocal folds, J. Acoust. Soc. Am. 118, 1689-1700] on page 1695, Dr. Thomson publicly acknowledges the work of Dr. Berry’s laboratory at UCLA in adapting his physical model for other investigations: “ In the above-referenced paper the physical model was constructed independently in Dr. Berry’s laboratory. While the reviewer is correct that the “creation” of such a physical model is not a “trivial” task, Dr. Berry has been perfecting these procedures for over a year. Several intricate aspects regarding the successful construction of the physical model have included (1) complete mixing of the various elements using a specialized shaker, (2) a low-pressure vacuum chamber to degas and prevent the formation of bubbles, and (3) post-curing of the “folds” in a heated oven. While Dr. Thomson is actively pursuing advanced body/cover adaptations of his physical model, he is well aware of Berry’s adaptations of the model for vocal fold scarring. Dr. Thomson and Dr. Berry are in frequent contact with each other, have a collegial relationship, and frequently exchange ideas on laryngeal modeling. To include both of them as consultants on the same research proposal would be unnecessary. The proposed procedural adaptations of the model for vocal fold scarring, while difficult if not impossible for the Titze/Chan physical model (because the superficial layer of the lamina propria is a liquid), are relatively straight forward for the Thomson physical model. Proposal states that a gap size of 1mm will be used. The unit is wrong and should read 0.1 -300 rad/s (corresponding to 0.016 - 48 Hz). The gap size was 1mm for our earlier work involving normal scarred tissue over this same frequency range ( Rousseau et al,2003) . Data was analyzed by Roger Chan. For the proposed work the gap will be varied to account for the desired force Not clear that cellular work presented in D.1.6.1 and C.2.3 covers significant new territory compared to work by Verdolini in Pittsburgh or Thibeault in Utah Our systematic approach to using growth factors, gene therapy ,functional outcomes ,development of a rat model are novel approaches and make unique contributions on an important topic. Dr. Susan Thibeault has joined our group as a consultant, read the grant proposal and concurs with our assessment. A letter of support is included with document. The linear skin Rheometer does not yield absolute numbers. The correlation of the relative numbers to absolute numbers should be clarified. The LSR is a precision electro-mechanical device designed to specifically measure the visco-elastic properties of human and animal tissue. The design is such that it can be very flexibly applied, and configured in different ways to obtain data by five different methods. Two of these techniques have been applied to excised human larynxes by Hess and Goodyer, and yield similar values and will be used in our studies. The figure and conversion factor from dynamic spring rate to viscosity (antipoise) is detailed in our latest manuscript included in the Appendix (Dailey, Welham et al. Submitted 2005). Shear properties are measured by attaching a 'probe' to the chuck which is attached to the tissue under test. The micro-positioner can then stress the tissue in the shear mode in a methodical manner (typically by applying a sinusoidal force cycle). The force and displacement sensors capture the absolute stress & strain data from which shear modulus is derived. The raw data is expressed in terms of Dynamic Spring Rate, which is the complex term made up of the Elastic Spring Rate and the viscous Loss Rate. Using the usual mathematical transformations, based on the geometry of the test set-up (i.e. tissue thickness and probe attachment area) the complex shear modulus term can be derived. It is also possible to resolve out the elastic and viscous modulii, as the instrument calculates the phase angle of the between the sinusoidal force and resultant position cycles. The indentometer approach is to derive a stress/strain characteristic by logging the change in force as the tissue is compressed. Shear modulus can be derived from this data by applying the mathematical transformation derived by Hayes in the 1970's. This methodology was developed specifically to determine the shear modulus from indentometer data obtained from soft tissue, and is widely used by many researchers today. The raw data takes the form of a classic indentometer stress/strain curve, which shows hysteresis when there is a viscous element to the tissue characteristics. The Hayes solution requires knowledge of the Poisson's ratio and the thickness of the tissue. As soft human tissue is highly incompressible its' Poisson's ratio is usually estimated to lie between 0.45 and 0.49, tissue thickness can be measured empirically. Therefore it is possible to derive absolute values for shear modulus. It should be clarified why growth factors are used instead of a mechanical environment like a bioreactor. Cells are affected by various factors such as transcription factors, growth factors, and microenvironment surrounding cells including mechanical stress. Titze proposed a bioreactor for engineering vocal fold tissue and indicated that vibratory strain alters the expression levels of extracellular matrix-related genes. Influence of mechanical stress on cell character is already reported in other organs, such as bladder wall and tendon, in which cells are exposed to mechanical stress and it is reasonable that fibroblasts in vocal folds are affected by mechanical stress as well. Nevertheless, we believe growth factors are the strongest tool for engineering vocal fold tissues. Various kinds of growth factors have been identified and the functions of each growth factor have been documented. The great advantage of growth factors is each growth factor has different function which enables one to control cell characteristics more precisely and abundant knowledge has been established in growth factors although there is a lot still unknown. The knowledge makes it easier to tune cells. For example, numerous growth factors have been used to differentiate stem cells to desired cells. Thus, we believe growth factor is an ideal tool to tune vocal fold fibroblasts. D.1.8.2 discusses software but there appears no reference or source of software and its availability. References are provided for the source of analysis software. At this time neither the Yan GAW or Jiang software are commercially available. The budget for year 5 lists “supplies” and “other expenses” as continuing from previous years. One should be less since year 5 should not contain much in terms of laboratory work but more analysis and publication preparation We do not anticipate stopping data collection or increased analysis during the 5th year of the project. We presume we will continue with a steady program of data collection, analysis and publication throughout the period of funding. This is absolutely critical in an integrated multidisciplinary project that uses the results of studies to formulate hypotheses in the other related areas such as we do in relating one type of model to another. Critique #5 It is not clear if excised rat larynges can be phonated. Given the small size of the structure, some feasibility data on this should be provided. Feasibility data is provided in D.1.7. Movement of rat vocal folds are visualized with creative optics using a microscope and high speed camera. Movement is best visualized in movie pictures (i.e. AVI format). AVI movies of normal and scarred rat larynges can be provided if requested. No figures or tables were used in this or any of the reports. No figures are provided to demonstrate the LSR map Figures and tables have been added to illustrate work completed and feasibility of proposed studies. The application implies that the investigators tried a variety of animal models during the initial project period but now are mainly using rats. This is likely for cost reasons. It is true that cost is an important issue, but it is not the main reason why we’ve shifted toward rats from bigger animals. Rats appear to have advantages compared to dogs and rabbits. The vocal fold lamina propria of rats displays characteristics similar to that of humans. Like the human, the rat LP has 3 layers with the deep layer containing more collagen fibers than the superficial layer. In contrast the fibrous components are denser in the superficial layer than in the deep layer in dogs LP. Also, rats can be expected to show quicker wound healing because of their short life span. In using dog and rabbit models, 6-month postoperative time frame was necessary for a vocal fold scar to mature whereas rats need only 2 months. This is a great advantage in conducting our research because we can address more questions and have longer term follow-up in a shorter time frame. Another rationale for focusing on rats is that there is an abundance of genetic information available. Moreover numerous basic scientific techniques, especially in molecular biology, are already established in rats. The availability of genetic information and developed techniques provide a short cut allowing us to focus on specific molecules in a timely fashion. Thus, rats appear to be an ideal model for investigation of wound healing in the vocal folds as further described under justified use of vertebrate animals. With regard to Aim 2, the relation of the aging rat vocal fold model studies from the preliminary studies to the overall goal of scar prevention and treatment and the proposed experiments is not explained. Three factors have motivated us to include life-span studies including the aging rat : 1) Fetal wound healing is known to do so scarlessly; 2) Cellular structure of the vocal fold is known to change across the life span but characteristics and regulatory agents are not well understood, and 3) Histological characteristics of aged and scarred vocal folds are similar. The ultimate goal of treating vocal fold scarring is to reconstruct healthy tissue. In this regard, there is a great deal of knowledge to be gained from studying the processes by which fetal and neonatal vocal folds develop into the exquisite adult vocal fold. Fetal wound healing is known to heal without scar and fetal tissue should contain the keys to develop therapies for scarless healing. Our previous study in neonatal and young rat vocal folds suggested that vitamin A storing cells are present in rat vocal folds as well as in human vocal folds, the vitamin A-containing lipid droplets in MF of rat vocal folds increased with age, and the cell shapes in MF change with age. These results imply the relationship of vitamin A to vocal fold maturity (Tateya T, in press 2005). (In addition, our preliminary data (unpublished) showed distinct keratinization of vocal fold epithelial cells in vitamin A deficient rats. Vitamin A may be involved in the development and maintenance of normal vocal fold structure.) Moreover, histological characteristics of aged and scarred vocal folds share some similar characteristics in terms of excessive collagen and reduced HA. (Hirano, et al unpublished data). This suggests that aged vocal folds can provide with an experimental model similar to the scarred vocal fold model and that the same therapeutic strategy can be applied to aged and scarred vocal folds. Our previous studies about the feasibility of growth factors support this. Growth factor is a potent regulatory element that affects cells and their functions. We have revealed that hepatocyte growth factor (HGF) and basic fibroblast growth factor (bFGF) significantly increases the production of hyaluronic acid (HA) and decreases collagen production from vocal fold fibroblasts in vitro studies. In vivo studies, we have found that local injection of bFGF improved aged vocal folds of rats in terms of histology. Our recent data also shows that local injection of bFGF improved the chronic vocal fold scar in a rat model in-vivo and in-vitro. There are a large number of investigators and consultants that will require organization to manage the many projects. Of the key personnel listed as at UWMadison, one currently resides in Japan and two others will be leaving the U.S. for Japan this year. They are key investigators in Aim 2. Plans for replacement of these positions are not spelled out in the application. During the first five years of funding we have demonstrated the organization and ability to manage many projects. Conference calls, electronic messaging and face-to-face meetings have facilitated coordination, interaction and operations with all key personnel and consultants. Additionally, for the past 20 years there have been Research Fellows from Japan working with Dr. Bless. This arrangement will continue and provide the in-site replacement. Drs. I Tateya, T Tateya and Hirano will continue to be part of the research team as consultants. A. SPECIFIC AIMS A.1. Statement of the Problem Vocal fold scarring is the single greatest cause of voice impairment following vocal fold surgery. 1,2 Such scarring results in the replacement of healthy tissue by fibrous tissue, a process that can irrevocably alter vocal fold function and lead to a decreased or absent vocal fold mucosal wave .3 Even small foci of scar can impede vocal fold function when separation of the body of the vocal fold (muscle) and its cover (epithelium and the superficial layer of the lamina propria) are compromised. Because there is currently no consistently effective treatment for scarred vocal folds, vocal fold scarring is one of the most challenging laryngeal disorders to treat . 4The long-range aim of this project no longer focuses exclusively on sulcus vocalis; it now encompasses the characterization and treatment of the more universal phenomenon of vocal fold scarring. We will accomplish this long-range objective by characterizing laryngeal scarring and its influence on phonation, both pre- and post-treatment, using (1) clinical and surgical trials, (2) controlled laboratory experiments, and (3) computer-modeling experiments. We will use laboratory experiments to investigate treatment effects at the cellular level in animal tissues and excised larynx models. Building on experiments completed over the last 5 years, we will also extend our initial laboratory investigations to the clinical population. It is necessary to combine clinical surgical treatment with systematic laboratory investigations to resolve the complex interactions between tissue characteristics and geometry and the surgical procedures required to create a suitable clinical outcome. A.2. Hypotheses A.2.1. Hypothesis 1. Vocal fold scarring results in predictable changes to vocal fold vibration and phonatory output. We will test specific subhypotheses and attempt varying the properties of the laryngeal scar in several models of vocal fold vibration, including a computational model, a physical model, and an excised larynx model. Subhypothesis 1. The location of the scar along the anterior-posterior and inferior-superior axes determines the severity of the impairment of oscillation and voice much more than the depth of the scar. For example, an anterior scar induces significantly greater impairment than a posterior scar. In addition, there is a critical area within ± 2mm of the superior-medial edge in which scarring is most detrimental to phonation. Subhypothesis 2. A linear increase in the viscoelasticity of the scarred tissue results in an exponential increase in phonation-threshold pressure, making phonation impossible beyond a certain critical threshold of viscoelasticity in scarred tissue. Subhypothesis 3. For mild to moderate scarring, a unilateral scar impedes phonation significantly more than an equivalent bilateral scar. Only for severe scarring does a bilateral scar impede phonation more than an equivalent unilateral scar. A.2.2. Hypothesis 2. The extracellular matrix (ECM) response associated with laryngeal scarring is a major cause of refractory dysphonia that can be prevented and/or minimized with treatment. We will test this hypothesis in the following ways: (1) we will measure the histologic, rheologic, and biomechanical properties of the treated vocal fold during acute and chronic stages of wound repair in a rat model and compare these properties with those of untreated, wounded vocal folds, (2) using cell-culture models, we will culture normal and diseased laryngeal fibroblasts from humans and animals and examine the effects of treatment on the in vitro deposition of the extracellular matrix. Subhypothesis 1. The prevention and/or reversal of changes produced in the vocal fold by scarring will be manifest in treated vocal folds compared with control vocal folds that have been scarred but not treated. Subhypothesis 2. Treated larynges will demonstrate improved aerodynamic properties for phonation characterized by increased vocal economy and reduced phonation-threshold pressure when compared with untreated larynges. Subhypothesis 3. Growth factors will induce an antifibrotic wound-healing response characterized by increased hyaluronan and decreased collagen when compared with untreated, wounded vocal folds. Subhypothesis 4. Upregulation of hyaluronic acid synthase genes will result in an antifibrotic wound-healing response characterized by increased hyaluronan and decreased collagen when treated vocal folds are compared with untreated, wounded vocal folds. Subhypothesis 5. Treatment of a vocal fold scar in rats with a 585nm pulseddye laser (PDL) will induce increased collagen and elastin and decrease the amount of disorganized collagen when treated vocal folds are compared with untreated, scarred rat vocal folds. Treatment with the PDL will improve the pliability of the vocal fold and reduce its aerodynamic inefficiency when it is compared with untreated vocal folds. A.2.3. Hypothesis 3. The location of the laryngeal scar combined with measures of the severity of impaired tissue pliability, geometrical tissue deformity, and glottal insufficiency provide a useful framework for treatment decisions. The impact of glottic insufficiency as a consequence of scarring is an independent variable that can significantly impede entrainment, oscillation, and glottic function. A.3. Aims A.3.1. Aim 1. To measure and contrast the histologic, viscoelastic, and vibratory properties of the pre- and post-treatment tissues associated with vocal fold scarring and to establish functional relationships between these biomechanical variables and phonatory output. This aim will be addressed using systematic data obtained from in vitro models, in vivo models, physical models, and computational models of the vocal folds. A.3.2. Aim 2. To determine the appropriate scaffolds, cells, and growth factors needed to regenerate a scarred vocal fold and examine their therapeutic effects using the same pre- and postoperative measures discussed in Aim 1. Using animal models, we will address this aim with both in vitro and in vivo studies. A.3.2. Aim 3. To determine the role of inflammatory mediators on the development of vocal fold scarring A.4. Significance In the 1995 Chevalier Jackson Lecture entitled "Phonosurgery: past, present, and future," Minoru Hirano suggested that the 2 major laryngeal problems awaiting improvement in the future are scarring and sulcus.1 However, little has changed since this lecture was given because there are no effective treatments for either problem. Both cause deformity of the vocal fold edge, an increase in stiffness of the vibratory structure, and glottic incompetence. Our current proposal is designed to meet this challenge with successful therapies for vocal fold scarring. Our work is important because scarred vocal folds are a significant source of disability. Predicting the clinical course of laryngeal wound healing and identifying optimal therapeutic options can save time, morbidity, and health-care dollars. Thus, this proposal is significant not only because it promises to develop effective treatments for laryngeal scarring but also because it could significantly reduce the amount of health-care dollars spent on addressing this problem. B. BACKGROUND Clinically, the scarred vocal fold represents one of the most challenging laryngeal disorders to treat, and it is regarded as the single greatest cause of voice impairment following phonosurgery.2,3 Currently, no consistently effective forms of treatment for vocal fold scarring exist. Our studies conducted over the past 5 years have helped to quantify the pathophysiologic characteristics of the scarred vocal fold. 5-30 Studies have revealed differences between the acute and chronic stages of vocal fold wound healing, suggesting that the acute and chronic stages of tissue repair have sufficiently different histologic characteristics and may require different treatment approaches. This proposal aims to build on knowledge acquired during the last 5 years to further the understanding of wound-healing events leading to scar formation and to develop better treatment approaches for different presentations of vocal fold scarring based on its underlying pathophysiology. Outcomes of this research have the potential to lead to a greater understanding of the acute and chronic stages of vocal fold wound healing. B.1. Current Treatment Approaches Most treatments for vocal fold scarring are aimed at excising and/or breaking up the scarred tissue or manipulating the ECM to create a tissue environment with optimal biomechanical properties. Current methods of treatment include surgical implantation and/or injection of a desirable substance into the vocal fold lamina propria.3 One of the drawbacks to injectables is that repeat injections are often necessary to maximize efficacy. A downside of implantable materials is that they are subject to the impact forces of vocal fold vibration and may be extruded from the site of implantation. Despite the limitations of these treatment approaches, ECM modification appears to hold the most promise for both the treatment and prevention of scarred vocal folds. 31 Because of limitations inherent in all of the currently available treatments, there is clear need for an improved understanding of what works, what fails, and why. The method that may prove to be most useful in ECM modification is one that stimulates vocal fold fibroblasts to synthesize desired ECM substances and minimize the production of molecules that promote fibrosis. In other words, the goal is to optimize the molecular environment to facilitate an ideal environment for tissue regeneration. The ideal substance would not extrude or migrate when implanted, would have long residence time in tissue, and would recreate the natural biomechanical properties of the vocal fold lamina propria. Alternately, modification of cellular function would provide an optimal situation because cells could produce a more natural extracellular matrix. B.2. Vocal Fold Models One of the problems in studying vocal fold scarring in a clinical population is that presentations of scar are often quite different among patients. Despite the lack of phonation in animals, animal models nevertheless provide a unique solution to this problem. Vocal fold injury can be systematically manipulated in an animal model so that the depth and extent of injury can be controlled, and periodic follow up can be undertaken to assess the different stages of wound healing. Among the different animal models used in laryngeal research are dogs, pigs, rats, and rabbits. Ideally, an animal model appropriate for investigations of scarring should have a larynx that can be phonated in excised-larynx studies for in vitro studies of vocal fold vibratory characteristics post-treatment, a larynx that provides enough tissue for completion of rheologic experiments for in vitro measurements of viscoelastic shear tissue properties, and a larynx that displays similar tissue and biomechanical properties with humans. One of the most frequently used animal models in laryngeal research is the canine model.32 While it is not a perfect animal model for all voice research because of the difference in differentiation of laryngeal layers between dogs and humans16 the length and thickness of the lamina propria in the canine larynx make it an ideal model for the investigation of the surgical management of scarred vocal folds. In addition, the canine larynx can be easily phonated experimentally, the lamina propria provides enough tissue to carry out both histologic and rheologic experiments using the same vocal fold, and the ECM components are similar to those in human larynges. Most important for our work, sulcus scar formation occurs naturally in dogs secondary to kennel cough. 14,35 Of all the animal models used, the rat is particularly good for the study of the prevention and treatment of laryngeal scarring in humans because the vocal fold has a 3-layered structure with ECM components similar to those in humans. It is also small and easy to handle, it regularly produces sound, and it has a short lifespan facilitating long-term follow up of treatments. The application of the rat model to our proposed studies is well justified because we have found that rats demonstrate developmental changes in ECM similar to those reported in humans .20,23 Most important, we have found that rats demonstrate altered tissue characteristics following scarring similar to those observed in humans. Furthermore, wound healing in rats demonstrates morphologic and functional changes in vocal fold fibroblasts and hyaluronic acid, and these changes parallel those observed in human vocal folds.20-23 B.3. The Histology of Vocal Fold Scarring The histologic ultrastructure of vocal folds plays a crucial function in the biomechanical properties of the lamina propria. The ECM of the vocal fold lamina propria consists of a number of important molecules that contribute to tissue characteristics during oscillation. 27,36 These molecules display important biomechanical functions and play critical roles in providing the ECM with structural support that influences tissue viscoelastic properties, regulates the thickness of the lamina propria, and affects fluid content. The vocal fold lamina propria consists of fibrous proteins and interstitial constituents. Collagen and elastin are 2 of the fibrous proteins found in the vocal fold lamina propria. Collagen and elastin contribute to tissue strength and flexibility. The interstitial constituents of the vocal fold lamina propria consist of proteoglycans and glycosaminoglycans. Proteoglycans and glycosaminoglycans, such as hyaluronic acid, occupy the spaces between fibrous proteins. The fibrous and interstitial components of the vocal fold lamina propria have important biomechanical functions that contribute to tissue characteristics during oscillation. These molecules play an important role in determining tissue viscoelasticity, and they may affect clinical voice measures, such as phonatory threshold pressure and vocal fundamental frequency. Thus, an increased understanding of the role of these molecules during wound remodeling should provide an important component in understanding how vocal fold scarring inhibits oscillation and might ideally be repaired to produce normal vibration patterns. Histologically, the scarred vocal fold is characterized by increased or disorganized collagen, decreased elastin, occasionally decreased hyaluronic acid, increased fibronectin, and decreased decorin, which destroys the viscoelastic property of the vocal fold.16,17,20,24,28,37-39 In this sense, the scarred vocal fold loses properties that allow it to be the primary source of vocal vibration. To regenerate normal tissue properties and associated vibratory function, histologic changes must be understood and addressed. Recently, tissue engineering has been used to regenerate tissues and/or their function. The underlying concept of tissue engineering is that tissue consists of 3 elements: scaffolding, cells, and growth factors. Because ECM(ECM) is primarily produced by fibroblasts in the lamina propria of the vocal fold, one strategy to restore normal organization of ECM to the scarred vocal fold would be to control fibroblasts using growth factors. Other reasonable strategies would be to administer cells, such as normal fibroblasts or stem cells, and to provide an appropriate scaffold in which cells can grow and function properly. Our proposed studies aim to determine the appropriate scaffolds, cells, and growth factors needed to regenerate the scarred vocal fold and then examine their therapeutic effects. The studies consist of in vitro studies, in vivo studies using animal models, and clinical studies in human subjects. B.5. Different Stages of Wound Repair The acute and chronic stages of wound healing appear to have sufficiently different histologic characteristics. Thus, it is necessary to investigate both stages to completely understand wound repair, determine treatment effectiveness for different presentations of scar, and improve clinical decision making. For example, Rousseau et al (2003) observed increased procollagen and decreased elastin in a vocal fold scar 2 months postoperatively. Elastin fibers were characteristically tangled and disorganized. However, after 6 months, the vocal fold scar revealed decreased elastin and increased collagen. Collagen fibers also formed thick, disorganized bundles, while the elastin fibers were disorganized throughout the entire scarred lamina propria. Biomechanical measurements revealed increased stiffness and dynamic viscosity for scarred tissue samples in both the acute and chronic scar. Further analysis of the scarred tissue samples for the adhesion molecules fibronectin, cadherin, syndecan-1, and syndecan–4 was also done.11,40,41 Results revealed a significant increase in fibronectin in the superficial layer of the scarred vocal fold lamina propria at both 2 and 6 months and a significant overexpression of syndecan-4 along the basal layer cells of the epithelium during both time periods. These studies have shed some light on the histologic ultrastructure of the scarred vocal fold lamina propria, as well as on factors that might contribute to increased stiffness and tissue viscosity. The studies demonstrated that changes in tissue viscoelastic properties might take place prior to scar maturation (as early as 2 months prior) and that while abundant collagen deposition (observed at 6 months) might influence viscoelastic shear properties, disorganization of collagen and/or elastin fibers (observed during both time periods), thick bundle collagen formation, or the interplay of several of these factors might also play a role. Moreover, results from Hirano et al (2003) suggested that the binding characteristics of fibronectin to collagen, proteoglycans, and other structural proteins might contribute to increased stiffness and dynamic viscosity of the scarred vocal fold. Thibeault et al (2002) studied the histologic and rheologic changes of a vocal fold scar 2 months postoperatively in a rabbit animal model. One of the most important findings from this study was that collagen was decreased during an acute phase of injury, yet stiffness and viscosity were increased. This was important because, traditionally, collagen has been regarded as the single most important cause of biomechanical tissue changes post-scarring. Thibeault and colleagues demonstrated that this notion was not the case during an acute phase of vocal fold injury, and they raised speculation that interstitial proteins may play a more important role in contributing to biomechanical tissue changes than previously thought. B.6. Hyaluronan Hyaluronan is an important glycosaminoglycan found in the vocal fold lamina propria that influences tissue viscosity, tissue flow, tissue osmosis, and wound healing. 38 Hyaluronan is also well suited for the binding of water molecules. This latter characteristic makes hyaluronan an excellent molecule for filling up space. Accordingly, Hertegard et al (2002) and Hallen et al (2001) have had success using cross-linked hyaluronan derivatives (hylan B gel) and the dextranomers in hyaluronan for the treatment of glottal insufficiency due to vocal fold bowing, paresis, paralysis, atrophy, and scarring. Although modified forms of hyaluronan provide increased residence time in tissue, they do not always address the biomechanical properties of the lamina propria sufficiently. Natural hyaluronan likely provides the most ideal substance for optimal tissue biomechanics. Unfortunately, little is known about ways to increase natural cellular production of hyaluronan. Interestingly, hyaluronan is the most prominent ECM molecule in injured fetal tissue, which heals without scarring.44 In fact, this property happens to be one of the major differences between fetal wounds and adult wounds. There are other factors that differentiate fetal wounds from adult wounds, such as an abundance of macrophages and lack of neutrophils during the first 4 days post-injury; a unique cytokine profile that may serve to promote tissue regeneration; and the earlier presence of fibronectin, which may serve as an important scaffold for cell-cell adhesion, cell-ECM adhesion, and epithelial cell migration. 44,45 Each of these factors has the potential to influence the biomechanical properties of the scarred vocal fold. For example, it has been found that the enzymatic removal of hyaluronan from the human vocal fold lamina propria leads to decreased stiffness of the vocal fold cover on the order of 35%, while dynamic viscosity is increased by 70% at frequencies above 1Hz .46 Chan and his colleagues have suggested that hyaluronan likely contributes to the maintenance of the optimal tissue viscosity necessary to facilitate phonation. Hyaluronan may also contribute to the optimal tissue stiffness that is important for vocal fundamental frequency control. Currently, data regarding hyaluronan deposition in the scarred vocal fold are limited to 2- and 6-month time frames post-injury.15-17,27 Thibeault, Rousseau, and associated collaborators found hyaluronan levels in the scarred vocal fold at 2 months post-injury to be similar to control levels in a rabbit animal model. Similarly, Rousseau found hyaluronan levels to be similar to control levels at both 2 and 6 months post-injury in a canine animal model, although in some cases, hyaluronan was mainly observed in the deepest layer of the scarred vocal fold. These findings suggest that although hyaluronan levels are stabilized (return to preoperative levels) by 2 months post-injury, there may be existing differences in the distribution of hyaluronan in the remodeling scar that in turn may affect biomechanical tissue properties. Thus, much can be learned from studying hyaluronan alterations in vocal fold wound healing. An equally important area of study lies in manipulating hyaluronan levels during various stages of wound healing because of hyaluronan’s impact on the ECM, which in turn impacts viscosity and vibratory characteristics. ECMmanipulation has been suggested as a possible treatment technique for vocal fold scarring. 10,46 The goal of ECMmanipulation is to arrive at an optimal balance of ECMconstituents by manipulating 1 or more tissue components. Because hyaluronan is an important molecule contributing to tissue viscosity and scarless fetal wound repair, techniques aimed at maximizing hyaluronan levels during acute wound healing may provide a useful method for restoring optimal tissue viscoelasticity and preventing postoperative scar formation. Our preliminary data with a small sample also suggest that autocross-linked HA gel has an effect on the functional outcomes of vocal folds, such as phonatory threshold pressure and voice production efficacy (Hirano et al. unpublished). HA is synthesized by 3 subtypes of hyaluronic acid synthase (Has) and digested by hyaluronidase (Hyal) in mammals. Using a rat model and real-time polymerase chain-reaction analysis, we’ve observed increased expression of Has1 and Has2 mRNA in the very early phase of vocal fold injury that returned to normal within 2 weeks. We’ve interpreted this finding to suggest that maintaining the upregulation of Has genes may be necessary to achieve scarless wound healing of vocal folds similar to that of a fetus. Consequently, we propose to transfect Has1 and Has2 genes into the injured vocal folds of rats to examine the effect of Has genes on the prevention of vocal fold scarring. B.8. Cell Transplantation Analyses of cellular location and concentration in the vocal fold lamina propria imply that fibroblasts distributed in the lamina propria of the vocal fold are primarily responsible for the production of ECM components. 51,52 Thus, to regenerate vocal fold tissue, it is important to control fibroblasts. It would appear that one means to restore normal organization of ECM to the scarred vocal folds would be to administer drugs, such as growth factors or genes. Other strategies would be to administer cells, such as normal fibroblasts or stem cells, or to provide an appropriate scaffold in which cells could grow and function properly. The studies we propose are significant because they aim to determine appropriate cells and scaffolds to regenerate the scarred vocal fold and then examine their therapeutic effects. The studies consist of in vitro studies, in vivo studies using animal models. B.9. Tissue Engineering Advanced tissue-engineering techniques enable us to regenerate new tissue in cell culture. Appropriate scaffolding, cells, and growth factors are needed to complete this task. Scaffolds should be biodegradable and provide a cell-seeded substrate that can be implanted into the vocal fold lamina propria. There are many possible approaches to developing an appropriate scaffold. For example, cell sheet engineering53,54 is one possible strategy. Cultured cells can be collected as a sheet by coating a culture plate with a temperature-responsive polymer (PIPAAm) that is detached from the plate by reducing the temperature of the polymer. The cultured cell sheet can be easily moved and piled onto another cultured cell sheet to create a 3-dimensional (3-D) cell culture. This technique enables one to construct organs by laying different types of cell sheets. The 3-Dl cell culture was carried out with rat's cardiac cells.54 Lamina propria consists of 3 layers with different concentrations of collagen, HA, and elastin. This engineered cell sheet is suitable as a scaffold to regenerate vocal fold tissue in 3 layers. Our proposed studies aim to find the appropriate scaffolds, cells, and growth factors needed to create a tissue-engineered vocal fold. B.10. In Vitro Inflammation Model of Vocal Fold Fibroblasts Healing of scarless fetal wounds is known to occur without a significant inflammatory processes.57 Since a key feature of scarless fetal-wound healing is an elevated HA level,38 there may be a link between inflammation, specifically through the cyclooxygenase-2 (COX-2) pathway,59 and the production of ECM components (HA and collagen) by proliferating fibroblasts during the wound-healing process. However, this link has not been demonstrated. We plan to establish an in vitro inflammation model of vocal fold fibroblasts and confirm whether any such link exists. This research is significant because it would provide a critical step in explaining the basis for current treatment techniques used to increase HA levels under conditions of inflammation. It would also provide the knowledge necessary to seek novel, more specific therapeutic agents. B.11. Growth-Factor Therapy Growth factors are potent regulatory elements that affect cells and their functions. We have discovered that hepatocyte growth factor (HGF) significantly increases the production of hyaluronic acid and decreases collagen production in vocal fold fibroblasts in vitro.6,7,58 We also have found that local injection of HGF prevented scar formation in injured vocal folds in a rabbit model and even improved the scarred vocal fold in a canine model.55,56 Yet, there are many problems as yet unanswered, such as what dosage of HGF is ideal, how frequently HGF should be injected, and what the best route of the administration of HGF might be. B.12. Cell Therapy Fibroblasts are distributed in the lamina propria of the vocal fold and are primarily responsible for the production of all extracellular matrix.11,12,38,40 Fibroblasts in the scarred tissue have been reported to be altered in terms of their ability to synthesize ECM.11 Injection of fibroblasts into a scarred vocal fold has been suggested as an alternative method of regenerating the vocal fold.41,72 In order to test this assumption, it is necessary to determine which fibroblast should be used and how to control the chosen fibroblast. This step is necessary because the functions of vocal fold fibroblasts, skin fibroblasts, and scar fibroblasts may be quite different. Regenerative medicine uses stem cells. Stem cells can be induced and differentiated into any type of mature cells. Bone marrow-derived mesenchymal stem cells (MSCs) have the potential to become other mature cells as well as bone-marrow cells. MSCs can be easily obtained from humans to avoid problems of allergic response or ethical issues that arise in association with the use of embryonic stem cells. MSC implants into injured vocal folds in the canine model have improved wound healing with less scar formation. Our studies aim to show how to control MSCs and the role they play in the treatment of vocal fold scarring. B.13. Functional Outcome Measures Phonatory threshold pressure (PTP) is a commonly used measure, defined as the minimum amount of lung pressure required to produce vocal fold oscillation.61,62 It is a quantitative measure of the relative ease of phonation. Onset PTP has been described as the minimum lung pressure needed to initiate vocal fold oscillation from rest, while offset PTP is defined as the minimum lung pressure needed to sustain vocal fold oscillation once it has already started.62 In the laboratory setting, onset and offset PTP can be obtained by directly manipulating subglottal air pressure. Vocal economy is typically used to investigate the efficiency with which the vocal folds are able to convert aerodynamic power into acoustic power, and it can be measured from simultaneous recordings of subglottal pressure, airflow, and sound intensity. Vocal economy can be defined as the ratio of acoustic power to aerodynamic power. Thus, the vocal economy measure employed in studies IV and V involved a dimensionless output-cost ratio (OCR) between the acoustic intensity (output) and subglottal pressure (cost). The combination of PTP, OCR, and histologic measures is important in assessing the impact of vocal fold scarring on phonation. Because functional measures of phonation are likely influenced by the underlying tissue structure of the vocal fold, all of these measures should be taken into account when reporting the effects of vocal fold scarring on vocal fold vibration. More studies are needed to investigate the effects of vocal fold scarring on these measures. B.14. Viscoelastic Measurements of Vocal Folds Vocal fold scarring continues to be a challenging clinical entity in the field of laryngology. Multiple treatment options, including medialization thyroplasty, scar/sulcus excision, and vocal fold augmentation with collagen, fascia, and fat, have all been attempted with less-than-optimal results. Failure to achieve an optimal approach is likely based on a lack of understanding of the fundamental nature of vocal fold scarring and how to characterize it. Historically, vocal fold scarring has been characterized by histologic, biochemical, aerodynamic, acoustic, stroboscopic, and rheologic parameters. Rheology of the tissues being tested has been limited by technological barriers. Parallel plate techniques require investigators to excise the entire vocal fold soft tissue away from its cartilaginous attachments and record measurements based on the tissue as a whole. The ability of this technique to record spatially important changes is poor. Parallel plate technology cannot, for example, map the depth at which vocal fold stiffness resides (for example, the epithelium, superficial lamina propria, vocal ligament, or thyroarytenoid muscle). In addition, it cannot localize stiffness along the long and vertical axes of the vocal fold. Importantly, scarring is localized to the epithelium and superficial lamina propria and occupies particular sites along the long and vertical axes. This shortfall in parallel plate technology prevents precise characterization of a vocal fold scar in both site and severity, limiting ability to track focal interventions. As the variety of interventions grows to accommodate the spectrum of problems that are manifest in vocal fold scarring, a more refined characterization of the scar itself will be required to tailor the treatment to the problem. Use of a linear skin rheometer (LSR) in the characterization of vocal fold scarring addresses the shortfalls that parallel plate technology cannot. We intend to characterize the local and regional rheometric changes to animal vocal folds using an LSR in both acute and chronic scar models. We will record rheometric changes induced by the application of growth factors, the 585nm pulsed dye laser, and genetic transfer techniques. We will then integrate the rheometric vocal fold maps into mathematical models of vocal fold oscillation. C.PRELIMINARY STUDIES AND PROGRESS REPORT Following is a list of work accomplished during the first granting period. Not included in the list but noteworthy is that between 2001-2005 seven of the presentations made at scientific society meetings were given peer review awards for scientific merit including ALA Young Faculty Research Award, ABEA Broyles Malony Award, ABEA Scientific Poster Award and the Voice Foundation David W. Brewer for Best Scientific Poster, 1) Hirano S, Kojima H, Tateya I, Ito J. Fiberoptic Laryngeal Surgery for Vocal Process Granuloma. Ann Otol Rhinol Laryngol 111:789-793, 2002. 2) Hirano S, Thibeault S, Bless DM, Ford CN, Kanemaru SI. Hepatocyte Growth Factor and its Receptor CMet in Rat and Rabbit Vocal Folds. Ann Otol Rhinol Laryngol 111:661-666, 2002. 3) Thibeault S, Gray S, Bless DM, Chan RW, Ford CN. Histologic and Rheologic Characterization of Vocal Fold Scarring. Journal of Voice 16:96-104, 2002. 4) Thibeault S, Gray S, Li W, Ford CN, Smith M, Davis RK. Genotypic and Phenotypic Expressions of Vocal Fold Polyps and Reinke’s Edema: A Preliminary Study. Ann Otol Rhinol Laryngol 111:302-309, 2002. 5) Thibeault S, Ford C. The Scarred Vocal Fold. In: Ossoff R, Shapshat S, Woodson G, Netterville J, Eds. The Larynx. Philadelphia, Pa: Lippincott Williams and Wilkins, 2002: 431-440. 6) Kriesel K, Thibeault S, Chan RW, Suzuki T, VanGroll PJ, Bless DM, Ford CN. Treatment of Vocal Fold Scarring: Rheological and Histological Measures of Homologous Collagen Matrix. Ann Otol Rhinol Laryngol 111:884-889, 2002. 7) Suzuki T, Connor NP, Lee K, Bless DM, Ford CN, Inagi K. Age-Related Alterations in Myosin Heavy Chain Isoforms in Rat Intrinsic Laryngeal Muscles. Ann Otol Rhinol Laryngol 111:962-967, 2002. 8) Hirano S, Bless DM, Heisey D, Ford CN. Effect of Growth Factors on Hyaluronan Production by Canine Vocal Fold Fibroblasts. Ann Otol Rhinol Laryngol 112:617-624, 2003 9) Hirano S, Bless DM, Rousseau B, Welham N, Scheidt T, Ford CN. Fibronectin and Adhesion Molecules on Canine Scarred Vocal Folds. The Laryngoscope 113:966-972, 2003. 10) Hirano S, Bless DM, Heisey D, Ford CN. Roles of Hepatocyte Growth Factor and Transforming Growth Factor β1 in Production of Extracellular Matrix by Canine Vocal Fold Fibroblasts. The Laryngoscope Both acute phase of vocal fold injury and chronic vocal fold scar will be examined in terms of the alteration of cells and ECM components in vocal fold lamina propria using animal models. There are two approaches of therapeutic research for vocal fold scarring; to prevent scar formation in acute vocal fold injury and to restore healthy tissue in chronic vocal fold scar. Preliminary data: In normal rat vocal folds, vimentin-positive cells existed in the deep layer of lamina propria and the basement membrane zone, whereas very few myofibroblasts existed in the lamina propria. Following injury, fibroblasts proliferated in the injured site of lamina propria with a peak at day 3 and produce ECM components. Myofibroblasts increased from days 5 and 7 returning to near normal at day 14. The inflammatory granuation tissue was thickest at days 3 and 5 gradually decreasing between 1and 2 weeks. The period of tissue contraction was almost in complete synchrony with the period of myofibroblasts. (Figure 7) HA appeared in injured vocal folds by day 3, peaked at day 5 and thereafter decreased showing lower level than control (Figure 8). Collagen type I also appeared in injured vocal folds by day 3, peaked at day 5 and thereafter gradually decreased though it kept higher level Figure 8: The alteration of ECM components in Figure 7: Cell component than control. vocal fold lamina propria after rat vocal fold changes in rat vocal folds after Collagen type stripping. The scale bar indicates 50m. vocal fold stripping. Cells are III appeared detected by at day 1 and continued to be intense at all time points after immunohistochemical staining for vimentin, a general marker day 3. Fibronectin also appeared at day 1 and continued to of fibroblasts, and alfa smooth be intense for 4 weeks and then decreased close to the muscle actin (alfa-SMA), a control level at 8 and 12 weeks.19,20,21 marker of myofibroblast. The Significance of the preliminary data: These results scale bar indicates 200m. suggested that: 1) What serve as a cell source of vocal folds in response to injury are the fibroblasts in the injured site of the lamina propria. The macula flava do not act as a cell sourse if they are not injured. 2) Myofibroblasts play an important role in producing contraction of the vocal fold scarring and that around 1week following injury is a critical period for wound contraction of the vocal fold scarring. 3) The expression of these ECM components peaks in the period of day 3-5. 4) The tissue remodeling process in scarred vocal folds slows down around 2 months after wounding. 5) The characteristics of vocal fold wound healing are similar to that of skin in the early phases but differ during the subsequent remodeling phase. C2.1.3. Vocal fold development and aging: a rat model Because fetal wounds heal scarlessly characterization of vocal folds through Figure 9: A) Expression of vimentin (purple) and prenatal, postnatal and aging process are collagen type III (green) in important. Vitamin A has been identified in 3-day-old, 3-week-old and the macula flava (MF) of human vocal folds 8-month-old rat vocal folds and rats. It is generally accepted to be a that are sectioned into axial morphogen that controls the differentiation slices. B) Vimentin-positive cells (purple) with nuclei and morphogenesis of cells and therefore it is staining (green) in mid expected to be related to the development membranous portion (MM) and maintenance of vocal folds and may play and posterior macula flavae a significant role in wound healing. We will (MF) of 3-day-old, 3-weekold and 8-month-old rat attempt to identify the key molecules that vocal folds lamina propria. cause age-related changes. To study the role of vitamin A we will use a vitamin a deficient rat model. Preliminary data: MF was observed as a mass of cells that expressed vimentin (general marker of fibroblasts) intensively in the cytoplasm. MF showed denser hyaluronic acid and collagen type I than the mid membranous portion of the vocal folds lamina propria. Clear developmental changes were evident in macula flava and other regions. The vimentinpositive cells of MF in 3-day-old vocal folds were mainly oval-shaped and had less cytoplasm, whereas those in 8-month-old vocal folds were spindle and stellate-shaped and had more cytoplasm, similar to that reported in humans. Vitamin A-containing lipid droplets, were limited to the MF of 3-week-old and 8-month-old rat vocal folds and were not present in 3-day-old rat vocal folds. 23 Significance of the preliminary data: These results suggest that a rat model is useful in studying of vocal folds development and that the presence of vitamin A changes with age. C.2.1.4. In-vitro inflammation model of vocal fold fibroblasts Various treatments have been tested in-vivo and in-vitro. One of these treatments involves Hepatocyte Growth Factor (HGF). HGF has mitogenic, proliferative and anti-fibrotic effects and is produced by vocal fold fibroblasts.55 Increased HA production was observed upon application of HGF to in-vitro vocal fold fibroblast cultures.11 HGF is also known to affect certain cell types and their production of cytokines, and may play a role in inflammation.73 We suggest here that HGF may affect HA production through inflammation. Scarless fetal wound healing is known to occur without significant inflammatory processes. Since a key feature of scarless fetal wound healing is also elevated HA levels57, there may be a link between inflammation, specifically the cyclooxygenase-2 (COX-2) pathway59, and the production of extracellular matrix components (HA and collagen) by proliferating fibroblasts during the wound healing process. However, this link has not been demonstrated in existing literature. This study aims to confirm if any such link exists, to explain current treatment methods aimed at increasing HA levels from an inflammation point of view, and to seek novel, more specific therapeutic agents based on this knowledge. The study will first establish the in-vivo expression of pro-inflammatory factors TNFalpha, Interferon-gamma and NFkappa-B in vocal folds following injury by real-time PCR. These factors will then be administered to in-vitro vocal fold fibroblast cultures, and COX-2 expression will be monitored as a NFkB marker of inflammation. HA and collagen synthase expression monitored as well by Realtime PCR. Introducing pro-inflammatory factors and then HA-level boosting agents will also be studied with relation to COX-2. The adjacent figure shows our preliminary data of mRNA expression level of inflammatory factors in the lamina propria following rat vocal fold 4hrs 8hrs 16hrs 24hrs 72hrs 4hrs injury examined by real time PCR (N=5 in each time point). Y axis shows expression levels of COX-2 a target gene in injured vocal folds compared to those in normal vocal folds. Nuclear factor 1.00E+01 kappa beta (NFkB) showed earliest onset 8.00E+00 bursts following injury with peaks at 8hrs. 6.00E+00 Tumor necrosis factor-alpha (TNF-alpha) 4.00E+00 peaked at 8hrs after injury. Cyclooxygenase-2 2.00E+00 (Cox-2) showed relatively slow response with a 0.00E+00 smaller peak at 4hrs and a larger peak at 4hrs 4hrs 8hrs 16hrs 24hrs 72hrs 16hrs after injury. Transforming growth factorbeta (TGF-B) showed slowest response with relatively weaker expression at 4, 8, and 16hrs than other factors and gradually increased at 24hrs and 72hrs. These expression patterns of inflammatory factors following injury are consistent with those reported in other regions such as skin. C.2.2. Development of growth factor therapy Growth factor is a potent regulatory element that affects cells and their functions. We have revealed that hepatocyte growth factor (HGF) and basic fibroblast growth factor (bFGF) significantly increases the production of hyaluronic acid (HA) and decreases collagen production from vocal fold fibroblasts in vitro studies. 40,41,56 We have revealed that HGF significantly increases the production of hyaluronic acid (HA) and decreases collagen production from vocal fold fibroblasts in in-vitro studies .40,41 We also have found that local injection of HGF prevented scar formation of injured vocal folds in a rabbit model, and even improved the scarred vocal fold in a canine model 15 In vivo studies, we have found that local injection of HGF prevented scar formation of injured vocal folds in a rabbit model 16,26, and even improved the scarred vocal fold in a canine acute phase model to some extent .50 We have also found that local injection of bFGF improved aged vocal folds of rats in terms of histology, which raises the notion that bFGF may also be effective for the treatment of vocal fold with chronic scar which has similar histological characteristics to aged vocal folds. Indeed, our recent data shows that local injection of bFGF improved the chronic vocal fold scar in a rat model in-vitro (Figure 10) and in-vivo (Figure 11).22 We are now attempting to determine the ideal combination of growth factors, dosages, the best frequency of injection and the best route of Figure 10. Effect of bFGF on administration to maximize the effect on the vocal fold cultured fibroblasts obtained 1.20E+01 1.20E+05 1.00E+01 1.00E+05 8.00E+00 8.00E+04 6.00E+00 6.00E+04 4.00E+00 4.00E+04 2.00E+00 2.00E+04 0.00E+00 0.00E+00 TNF-alpha 8hrs 16hrs 24hrs 72hrs 24hrs 72hrs TGF-B 1.40E+02 1.20E+02 1.00E+02 8.00E+01 6.00E+01 4.00E+01 2.00E+01 0.00E+00 8hrs 16hrs 120 100 80 Normal-Has1 Scar-Has1 60 Normal-Has2 Scar-Has2 40 20 0 0hr 3hrs 6hrs 12hrs 24hrs from chronic rat vocal fold scar examined by real-timeFigure 11. Effect of growth RT-PCR. Has 2 mRNA factors on chronic rat vocal fold scar in vivo(Alcian Blue expression level in fibroblasts from scarred staining for HA). HA in bFGF vocal fold increases higherinjected rats have significantly higher HA than than that in fibroblasts from sham and HGF injected rats. normal vocal fold. scarring, and ultimately to provide the bases to initiate clinical studies. The problems left are how much dosage of HGF and bFGF is ideal, and how frequently HGF and bFGF should be injected, and which of them has a better effect on acute and/or chronic vocal fold scar. The best route of the administration should be warranted. C.2.3. Prevention of scar and regeneration of vocal fold: for a future treatment These studies aim to develop new treatment methods of acute/chronic vocal fold scar for a future clinical treatment. Animal models are used for this study. Gene therapy and tissue engineering techniques will be used for the regeneration of the vocal fold tissue. C.2.3.1. Gene therapy Human vocal fold lamina propria consists of ECM components and cell components, and hyaluronic acid (HA), collagen, and elastin are main components of ECM that play vital roles in mechanical and biological functions. 46,48.74 Our preliminary studies have supported the notion that HA has important biological functions other than acting as a space filling material and that it serves both as a pathway for cell migration and influences cell proliferation and differentiation. Using a rat model and real-time PCR we observed an increased expression of Has1 and Has2 mRNA in the very early phase of vocal fold injury which returned to normal within 2 weeks. This suggested that maintaining upregulation of Has genes may be necessary to achieve scarless wound healing of vocal folds similar to that seen in a fetus. In Figure 12. mRNA expression of Has proposed studies we will transfect Has1 and Has2 genes into injured 1, 2, and 3 genes following rat vocal folds of rats to examine the effect of Has genes on prevention of vocal fold injury revealed by real-time PCR fold scarring. Our preliminary studies (Figure 12, 13) have also shown the effect of bFGF and HGF on vocal fold scarring. Administration of bFGF for the chronic vocal fold scar returned HA to normal level and HGF injection for acute phase scar returned collagen level to normal. However,. bFGF wasn’t effective in terms of collagen and HGF treatment didn’t improve the aerodynamics. One of the reasons for the insufficient effect is thought to be a short half-life of growth factors, only a few days. Because transfection techniques maintain Figure 13. Expression of Has2 mRNA following rat vocal fold injury revealed expression of a target gene for a longer period Tateya sought training by in-situ hybridization. and gathered pilot data. In pilot studies bFGF and HGF were overexpressed by transfection to prevent/restore vocal fold scarring using a rat model. Of transfection strategies we opted for non-viral methods because they are non invasive and considered to be suitable for the treatment of benign conditions, such as vocal fold scarring. In-vivo electroporation technique was used as a first step in order to maximize the transfection efficacy . The adjacent figure shows a coronal section of bilateral rat vocal folds 2 weeks after electroporation of enhanced green fluorescence protein (EGFP) gene. Transfected cells in the injected side of the vocal folds shows strong green fluorescence whereas little signal is observed on the contralateral control side. C2.3.2. Cell transplantation Lamina propria consists of ECM components and cell components, mainly fibroblasts. Our preliminary work has shown the distribution of fibroblasts in the lamina propria of the vocal fold of developing rats. It has also demonstrated that the fibroblasts may be primarily responsible for the production of every ECM components.51,52 We’ve also determined to regenerate vocal fold tissue, it is important to control fibroblasts by administrating drugs, such as growth factors or genes, to restore normal organization of ECM to the scarred vocal fold. Our continued studies aim to find out appropriate cells and scaffolds to regenerate the scarred vocal fold, and then examine their therapeutic effects. The studies consist of in vitro, in vivo using animal models, and human subjects. C2.3.3. Establishment of in-vitro inflammation model of vocal fold fibroblasts As previously stated in preliminary work various treatments have been tested invivo and in-vitro. One of these treatments involves Hepatocyte Growth Factor (HGF). HGF has mitogenic, proliferative and anti-fibrotic effects and is produced by vocal fold fibroblasts .55 Increased HA production was observed upon application of HGF to in-vitro vocal fold fibroblast cultures.11 HGF is also known to affect certain cell types and their production of cytokines, and may play a role in inflammation.73 We suggest here that HGF may affect HA production through inflammation. Scarless fetal wound healing is known to occur without significant inflammatory processes.. Since a key feature of scarless fetal wound healing is also elevated HA levels .57 there may be a link between inflammation, specifically the cyclooxygenase-2 (COX-2) pathway59, and the production of extracellular matrix components (HA and collagen) by proliferating fibroblasts during the wound healing process. However, this link has not been demonstrated in existing literature. Our continued work aims to confirm if any such link exists, to explain current treatment methods aimed at increasing HA levels from an inflammation point of view, and to seek novel, more specific therapeutic agents based on this knowledge. D. RESEARCH DESIGN AND METHODS This section is divided into two sections; methods and research design. A table summarizing the relationship of the methods to each specific aim is provided in the Appendix. The methods that will be commonly used in our series of experiments are summarized here and referred to by letter. Method A describes animal models of vocal fold scarring; Method B tissue preparation; Method C histology; Method D protein analysis; Method E gene analysis; Method F rheologic examination; Method G excisedlarynx acoustic, aerodynamic, and movement analysis; and Method H clinical assessment. These methods are based on knowledge and experience gained during the last 5 years of work on laryngeal scarring. Methods that are unique to an individual experiment are described separately. The number of rats determined for each experiment were based on needs to meet adequate statistical power and numbers that could be easily handled each year without posing any hardship on staff or facilities. D.1. METHODS D.1. Method A: Animal Models of Vocal Fold Scarring D.1.1. Rat videolaryngoscopic surgery. Rat videolaryngoscopic surgery will be performed as described by Tateya.20 Rats will be anesthetized with an intraperitoneal injection of ketamine (90mg/kg) and xylazine (9mg/kg). The animals will be placed on an operating platform in a near-vertical position. A suspension microlaryngoscope fabricated from a 1mm diameter Figure 14 (A) Rat videolaryngoscopic surgery. A rat is placed on an steel wire20 will be operating platform in a near-vertical inserted though the position. A suspension animal’s mouth to microlaryngoscope fabricated from help visualization 1mm diameter steel wire is inserted of vocal folds. though the mouth to help visualize the vocal folds. (B) A rat larynx Vocal folds will be visualized by monitoring with a visualized by 1.9mm diameter telescope with an angle of 25. (C) Left vocal fold stripping is performed using a 25G needle. The right side is kept intact and used as a control. monitoring with a 1.9mm diameter telescope with an angle of 25 (Richard Wolf, Vernon Hills, IL, USA). Using a 25G needle and microforceps, unilateral vocal fold stripping will be performed for histologic study and in situ hybridization, and the thyroarytenoid muscle will be exposed. The contralateral side will be kept intact and used as a control. For realtime polymerase chain-reaction (PCR) study, bilateral vocal fold stripping will be done to get enough sample volume to perform real-time PCR, and control samples will be collected from untreated rats. The rats will be anesthetized with a mixture of ketamine (90mg/kg) and xylazine (9mg/kg) and humanely euthanized by injecting a euthanasic agent (0.22mL/kg) intracardially. D.1.2. Canines with kennel cough exhibiting general edema and unilateral or bilateral sulcus. The larynges of these canines will be obtained from the kennel cough cases that have been sacrificed for other purposes and identified by veterinarians in the School of Veterinary Medicine, University of Wisconsin-Madison. These excised canine larynges with naturally occurring sulci will first be run on the excised-larynx system (Method G) to determine the impact of the sulcus on vibration. The same specimens will subsequently, be histologically studied (Method C) to determine how the location and depth of the sulcus impact vibration. No surgery will be done on these specimens. D.1.2. Method B: Tissue Preparation D.1.2.1. Human and canine larynges. Human larynges will be obtained from autopsy cases and canine larynges will be obtained from the cases used and euthanized in the School of Veterinary Medicine, University of Wisconsin-Madison. For histology specimens (Method C), vocal fold tissue will be cut into pieces of approximately 0.5mm thickness coronally or horizontally, quickly frozen with a combination of acetone and dry ice, and preserved in a –80oC freezer. Ten to 30µm cryostat sections of vocal folds will be prepared, air-dried, and stored at -20oC until they’re used. For electron microscopy, larynges will be sectioned into pieces of 0.5-1.0 x 5 x 10mm. For rheologic examination (Method F) and excised-larynx studies (Method G), whole larynges will be removed, quickly frozen with liquid nitrogen, and then preserved in a –80oC freezer until they are used. D.1.2.2. Rat tissue preparation. Rat tissue will be obtained using rat videolaryngoscopic surgery under the procedure described in Method A. For histologic study (Method C), whole excised rat larynges will be harvested soaked in embedding medium (optical coherence tomography compound, Tissue-Tek, Kyoto, Japan), quickly frozen with a combination of acetone and dry ice, and kept in a freezer at –80oC. For conventional stains, 10µm cryostat coronal or axial sections of vocal folds will be prepared, air-dried, and stored at -20oC until used. For immunohistochemistry study, 10 to 30µm cryostat coronal or axial sections of vocal folds will be prepared, air-dried, and stored at -20oC until used. For protein analysis (Method D) and gene analysis (Method E), whole excised rat larynges will be harvested soaked in embedding medium, quickly frozen with a combination of acetone and dry ice, and kept in a freezer at –80oC. Additionally, for protein analysis (Method D) and real-time reverse-transcription PCR (RT-PCR), a microdissection technique will be used to collect the lamina propria from larynges accurately. Sixty µm cryostat axial sections of the vocal folds will be prepared and the entire lamina propria dissected by visualizing it with a microscope and using 30G needles. The tissue will be collected in tubes and kept in a freezer at –80oC. For rheology (Method F) and excised-larynx study (Method G), the whole larynx will be removed, quickly frozen with liquid nitrogen, and then preserved in a –80oC freezer until it is used. D.1.3. Method C: Histology D.1.3.1. Conventional stains. Elastica-van-Gieson (EVG) staining will be performed to identify collagen and elastin separately. Masson’s trichrome staining will be used to detect collagen fibers more clearly than with EVG staining. Alcian blue staining (pH 2.5) will be used to identify HA. The hyaluronidase digestion technique will be used to detect HA. For the hyaluronidase digestion procedure, 50mg of bovine testes hyaluronidase (Sigma, St. Louis, MO) will be diluted in a 100mL phosphate-buffered saline (PBS) solution. Each section will be incubated in this solution for 1 hour at 37oC. Next, the sections will be stained with Alcian blue (pH 2.5). HA will be detected by comparing the sections without digestion to those with digestion. Five slides will be used for each stain per animal. D.1.3.2. Immunohistochemistry. Tissue sections will be unfixed or fixed in 4% paraformaldehyde and washed 3 times in a PBS solution. For immunofluolescence study, sections will be blocked with 5% normal goat serum and 0.1% Triton-X in PBS, incubated with adequately diluted first antibodies with 1% normal goat serum and 0.1% Triton-X, washed in PBS, and incubated with adequately diluted second antibodies and TOTO-3 (200nm). Finally, samples will be washed 3 times in PBS and mounted on coverslips in Vectashield (Vector Labs, Burlingame, CA) for observation under a laserscanning confocal microscope (Bio-Rad H600, Hercules, CA). A DakoCytomationLabelled Streptavidin-Biotin2 System (Dako, Carpinteria, CA) will also be used for lightmicroscopy observation using the same first antibodies and counterstaining them with Mayer’s Hematoxylin. D.1.3.3. Electron microscopy (Immuno-SEM). Immunohistochemstry is done the same method as stated above in Method C except for using the thick sliced tissue (see Method B) and gold- conjugated secondary antibody. After immunolabeling, the tissue is fixed in 1% glutaraldehyde for 1 hour, dehydrated in a graded series of concentrations of ethanol and dried using a dryer for 1 hour, and coated with an iron beam coater. Cd \ Md Observation is conducted with a Hitachi S900 High Resolution, Low Voltage, FieldEmission Scanning Electron Microscope (Hitachi High Technologies America, Inc. Pleasanton, CA). D.1.3.4. Optical coherence tomography (OCT).. All of the laryngeal scars studied in our excised-larynx experiments will be imaged with an OCT system obtained from the Ophthalmology Department at the University of Wisconsin-Madison (see letter of support). This system is the same one reported in our preliminary studies. Because this technology is currently being adapted for clinic use, the laboratory techniques used to characterize laryngeal scarring should eventually be available in clinics. Indeed, OCT used in operating rooms has already helped guide the surgical treatment of laryngeal carcinoma 79 although the additional restrictions of endoscopy introduce new challenges as surgeons and engineers attempt to achieve clarity and precision of in vitro images. 80,81 Attempting to use OCT to image the laryngeal mucosa in an outpatient office setting would present additional challenges .82 D.1.4. Method D: Protein Analysis D.1.4.1. Enzyme-linked immunosorbent assay (ELISA). Hyaluronic acid production will be examined using a sandwich ELISA test. Ninety-six-well microtiter plates (Fischer Scientific, PA) will be coated with 25μL of 0.5μg/mL hyaluronic acid binding protein (HABP; Seikagaku America, MA) and incubated overnight at 4oC. The plates will be blocked with 2% bovine serum albumin (BSA) in a sodium phosphate buffered solution (pH 7.1), and incubated for 2 hours. The plates will be washed 3 times with PBS containing 0.05% Tween 20, and then twice with PBS. Twenty-five microliter aliquots of standard HA (Seikagaku America, MA) or samples will be dispensed into the wells and the plates incubated for 1 hour. Samples will be examined in duplicate. After the plates are washed, 25 microliter aliquots of 1μg/mL biotin-labeled hyaluronic acid binding protein (B-HABP; Seikagaku America, MA) will be added into the wells. The plates will be incubated for 1 hour and then washed. After the addition of 25 microliter aliquots of 1μg/mL peroxidase-conjugated streptavidin (Pierce Endogen, IL), the plates will be incubated for 30 minutes and then washed again. An aliquot (40μL) of 3,3',5,5'tetramethylbenzidine (TMB) (KPL Inc., MD) in an acidic buffer will be added. The reaction will be stopped with 40 microliter TMB stop solution. Absorbance will be read at 450nm by a microplate reader (ELX800, Bio-Tek Instrument Inc., VT). The concentrations of HA in samples will be extrapolated from the standard curve. Soluble collagen type I in supernatant media will be detected by capture ELISA kit (MD Biosciences Inc., Montreal, Canada) and fibronectin production will be examined using an inhibition ELISA kit (Chemicon International Inc., CA). D.1.4.2. SDS-PAGE. Samples will be immediately placed in a skinning solution (100mM KCl, 10mM imidazole, 1mM MgCl2, 2mM EGTA, 4mM ATP, 1% Triton X-100, and 1% protease inhibitor cocktail; pH 7.0) at 4°C for 60 minutes and then washed in an identical solution without Triton at 4°C for 2 minutes. Next, the samples will be placed in 50µL boiling buffer solution (5% SDS, 10% glycerol, 60mM Tris; pH 6.8), heated, and vortexed for up to 30 minutes to facilitate dissolution. The samples will then be frozen and stored at -80°C in preparation for electrophoresis. Two-dimensional SDS-PAGE will be performed using the method described by O’Farrell et al. 69 Isoelectric focusing will be performed in glass tubes (2.0mm inner diameter) using 2.0% pH 3.5-10 ampholines (Amersham Pharmacia Biotech, Piscataway, NJ) for 9600 V-hours. Fifty ng of an isoelectric focusing internal standard (either carbonic anhydrase or tropomyosin) will be added to each sample. Carbonic anhydrase migrates with a molecular weight (MW) of 29kDa and an isoelectric point (pI) of 7.3. Tropomyosin migrates with a MW of 33kDa and pI of 5.2. A pH gradient plot for the set of ampholines will be generated using a surface pH electrode. The gels will be silver-stained using the protocol described by Oakley et al .70 The gels will be scanned using an Agfa Arcus II flatbed scanner (Agfa, Mortsel, Belgium) in transparent mode at 200 dpi resolution and 24-bit image depth. Image analysis will be performed using Melanie 4.02 software (GeneBio, Geneva, Switzerland) and Melanie II-a software (Swiss Institute of Bioinformatics, 2003). This software package utilizes Figure 15. Illustration of quantifiable protein-spot a protein-spot detection strategy incorporating a features, visualized using (A) an intensity variation profile and (B) a 3-D representation of the diffusion-smoothing algorithm, a second derivative highlighted area. (MW = molecular weight, pI = feature-detection algorithm, and a minimum pixel-area isoelectric point, Int. = pixel intensity.) parameter. Quantifiable spot features (used as indices of relative protein quantity) include optical density (OD), area, and volume (Figure 15). The OD will be calculated as the difference between the maximum pixel intensity in a given spot and the minimum pixel intensity in the background region immediately adjacent to the spot. The area (inside the spot border) will be calculated at 0.75 of OD (as measured from the point of maximum pixel intensity). The volume will be calculated as the sum of the intensity of each pixel within the spot border. Estimated MW and pI values for identified spots will be determined from interpolation and extrapolation (logarithmic for MW; linear for pI) of values from known internal standards. D.1.5. Method E: Gene Analysis D.1.5.1.Real-time RT-PCR. Tissue from Method B will be treated with proteinase K. mRNA will be extracted using an RNeasy Micro kit (Qiagen, Valencia, CA, USA) and treated with RNase free DNase I (Qiagen, Valencia, CA, USA) to digest potentially contaminated genomic DNA. Reverse transcription will be performed using Superscript III (Invitrogen, Carlsbad, CA, USA) to synthesize first-strand cDNA. Real-time PCR will be performed in a 20µL volume using the manufacturer's protocols and the reaction mix will be examined. The mix is composed of 2µL of template cDNA, 2µL of LightCycler DNA Master SYBR Green I (Roche Applied Science, Indianapolis, IN), 4mM MgCl2, 0.5µM final concentration of each primer, and RNase-free H20 to 20µL and expression of target genes, such as Has1, Has2, Has3, Hyal1, Hyal2, Hyal3, Hyal4, matrix metalloproteinase (MMP)-1, MMP-8, MMP-9, MMP-13, and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) genes. Amplification will be performed under the following conditions: 1 cycle of 95°C for 110 seconds, followed by 40 cycles of 95°C for 10 seconds, 55°C for 10 seconds, and 72°C for 20 seconds, and 1 cycle of 60°C to 95°C to make a melting curve. Fluorescence will be detected with a Smart Cycler II system (Cepheid, Sunnyvale, CA) and accompanying software. RT(-) samples, for which reverse transcriptionase is not added during RT, will also be treated with PCR reaction as a negative control sample to clarify that an amplified DNA band is not made from contaminated genomic DNA. Primer dimmer production will be checked using melting curves and gel electrophoresis after PCR. Quantitative analysis will be performed based on a delta-CT method using standard curves, and the ratio of target gene concentration to GAPDH will be calculated. Statistical analysis will be performed by non-repeated ANOVA with a significant p value of 0.05. D.1.5.2. In situ hybridization. In situ hybridization experiments will be performed as described by Takebayashi, Akazawa, and Kageyama (1995) with some modifications84. In brief, cDNA templates of a target gene will be generated by PCR. cDNA, including the coding region, will be subcloned into pGEM-T Easy (Promega, Madison, WI) and used as the template for generating digoxigenin (DIG)-labeled RNA probes by in vitro transcription. The templates will be generated by linearization with restriction enzymes for each antisense and sense probes. Antisense probes will be synthesized by runoff transcription from a T7 promoter with DIG-uridine triphosphate using an RNA labeling kit (Roche Applied Science, Indianapolis, IN). Meanwhile, DIG-labeled sense probes, synthesized by runoff transcription from SP6 promoter will be used as negative control probes. The tissue sections described in Method B will be fixed in 4% paraformaldehyde (PFA) for 30 minutes, rinsed with 0.1M phosphate-buffered saline (pH 7.5) containing 0.1% Tween-20 for 5 minutes twice. Hybridization will be performed at 65°C overnight in a hybridization buffer (50% formamide, 1% dextran sulfate, 5 x SSC, 50ug/mL heparin, 50ug/mL yeast tRNA) containing DIG-labeled RNA probes. The sections will be washed in 5 x SSC at 65°C for 30 minutes, 2 x SSC at 65°C for 30 minutes 3 times, and washed with TBST 3 times. The probes will be revealed by alkaline-phosphatase-coupled antiDIG antibodies (Roche Applied Science, Indianapolis, IN), which react with nitrobluetetrazolium-chloride and 5-bromo-4-chlor-indolyl-phosphate substrates for color reaction. D.1.6. Method F: Rheologic Examination D.1.6.1. Linear viscoelastic shear properties. Linear viscoelastic shear properties of the scarred and normal lamina propria will be measured. Elastic shear modulus (G’) and dynamic viscosity (Eta’) will be determined as a function of oscillation frequency (0.1-300 Hz). Larynges will be excised immediately postmortem and quick frozen using liquid nitrogen and then stored in a freezer at –70oC. Prior to analysis, the larynges will be thawed overnight at 4oC and warmed gradually to 37oC, at which time the lamina propria will be dissected. The tissue samples will be maintained at 37oC +0.1oC in a water bath until mounted in a rheometer for viscoelastic measurements. This temperature will also be maintained in the rheometer via a temperature-control unit. Small amplitude sinusoidal oscillatory shear deformation of the sample will be performed with a controlled strain rheometer (RFS-3 Rheometric Scientific, Piscataway, NJ). A parallel plate (plate on plate) testing geometry will be used, consisting of a stationary lower plate and a rotating upper plate (diameter = 7.9mm) and a gap size of 1mm. The lamina propria sample will be placed in the gap between the two plates and subjected to precisely controlled sinusoidal torque. A sensitive transducer will monitor the resulting angular displacement and angular velocity of the upper plate as a function of time. Shear stress, shear strain, and the strain rate associated with oscillatory shear deformation will be computed from the prescribed torque and the measured angular velocity by a computer, and linear viscoelastic functions (elastic shear modulus G’ and dynamic viscosity Eta’) will be quantified based on the theory of linear viscoelasticity. A shear-strain amplitude of 1.0% will be used to ensure oscillation linearity, and measurements will be obtained at a frequency of 0.1-316 rad/s (corresponding to 0.01650Hz) at 37oC. The viscoelastic data will be compared using Student’s paired t test for the normal and treated side in each group, and Mann Whitney nonparametric testing will be used for comparison between growth factor-treated and sham-treated vocal folds. A p value < 0.05 is considered statistically significant. D.1.6.2. LSR basic equipment.. Laryngeal specimens from animal sources will be prepared by sagittal hemisection, taking care to leave the vocal fold attachment to the thyroid cartilage at the anterior commissure region intact. The specimens will be affixed to a firm table-top. The specimens will be kept moist with physiologic saline and measurements will be made at room temperature (roughly 20oC). Measurements will be made using needle-tipped probes that have a fine ridge carved into them 1mm from the distal tip so that consistent depth penetration can be monitored. We will use the most effective of several designs tested; the needle is made from a spring steel rod 1mm in diameter and 10cm in length and bent to a right angle 5mm from one end. A fine insect pin will be soldered to the short bent section so that it protrudes 1.5mm beyond the end of the rod. This needle will be inserted into the tissue up to the rod, which controls the insertion depth to 1.0mm. Basic materials will include human, dog, and rat larynges. Dog and rat vocal folds will be subjected to manipulation with growth factors, a 585nm pulsed dye laser, and genetic transfection. The vocal folds will be tested along with controls using the materials described above. Dog vocal folds will be tested several times at 24 to 30 points along the Figure 16. Schematic drawing of a linear folds for maximal mapping of rheologic changes. Rat vocal skin rheomatic sensing head. folds are too small to allow for mapping, so 1 central point will be tested on the control side and on the test side, using multiple trials at this central point to maximize statistical power. Using these noninvasive measurements of histologic and viscoelastic properties of the laryngeal mucosa, we can correlate the properties of the scarred folds with the resultant acoustic (phonatory) signals. For our in vitro studies, we will be using an OCT system provided to us by the Department of Ophthalmology at the University of Wisconsin (see signed statement). For the LSR studies, we will be using a system designed by Eric Goodyer (see Appendix for additional details). D.1.7. Method G: Excised Larynx Experiments We will examine vocal fold vibration in larynges using an excised larynx setup that maintains in vivo conditions of Figure 17. Scheme of excised larynx setup temperature and humidity while recording high-speed images of the vibratory pattern, airflow, pressure, and acoustic signal. In addition, normal untreated larynges will be examined in the identical manner and used as controls. To better visualize the vocal folds of excised whole larynges, supraglottic structures, such as the epiglottis, the false vocal folds, and the aryepiglottic folds, will be removed following resection of the superior portion of the thyroid cartilage. Both right and left arytenoid cartilages will be sutured to each other by 5-0 or 6-0 nylon strings to obtain glottal closure. Figure 17 shows the general experimental setup we will use to monitor vocal fold vibration. The larynx will be mounted with the upper section of the trachea mounted on top of a pipe. The trachea is tightly clamped to the pipe with a hose clamp to avoid any air leakage. The larynx will be stabilized with a circular multipronged device. An air compressor will be used to generate airflow. The flow quantity will be controlled Figure 18. Measurement of mucosal wave amplitude using a rabbit model. throughout the experiment with a valve and measured (A) closed phase, (B) maximum open with a flow meter. The air will be humidified to 100% phase. Mucosal wave amplitude = (d2humidity at 36 to 38oC by passing it through a heaterd1) / L. (d1, d2 = the distance from the humidifier (3M, Bird Co., Palm Springs, CA). Continual midline of the glottis to the free edge of the vocal fold, L = the length from the dripping of saline onto the vocal folds will also help anterior commissure to the vocal prevent dehydration of the vocal folds. process.) A high-speed digital imaging system (Kodak Ektapro [Photron] 4540) will be used to record glottal vibrations from a superior view using a Nikon lens (200mm micro-Nikkor). The camera will be mounted 50cm above the larynx and the image viewed on a monitor. The images will be recorded at a frame rate of 4500 frames per second with a CCD array of 256 x 256 pixels and an 8-bit monochrome intensity level per pixel. A pressure sensor (Micro switch PK8772-4, Honeywell Inc., IL) will be mounted on the pipe directly beneath the vocal folds to monitor subglottal pressure. Subglottal pressure will be increased by 2cmH2O increments from the phonatory threshold pressure, and glottal images will be taken at each increase. The phonatory threshold pressure, vocal efficiency, amplitude of mucosal wave, and glottal gap will be compared across normal, treated, and sham groups. Vocal efficiency is defined by the formula: sound pressure level [dB] over subglottal pressure [cmH2O]. The amplitude of mucosal wave and glottal gap will be examined using image analysis software (Scion Image beta3b, Frederick, Maryland). The distance (d1) from midline of the glottis to the free edge of the vocal fold will be measured at the anteroposterior middle portion of the vocal fold at the closed phase, and then the same distance (d2) will be measured at the maximum open phase (Figure 18). We will define the mucosal wave amplitude by subtracting d1 from d2 and then Figure 19. Measurement of normalize it by dividing the result by the length (L) glottal gap using a rabbit from the anterior commissure to the vocal model. Glottal gap = a / L2. (a = glottal area, L = the length from process: mucosal wave amplitude = (d2-d1) / L. the anterior commissure to the The glottal gap will be examined on the images vocal process.) obtained at the closed phase. The glottal area (a) will be measured and then normalized by dividing it by L2 (Figure 19): glottal gap = a / L2. Perturbation measures will be obtained from the high-speed images using the Yan GAW (2004) analysis program that converts the glottal area waveform into perturbation plots.77 Measures of the mucosal wave will be obtained from software developed by Jiang (2005). These values will be calculated in each larynx at PTP and 18cmH2O of subglottal pressure.85 D.1.9. Method I: Surgical Treatment: Animals and Humans D.1.9.1. Pulsed dye laser in animal models. A 585nm PDL (Cynosure, Chelmsford, MA) will be used in acute and chronic scar models in the rat. With the rat under anesthesia and the vocal folds exposed (Method A), the PDL will be applied through a 600-micron flexible fiber. The fiber will be supported from the superstructure of the device holding the rat. A non-test vocal fold will be covered by dark impermeable material to prevent exposure to the PDL. The total exposure of the vocal folds to the energy of the PDL will vary. The fiber tip will be at variable distances from the test vocal fold to alter the fluence (laser energy) applied. The energy per pulse can also be adjusted (approximately 500 millijoules), as can the number of total pulses. The fiber tip will be introduced perpendicular to the medial surface of the test vocal cord. Surgilube will be lightly applied to the vocal fold prior to PDL application to prevent drying of the fold from the laser. After application of the PDL, the rat will be awakened and maintained until serial PDL applications are completed or euthanasia (Method A). Each experimental rat will undergo at least 1 PDL application. One month after the last PDL application, each rat will be euthanized and the larynx subjected to analysis using excised larynx vibration, LSR, histology, and ELISA testing (see Methods G, F. A, C, and D, respectively). D.2. RESEARCH DESIGN D.2.1 Computational Model of the Vocal Fold D.2.1.1. Different anterior-posterior lengths of a mucosal scar in the finite-element model. In a finite-element study from our previous proposal (Berry et al, in press), we have already investigated most of the variations enumerated in the physical model experiment described in D.2.2 below. The only exception is that we have not yet studied variations in the anterior-posterior length of the scar. There is some indication in the literature that such variations in the viscoelastic tissue properties along the anteriorposterior length of vocal folds may be responsible for generating different anteriorposterior vibration modes in vocal folds (Neubauer, 2001). Furthermore, prior clinical experience suggests that an anterior scar is more detrimental to phonation than a posterior scar, although this observation or hypothesis has never been systematically evaluated using laboratory or computational models of phonation. Thus, we propose to investigate this hypothesis and implement anterior-posterior variations in scar length and report the resultant tissue vibrations and acoustic output. We will use descriptive statistics to summarize our findings from the finite element modeling. D.2.1.2. Left-right asymmetry in the finite-element model. To achieve left-right asymmetry, we will repeat experiment D.2.2 from the physical model experiment described below on the finite-element model. The only exception is that a near-complete set of permutations between left and right will be performed on the model, because repeating an experiment thousands of times (72 x 72 = 5184) is feasible on a computer model but not on a physical model. The results of the computer modeling will be summarized with descriptive statistics. D.2.2Physical Model of the Vocal Fold D.2.2.1. Investigating the influence of the size and position of a vocal fold scar using a physical model. A physical model enables precise positioning and sizing of the sulcus in the vocal fold mucosa, much more so than in human subjects or excised-larynx models. In addition, because a physical model’s oscillations are flow-induced in an actual physical setup and are not subject to numerical instabilities, the results from these experiments provide a completely independent assessment of the predictions generated from computer studies. As described in our preliminary studies, a physical model of a normal vocal fold will be made by curing a polyurethane compound into a cast or model of the desired vocal fold shape. The scarred vocal fold will be generated as follows: (1) Use the same cast as that for a normal vocal fold. (2) Using the appropriate ratios of the polyurethane materials, generate a polyurethane block that is 3 to 30 times as stiff as a normal vocal fold (the normal fold has a stiffness of approximately 14kPa). Let the block cure. This block will serve as the material from which to extract the vocal fold scar. (3) Out of this block, cut a cylindrical rod of desired diameter. Cut the rod in half by placing a scalpel along the circular diameter of 1 of the ends of the rod and then cutting the rod along its entire length. (4) Place the half-cylinder rod in the desired location of the cast, with the flat end (e.g., the cut end) facing the bottom of the cast (e.g., the medial surface of the fold). (5) Pour a polyurethane liquid into the cast over the scar. (6) Wait until the polyurethane substance cures. (7) After creation of two such vocal folds, the folds will be mounted into acrylic plates and then pressed together, with the plates mounted over a supply of compressed air, as described in our preliminary studies. (8) Subglottal pressure will be increased, starting from zero, until phonation occurs. The following variables will be measured: (a) phonatory threshold pressure, (b) amplitude of vibration, (c) degree of glottal closure, (d) mucosal wave velocity, (e) mucosal wave shape, (e) glottal airflow, and (f) acoustic output. We will measure the vibration variables under the following conditions: (1) The lateral depth of the scar will be changed at the following increments: 0.5, 1.0, 1.5, and 2.0mm (4 conditions). (2) The vertical thickness of the scar will be implemented at 0.5 and 1.0mm (2 conditions). (3) The top of the scar will be positioned below the top of the medial surface of the folds at the following increments: 0.5, 1.5, and 2.5mm (3 conditions). (4) The anterior-posterior length of the scar will be 2 mm, half the vocal fold length, and the full vocal fold length (3 conditions), always positioned mid-way between the anterior-posterior ends of the folds. Thus, we propose to simulate the size and position of the scar under a total of 72 conditions, contrasting all the conditions according to the vibration variables. Phonatory threshold pressure, acoustic intensity, and fundamental frequency will also be measured, along with all the vibratory variables enumerated in Aim 1 (A.3.1). Finally, the properties of the laryngeal scar will be correlated with the measured phonatory variables. The relationship of the six "vibration" variables to the four scar variables will be characterized with multiple regression. The same technique will be used to examine how scar characteristics affect the phonatory variables. D.2.2.2. Left-right asymmetry using a physical model. Vocal fold scarring can occur unilaterally or bilaterally. However, we have not yet systematically investigated the influence of a unilateral scar in any of our models because it requires the use of a full larynx model and asymmetry between the left and right vocal fold. Significantly, our new physical model allows us to phonate a full larynx just as easily as a hemilarynx . 43,44 Thus, for this experiment, we propose to repeat the scarring conditions explained in D.2.2.3 for the left vocal fold only. The right vocal fold will not be scarred. Thus, we will systematically investigate the influence of a unilateral scar on vocal fold vibration. The statistical analysis will be similar to that for Experiment D.1.2.1. This will allow us to estimate and compare the effect of bilateral versus unilateral scarring. D2.2.3. Optimization of a common phonosurgical treatment of scarring using a physical model. One condition we have not considered up to this point in our models is the underlying idea of mucosal slicing, in which a series of vertical scars interrupts the anterior-posterior fibrotic tension while at the same time allowing mucosal wave propagation up the medial surface of the folds (at least in the non-scarred regions). Indeed, a systematic laboratory investigation has never been conducted to contrast this type of vertical scarring with 1 long longitudinal scar near the vocal fold edge. By applying an adhesive to the medial surface of the physical model for the 2 different conditions, we will compare these 2 techniques. We will use ANOVA to examine differences between vertical and longitudinal scarring. D.2.3 Excised-Larynx Model of Vocal Fold Vibration The general methods for excised-larynx experiments have already been described (Method G). Although scars cannot be simulated as precisely and systematically on an excised larynx as on a physical model or computational model of vocal fold vibration, one advantage of the excised larynx is that it is a closer representation of the intact human larynx than the other models. For this reason, the excised larynx can help bridge the gap between laboratory and clinical observations. Thus, we propose to phonate a variety of excised larynges, using specimens from humans, dogs, pigs, and rats. Scars will be induced on human, porcine, and rat larynges using trichloracetic (TCA) acid, as described in earlier work .13 The naturally occurring sulci or scars found on canines will also be studied . 14,13,35 The main focus of our new in vitro and in vivo studies will be to repeat our previous studies using new non-invasive measures of tissue histology and viscoelasticity. Tissue histology will be measured using OCT (Method C) and tissue viscoelasticity will be measured using LSR (Method F). On the excised larynx, we will attempt to simulate the size and position of the sulcus for the same 72 conditions mentioned for the physical model using TCA acid as described in earlier work 13 and our preliminary studies, using human larynges for all conditions, but porcine and rat larynges for a subset of the conditions. We will also examine naturally occurring sulci on 12 different canine specimens. In all of the experiments, the viscoelasticity and the extent of the induced (or naturally occurring) scar will be measured using LSR and OCT, respectively. Phonatory threshold pressure, acoustic intensity, and fundamental frequency will also be measured, along with all the vibratory variables enumerated in Aim 1 (A.3.1). Finally, the properties of the laryngeal scar will be correlated with the measured phonatory variables. The relationship between scar characteristics and the viscoelastic and phonatory responses will be examined with multiple regression models. D.2.4. Homeostasis of Extracellular Matrix Components D.2.4.1. In vitro studies. In our series of studies designed to characterize the ECM structure of the lamina propria, we will use these specimens: (1) human vocal folds from autopsy cases and canine vocal folds from dogs with kennel cough, (2) rats at different ages and genders (previous work completed on young male rats by Tateya et al 23 will be duplicated on old male rats and both young and old female rats), (3) rats having vocal fold wounds from videolaryngoscopic surgery (Method A). The methods used will be those developed during the previous 5 years. Immunohistochemistry and electron microscopy (Method B) will be used to reveal the distribution and the fine structure of collagen subtypes, elastin, and SLRPs in humans, canines, and rats. Using rat specimens, we will perform real-time RT-PCR to examine the homeostasis of collagen, HA, and SLRPs in detail, and in situ hybridization will be performed to locate the cells that produce ECM components in normal and scarred vocal folds (Method E). Analysis of Variance models (ANOVA) will be used to examine differences in homeostasis between e.g. sex or age. D.2.4.2. Establishing an in vitro inflammation model of vocal fold fibroblasts. To examine the effect of various factors on reducing inflammation, we will establish an in vitro inflammation model of vocal fold fibroblasts. At first, we will determine the effect of introducing pro-inflammatory or pro-apoptotic factors on the cells of the vocal fold. Rats will be humanely euthanized (Method A), vocal fold lamina propria will be collected from vocal folds under a microscope, and the specimens will be placed in a Petri dish and chopped into pieces. The tissues will then be incubated in Dulbecco’s modified Eagle’s medium (DMEM, Invitrogen, Carlsbad, CA) containing 10% fetal bovine serum (FBS, Invitrogen, Carlsbad, CA), penicillin (10,000 IU, Invitrogen, Carlsbad, CA), streptomycin (10,000μg/mL, Invitrogen, Carlsbad, CA), and amphotericin B (25μg/mL, Invitrogen, Carlsbad, CA) in an incubator containing 5% carbon dioxide and 95% air at 37oC. Fibroblasts at first passage will be subcultured in 6cm dishes and incubated with DMEM and 10% FBS in an incubator containing 5% carbon dioxide and 95% air at 37oC. After 90 to 100% confluence, the medium will be replaced by a non-serum medium (AIM-V Media, Invitrogen, Carlsbad, CA). After incubating for 2 days, tumor necrosis factor (TNF)-alpha, interferon-gamma, and nuclear factor (NF) kappa-B will be added into each dish. The cell sample will be collected after culturing for 0, 3, 6, 12, and 24 hours. The culture medium will also be collected from each sample and used for ELISA study (Method D) to analyze HA concentration. Total RNAs will be extracted from the cells and reverse transcription will be performed to obtain first strand cDNA. COX-2 mRNA expression will be examined by real-time PCR (Method E). The pro-inflammatory factor that stimulates COX-2 expression most strongly will be used as an initiation factor of the in vitro inflammation model. Collagen type I/III/HA synthase expression and apotosis will also be monitored by real-time PCR. Subsequently, the effect of introducing selected factors in the presence of elevated levels of HA will be determined in order to examine the effect of high HA levels on the inflammation process. Again, collagen type I/III/HA synthase expression and apotosis will be monitored. As the last step, growth factors, such as HGF, will be applied after initiating the in vitro inflammation model, and the effect will be examined in terms of COX-2 expression and HA production. The relationship between COX-2 expression and outcome of the inflammation model in terms of HA concentration will be clarified. After establishing an in vitro inflammation model, different factors will be applied to examine their effect on reducing inflammation. In order to account for nesting in the experimental structure, linear mixed effect models will be used to examine the inflammation reduction of the different growth factors. D.2.4.3. Optimizing the dosage, timing, and type of growth factor used in treating acute or chronic vocal fold scars. To determine the ideal dosage and timing of HGF and bFGF, drugs will be injected into acute (3 days postoperatively) or chronic (2 months postoperatively) scarred rat vocal folds at different concentrations (10ng, 100ng, and 200ng). The injection will be repeated at different times (once/week x 1 and 5 times). The effects in preventing or reducing a scar will be examined by histology, rheology, and excised-larynx study. The results will be used to determine the most appropriate way of administering these treatments and serve as the bases for further studies. Three hundred and fifty-five Sprague-Dawley male rats (400-450g in weight) will be involved in the proposed studies. Rat vocal fold stripping will be performed (Method A). The other side will be kept intact and used as a control. Five percent of the rats will be randomly selected and sacrificed 1 day following surgery to histologically confirm the injury. The remaining rats will be randomly divided into 28 groups, each group consisting of 12 rats. The variables of interest defining the groups include: type of scar, acute (3 days postoperatively) or chronic (2 months postoperatively); material injected (PBS, bFGF, or HGF), volume of drug injected (10ng, 100ng, or 200ng); and number of injections (ranging from 1 to 5 times). Ten microliters of PBS, HGF (10ng, 100ng, or 200ng in 10μL of PBS, Sigma-Aldrich, St. Louis, MO), or bFGF (10ng, 100ng, or 200ng in 10μL of PBS, Sigma-Aldrich, St. Louis, MO) will be injected into the scarred vocal fold of each group. Injections will be given weekly for 1 or 4 weeks using a 27G Hamilton’s syringe (Hamilton, Reno, NV) under videolaryngoscopy. The rats will be humanely sacrificed 2 months after the last injection. Whole larynges will be harvested and used for histologic, rheologic, and aerodynamic examination. We will use Alcian blue stain, EVG stain, and immunohistochemistry to evaluate hyaluronic acid, collagen, and elastin. For rheologic examination, larynges will be examined by LSR. PTP values and vocal fold vibration amplitude will be analyzed by excised-larynx study (see Methods B, C, F, and G). The histological, rheology, and aerodynamic data will be analyzed with ANOVA models. With twelve rats per group, we will be able to find a standardized treatment difference of 1.20 with 80% power using a two-sided two-sample t-test at a 5% significance level. Power increases to 90% for a standardized treatment difference of 1.39. D.2.4.4. Achieving a long-lasting effect from growth factors. Methodology to improve the longevity of locally administered growth factors will be developed after the best combination of growth factors has been determined. Recently, gelatin-embedded HGF has demonstrated a long-lasting effect.54,90 This compound is gradually digested in the tissue and remains there for 1 to 2 months. Using an animal model (see Method A), we will inject the scarred vocal folds with gelatin-embedded growth factor, and the effects will be examined by histology, rheology, and excised-larynx study (Methods B, C, F, and G) The longevity of the growth factor effect will be examined via ANOVA, by comparing gelatin-embedded growth factor delivery against the standard injections. D.2.5. Strategies to Prevent Scarring and Promote Regeneration D.2.5.1. Gene therapy: in vivo electroporation. Rats will undergo unilateral vocal fold stripping and be divided into 7 groups: PBS, enhanced green fluorescence protein (EGFP), EGFP-Has1, EGFP-Has2, EGFP-bFGF, EGFP-HGF, and EGFP-EGF groups. For these 7 groups, phosphate-buffered saline, and 6 kinds of recombinant plasmid DNA-encoding-enhanced green fluorescence protein — EGFP, EGFP-Has1, EGFPHas2, EGFP-bFGF, EGFP-HGF, and EGFP-EGF — will be injected into the scarred vocal folds and electroporation will be performed to transfect these genes. Electroporation will be performed using the PulseAgile electroporation system (Model PA-4000) with a programmable pulse switch (Model PA-201) (Cyto Pulse Sciences, Inc., Columbia, MD) and a bipolar electrode placed on the superior and inferior surfaces of the vocal fold. Bidirectional transfection will be performed to maximize the efficacy of gene delivery. These procedures will be performed in the acute and chronic phase of injury. Rats will be sacrificed at several time points (2 weeks, 1 month, 2 months, and 3 months). The effects of these treatments will be examined by Alcian blue staining (HA detection), trichrome staining (collagen), and immunohistochemistry for collagen subtypes (Method B, C). Excised-larynx (Methods F, G) acoustic and aerodynamic parameters will also be used to analyze the treatment effects. The efficacy of electroporation will be examined to validate the results obtained. Transfected cells will be detected histologically by means of immunohistochemistry using an anti-EGFP antibody. mRNA expression of EGFP and target genes will also be examined by real-time RT-PCR (Method E). The gene that shows the best results will be used for a naked DNA injection study. For this study, we will need 340 rats to ensure adequate statistical power for the treatment and control groups. The 340 rats will include 25 normal control rats that will receive neither injury nor treatment. The remaining 315 rats will undergo unilateral vocal fold stripping and be randomly divided into the 7 groups listed above (PBS, EGFP, EGFP-Has1, EGFP-Has2, EGFP-bFGF, EGFP-HGF, and EGFP-EGF). For these 7 groups, PBS and 6 kinds of recombinant plasmid DNA-encoding-enhanced green fluorescence protein — EGFP, EGFP-Has1, EGFP-Has2, EGFP-bFGF, EGFP-HGF, and EGFP-EGF — will be injected into scarred vocal folds respectively and electroporation will be performed to transfect these genes. These procedures will be performed 5 days after vocal fold stripping. Rats will be sacrificed at 3 time points: 10 days, 4 weeks, and 8 weeks after vocal fold stripping. The effects of treatment will be examined by the same method described above. This study has n=15 for each time point of each of 7 treatment methods. ANOVA models will be used to examine the effects of the different gene therapy groups. With n=15 rats per group, we will be able to find a standardized treatment difference of 1.06 with 80% power using a two-sided twosample t-test at a 5% significance level. Power increases to 90% for a standardized treatment difference of 1.23. D.2.5.2. Naked DNA injection. Work in several laboratories has shown that naked plasmid DNA (pDNA) can be delivered efficiently to cells in vivo and has great prospects for basic research and gene therapy .87,88 Naked DNA injection is less invasive than electroporation and other gene-delivery methods, and it appears to be the most ideal way to deliver gene therapy for scarring. The rats in our experiment will undergo unilateral vocal fold stripping (Method A), and they will be injected with naked DNA in the acute and chronic phase of injury. The rats will be euthanized at several time points (2 weeks, 1 month, 2 months, and 3 months after injection), and the effects of treatment will be examined by histology, rheology, and excised-larynx study (Methods B, C, F, and G). The efficacy of electroporation will also be examined to validate the results obtained, as described above. The efficacy of naked DNA injection in the eight gene therapy groups will be examined with ANOVA models. With n=12 rats per group, we will be able to find a standardized treatment difference of 1.20 with 80% power using a 2-sided 2-sample ttest at .05 significance. Power increases to 90% for a standardized treatment difference of 1.39. D.2.5.3. Cell transplantation: fibroblasts. Fibroblasts in the scarred tissue are altered in terms of their ability to synthesize ECM.49 Fibroblast injection into the scarred vocal fold has been suggested as an alternative therapy to regenerate the vocal fold.72 The most important issues associated with this therapy are related to which fibroblast should be used and how to control the fibroblasts because the functions of various types of fibroblasts (vocal fold fibroblasts, skin fibroblasts, and scar fibroblasts) may be different. Therefore, we will characterize the functions of vocal fold, skin, oral mucosa, and scar fibroblasts in vitro in terms of ECM production and the properties of proteins. Two months after unilateral vocal fold stripping, the vocal fold lamina propria will be collected from normal and scarred vocal folds under microscope dissection, and the specimens will be placed in a Petri dish and chopped into pieces. Samples from skin and oral mucosa will also be collected as controls. The tissues will then be incubated in Dulbecco’s modified Eagle’s medium (DMEM, Invitrogen, Carlsbad, CA) containing 10% fetal bovine serum (FBS, Invitrogen, Carlsbad, CA), penicillin (10,000 IU, Invitrogen, Carlsbad, CA), streptomycin (10,000μg/mL, Invitrogen, Carlsbad, CA), and amphotericin B (25μg/mL, Invitrogen, Carlsbad, CA) in an incubator containing 5% carbon dioxide and 95% air at 37oC. Fibroblasts at first passage will be subcultured in 6cm dishes and incubated with DMEM and 10% FBS in an incubator containing 5% carbon dioxide and 95% air at 37oC. After 90 to 100% confluence, the medium will be replaced by a non-serum medium (AIM-V Media, Invitrogen, Carlsbad, CA). After incubating the fibroblasts for 2 days, the cell samples will be collected after culturing for 0, 3, 6, 12, and 24 hours. The culture medium will also be collected in each sample and is used for ELISA study. Total RNAs will be extracted from the cells and reverse transcription will be performed to obtain first strand cDNA. The production of HA, collagen, elastin, fibronectin, and decorin will be examined using ELISA and real-time PCR (Methods D and E). For protein analysis, protein will be extracted from fibroblasts from oral mucosa, skin tissues, and normal and scarred vocal folds. Two-dimensional sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS-PAGE) will be performed to characterize the fibroblasts in terms of protein properties. The raw data will be analyzed by Melanie software (Swiss Institute of Bioinformatics, Geneva, Switzerland), and the spots that show a significant difference will be identified by amino-acid sequencing. As a second step, we will examine the effects of growth factors and cytokines on each fibroblast in cell culture in terms of alteration of ECM production. Growth factors will be applied to cultured fibroblasts from oral mucosa, skin tissue, and normal and scarred vocal folds. ELISA and real-time PCR will be performed to examine the effect of growth factors on each cell line (Methods D and E). We will then determine the cell line that shows similar characteristics to those of normal vocal folds and that produces appropriate ECM components for transplantation. As a third step, we will obtain fibroblasts from an animal model, culture them, and implant them into the scarred vocal fold of the animal. The effects will be clarified using histology, rheology, and excised-larynx studies of vocal fold vibration (Methods B, C, F, and G). As the last step, we will implant fibroblasts into the scarred vocal fold in an animal model and administer regulatory factors (growth factors, naked DNA, etc.) to control the exogenous fibroblasts. The effects will be clarified using histology, rheology, and vibratory examinations (Methods B, C, F, and G). Differences between the twelve groups in the data from ELISA and PCR (Methods D, E) will be examined via linear mixed effect models, to account for nesting due to the different culture periods. With twelve rats in each of twelve groups, we will be able to find a standardized treatment difference of 1.20 with 80% power using a two-sided two-sample t-test at a 5% significance level. Power increases to 90% for a standardized treatment difference of 1.39. D.2.5.4. Cell transplantation: stem cells. Mesenchymal stem cells will be cultured and various growth factors and cytokines will be added. We will examine how best to induce MSCs and differentiate them into other cells. The functions of the MSCs in terms of ECM production will be demonstrated by ELISA and real-time PCR. The effects of MSC implantation into the scarred vocal fold will be examined in an animal model. A combination of growth factors will be administered. The effects will be assessed with histologic, rheologic, and excised-larynx studies (Methods C, F, and G). Differences between growth factors will be modeled with ANOVA. With twelve rats per group, we will be able to find a standardized treatment difference of 1.20 with 80% power using a twosided two-sample t-test at a 5% significance level. Power increases to 90% for a standardized treatment difference of 1.39. D.2.5.5. Tissue engineering. Fibroblasts will be seeded on the polymer in cell-culture dishes, and growth factors will be added to induce the production of appropriate ECM components for each layer. Growth factors will be determined based on the results of the experiment described in D.5.3. After an adequate incubation period, the sheets will be laid and tissue-engineered lamina propria will be made after further incubation. The engineered lamina propria will be examined by histology (Method C) focusing on the organization of ECM. Rheologic examination will clarify the viscoelasticity of the vocal fold (Method F). With twelve rats in each of three groups, power is the same as in D.2.5.4. D.2.5.6. Pulsed dye laser trials. Two introductory trials of the PDL will be performed to understand the effects of PDL energy levels and the number of PDL applications on tissue changes in rat vocal folds in the chronic scar model (Method A, I). Rats that have undergone surgical damage to 1 vocal fold and have survived for 2 months from injury will be selected for these tests. First, we will use the PDL to check that the energy being applied is less than the energy necessary to produce immediate tissue destruction. Then, using a fixed number of pulses and a fixed level of energy per pulse being delivered from the unit in a given session, we will use different rat groups to test for tissue changes as the distance of the fiber tip from the surface of the test vocal fold increases. Distances from the vocal folds will be 3, 6, 9, 15, and 20mm. Thus, 5 groups will be used, each group having 2 rats. Two scarred but untreated rats will be used as controls. Each test rat will undergo only 1 PDL application session. One month after the last PDL application, each rat will be euthanized and the larynx subjected to analysis using excised-larynx vibration, LSR, histology, and ELISA testing (see Methods G, F, A, C, and D). Second, the effect of serial PDL applications to chronically scarred rat vocal folds will be tested. Four test groups, each with 3 scarred rats, will be subjected to PDL applications in the manner described above. Two scarred, untreated rats will serve as controls. The number of pulses, amount of energy per pulse, and distance of the fiber tip from the vocal fold surface will be determined from experience in the first PDL experiment. These variables will be kept constant. The 4 test groups will undergo 1, 2, 3, and 4 total PDL applications respectively, with 3 weeks between each application. One month after the last PDL application, each rat will be euthanized and the larynx subjected to analysis using the excised-larynx platform, LSR, histology, and ELISA testing (Methods B, G, F, A, C, and D). In the tests to ensure tissue destruction does not occur, tissue changes due to energy, pulses, and distance from the vocal folds will be modeled with regression analysis. With three rats per group in the non-control groups, we will be able to find a standardized treatment effect of 3.07 with 80% power using a two-sided two-sample t-test at a 5% significance level. Power increases to 90% for a standardized treatment difference of 1.39. TIMELINE YEARS Aim 1: Measure and contrast the histologic, viscoelastic and vibrational properties of the pre- and post-operative tissues associated with vocal fold scarring. Document any correlations which exist between these properties and the resultant acoustical signal. Efforts will be directed toward completion of Aim 1 throughout the five years of funding. Aim 2: Determine appropriate scaffolds, cells and growth factors to regenerate the scarred vocal fold, and examine their therapeutic effects. 2.1. Homeostasis of ECM components 2.1.1. Human vocal folds 1, 2 year 2.1.2. Animal 1, 2 year 2.1.3. Development and aging 1, 2, 3 year 2.1.4. In-vitro inflammation model of vocal fold fibroblasts 1, 2, 3 year 2.2. Development of growth factor therapy 2.2.1. Optimization of dosage, timing and a type of a growth factor for the treatment of acute/chronic vocal fold scar 1, 2, 3 year 2.2.2 Achieving a long-lasting effect of the growth factor 3, 4 year (2.2.3. Clinical trial) 2.3. Prevention of scar and regeneration 2.3.1. Gene therapy 2.3.1.1. In-vivo electroporation 1, 2 year 2.3.1.2. Naked DNA injection. 2, 3, 4, 5 year 2.3.2. Cell transplanation 2.3.2.1. Use of fibroblasts 1, 2, 3, 4 year 2.3.2.2. Use of stem cells 3, 4, 5 year E. HUMAN SUBJECTS Non Applicable. F. VERTEBRATE ANIMALS 2. Justify use of animals selected in the proposed study: The use of experimental animals is required in the present research, as our other models of investigation, such as computer modeling would not allow us to look at the effects of treatment approaches or stages of wound repair. Also clinical studies would not allow us to make systematic changes in timing, magnitude and combinations of treatments necessitating the use of animals. Our particular strain of rat was chosen for this research because it is sufficiently large that the larynx can be easily visualized for vocal fold stripping, vibration patterns can be documented with acoustic, aerodynamic and high speed imaging, and OCT measures of the viscoelasticity can also be obtained. A rat model was chosen for analysis due to the investigators technical expertise with rats, and a number of scientific considerations. First, the rat has a short life span, with median lifespan of 36 months. As such, physiological and morphological changes associated with scarring can be realized in a relatively short period of time. Second, the ease of handling rats allows rigorous experimental control and measurement of multiple parameters, and examination of the relationships among variables. Third, the rat is ubiquitous in biomedical research. When developing interpretations of our findings, we can draw upon the work of others in a large knowledge base. Rat models for studies of vocal fold tissue allow for a relatively straightforward comparison to data derived via study of human vocal folds because of similar characteristics in the lamina propria ECM, found abundantly in the literature. Accordingly, knowledge gained by our research can add to the available data on wound healing. Fifth, the relative magnitude of fibroblasts in these rodents corresponds to that typically reported for humans. As such, the rat model is relevant to changes observed in both the acute and chronic scar.. Statistical methods and power calculation have ensured that our sample size is adequate for the full cadre of animals and for a conservative estimate of the animal sample size incorporating potential loss (i.e., 80% of the sample used). The number of animals for each experiment was determined via statistical power calculations performed by Dr. Glen Leverson, the biostatistician consulting on this project. Based on 12 rats in each group, if a treatment causes the population mean to shift by at least 1.2 standard deviation units, we should have an 80% chance of declaring statistical significance (If the relative treatment effect is 1.2, 12 rats per group will yield a power of 0.8 if testing is done at the usual 5% critical level. The power was based on a pairwise contrast of two means in the ANOVA). Under most circumstances a shift of 1.2 standard deviation units is quite small so our design should be effective at detecting scientifically relevant effects. Based on these calculations we have determined that minimal number of animals necessary to address the questions posed. A summary table of how the animals will be allocated to the studies follows. Estimated number of animals for 5 year period (2005-10) 1 (human and canine) 2 (rat; age and gender) 3 (scarred rats) 4 (In-vitro inflammation) D2-2 (GF therapy) 1 (Optimization of GF) 2 (Long lasting effect) D2-3 1 (Gene (Prevension&regenerat therapy) ion) Number of groups Number rats/group Number of ra 4 12 48 2 12 24 2 12 24 6 12 72 4 12 48 1 (electroporation) 14 12 168 2 (naked DNA) 1 (fibroblasts) 8 12 12 12 96 144 2 (stem cells) 8 3 12 12 96 36 D2-1 (Homeostasis of ECM) 2 (Cell transplantation ) 3 (Tissue engineering) 756 .The animals will be humanly treated. They will be anesthetized with ketamine 35mg/kg and Xylazine 5mg/kg in an intramuscular injection. Animals will be placed on a operating table and the larynx exposed using a specially constructed laryngoscope. Once the larynx is visualized with a Zeiss operating scope. One vocal fold will be stripped and the contralateral fold left untreated for comparison. Animals will recover in their cages in the animal facility until a scar is formed. All post-op animals will be inspected daily for 7 days by the researcher for signs of distress. Animal caretakers at the facility also inspect animals twice daily. Any animals experiencing severe distress or pain will be sacrificed immediately (we do not expect this to be a common occurrence as the animals have tolerated the procedure well in our previous studies). Sacrifice will be carried out with the ketamine/Xylazine anesthesia previously described, followed by pentobarbital overdose. Once the animal has ceased respiration and heart beats, the larynx will be removed and prepared for histological , acoustical, aerodynamic, vibratory motion analysis and rheological analysis. 6.B. As previously stated we have chosen rats because of their relative low cost, wide availability, size, ability to visualize the larynx and ease of anesthesia and surgery. Although many laryngeal experiments have been performed in dogs, we feel that rats will provide us with sufficient information to study the laryngeal musculature without excessive cost. The numbers of animals proposed for the experiment is necessary to give statistically significant data and to allow a buffer for certain inevitable animal deaths with this laryngeal experiment. 6.C. Veterinary care will be provided by the UW Research Animal Resources Care (RARC) facility. All animals will be housed in the animal facility under the care of two full-time veterinarians and several trained animal care workers. All persons working with animals at the University of Wisconsin have passed a rigorous test on animal care guidelines and are certified by the facility before being allowed to handle animals. 6.D. All procedures have been reviewed and approved by the RARC as not causing undue pain or suffering to these animals. We are using standard surgical and euthanasia procedures recognized by the Animal Care Committee. The surgery is similar to a vocal fold biopsy procedures, which is commonly performed by the surgical supervisor, Dr. Charles Ford , in a clinical setting under local anesthesia with little patient discomfort. 6.E. Euthanasia will be performed on the animals using an overdose (.22mg/kg I.V.) of prentobarbital. This method has been selected because of the ease of administration and its proven usefulness for this purpose. It is consistent with recommendations of the Panel on Euthanasia of the American Veterinary Medical Association. G. LITERATURE CITED 1) Hirano M. Chevalier Jackson Lecture: Phonosurgery-Past, Present, Future. American bronchoesophageal Association, 1995. 2) Woo P, Casper J, Colton R, Brewer D. Diagnosis and treatment of persistent dysphonia after laryngeal surgery: a retrospective analysis of 62 patients. Laryngoscope 1994; 104(9):1084-1091. 3) 4) Benninger MS, Alessi D, Archer S, Bastian R, Ford C, Koufman J et al. Vocal fold scarring: current concepts and management. Otolaryngol Head Neck Surg 1996; 115(5):474-482. Thibeault S, Ford C. The scarred vocal fold. In: Ossoff R, Shapshay S, Woodson G, Netterville J, Eds. The Larynx. Philadelphia. Pa: Lippincott Williams and Wilkins. 2002:431-440. 5) Hirano S, Bless D, Heisey D, Ford C. Roles of hepatocyte growth factor and transforming growth factor beta1 in production of extracellular matrix by canine vocal fold fibroblasts. Laryngoscope 2003; 113(1):144-8. 6) Hirano S, Bless DM, Heisey D, Ford CN. Effect of growth factors on hyaluronan production by canine vocal fold fibroblasts. Ann Otol Rhinol Laryngol 2003; 112(7):617-24. 7) Hirano S, Bless DM, Rousseau B, et al. Fibronectin and adhesion molecules on canine scarred vocal folds. Laryngoscope 2003; 113(6):966-72. 8) Hirano S, Bless DM, Rousseau B, et al. Prevention of vocal fold scarring by topical injection of hepatocyte growth factor in a rabbit model. Laryngoscope 2004; 114(3):548-56. 9) Hirano S, Bless DM, Munoz-del-Rio A, Connor N, Ford CN. Therapeutic Potential of Growth Factors for Aging Voice. The Laryngoscope 114:2161-2167, 2004. 10) Hirano S, Bless DM, Nagai H, Rousseau B, Welham N, Montequin D, Ford CN. Growth Factor Therapy for Vocal Fold Scarring in a Canine Model. Ann Otol Rhinol Laryngol 113:777-785, 2004. 11) Hirano S, Bless DM, Massey R, Hartig G, Ford CN. Morphological and Functional Changes of Human Vocal Fold Fibroblasts with Hepatocyte Growth Factor. Ann Otol Rhinol Laryngol 112:1026-1033, 2003 12) 13) 14) 15) 16) 17) 18) 19) 20) 21) 22) 23) 24) 25) 26) 27) 28) 29) 30) Hirano S, Hiromi N, Tateya I, Tateya T, Ford CN, Bless DM. Regeneration of Aged Vocal Folds with Basic Fibroblast Growth Factor in a Rat Model: a preliminary report. Ann Otol Rhinol Laryngol 114:304-308, 2005. Montequin D, Rousseau B, Bless D. Simulating a sulcus using TCA acid. Vocal Fold Physiology Conference, August 2004, Marseille, France. Montequin D, Rousseau B, Bless D. Naturally occurring vocal fold sulcus and edema in canine larynxes: an excised model. Submitted to Annals of Otol Rhino Laryng. Rousseau B, Hirano S, Scheidt TD, Welham NV, Thibeault SL, Chan RW, Bless DM. Characterization of vocal fold scarring in a canine model. Laryngoscope 2003;113:620-627. Rousseau B, Hirano S, Chan R, Welham NV, Thibeault SL, Bless DM, Ford CN. Characterization of chronic vocal fold scarring in a rabbit model. J. Voice 2004;18:116-124. Rousseau B, Sohn JH, Montequin DW, Tateya I, Bless DM. Functional Outcomes of Reduced Hyaluronan in Acute Vocal Fold Scar. Ann Otol Rhinol Laryngol 113:767776, 2004. Rousseau B, Tateya I, Lim X, Munoz-del-Rio A, Bless DM. Investigation of AntiHyaluronidase Treatment on Vocal Fold Wound Healing. Journal of Voice, 2005 Tateya T, Tateya I, Bless DM. Collagen Subtypes in Human Vocal Folds. (submitted) Tateya T, Tateya I, Sohn JH, Bless DM. Histologic Characterization of Rat Vocal Fold Scarring. Ann Otol Rhinol Laryngol 114:183-191, 2005. Tateya T, Tateya I, Sohn J, Bless DM. Histological study of acute vocal fold injury in a rat model. Ann Otol Rhinol Laryngol (submitted). Tateya I, Tateya T, Sohn JH, Watanuki M, Bless DM. Therapeutic Effect of Growth Factors on Chronic Vocal Fold Scarring in a Rat Model. (submitted) Tateya T, Tateya I, Munoz-del-Rio A, Bless DM. The Post-natal Development of Rat Vocal Folds. (in press 2005). Tateya I, Tateya T, Watanuki M, Bless DM. Homeostasis of Hyaluronic Acid in Normal and Scarred Vocal Folds. (submitted) Tateya I,Tateya T, Xinhong L, Sohn JH, Bless DM. Cell Production in Injured Vocal Folds: A Rat Study. (in press 2005). Thibeault S, Bless DM, Gray S. Interstitial Protein Alterations in Rabbit Vocal Fold with Scar. Journal of Voice 17:377-383, 2003. Thibeault SL, Gray SD, Bless DM, Chan RW, Ford CN. Histologic and rheologic characterization of vocal fold scarring. J Voice 2002;16:96-104. Thibeault SL, Rousseau B, Welham NV, et al. Hyaluronan levels in acute vocal fold scar. Laryngoscope 2004; 114(4):760-4. Welham, N. V., Rousseau, B., Ford, C. N., & Bless, D. M. (2003). Tracking outcomes after phonosurgery for sulcus vocalis: a case report. J Voice, 17(4), 571-8. Welham, N. V., Rousseau, B., Ford, C. N., & Bless, D. M. (2004). Perceptual, instrumental and psychosocial outcomes after surgery for sulcus vocalis. Poster presented at the Annual Meeting of the American Academy of Otolaryngology – Head and Neck Surgery, New York, NY, USA. 31) Chan RW, Titze IR. Hyaluronic acid (with fibronectin) as a bioimplant for the vocal fold mucosa. Laryngoscope 1999; 109(7 Pt 1):1142-1149. 32) Paniello RC, Dahm JD. Long-term model of induced canine phonation. Otolaryngol Head Neck Surg 1998; 118(4):512-522. 33) Garrett CG, Coleman JR, Reinisch L. Comparative histology and vibration of the vocal folds: implications for experimental studies in microlaryngeal surgery. Laryngoscope 2000; 110(5 Pt 1):814-824. 34) Riede, T. Vocal tract length and acoustics of vocalization in the domestic dog (canis familiaris), J. Exper Biology. 202: 2859-2968, 1999. Riede, T., Herzel, H., Mehwald, D., Seidner, W., Tumler, E., Bohme, G., Tembrock G., 35) Nonlinear phenomena in the natural howling of a dog+wolf mix. J Acoust Soc Am, 108:1435-1442, 2000> 36 Gray 2000 37) Gray SD, Titze IR, Chan R, Hammond TH. Vocal fold proteoglycans and their influence on biomechanics. Laryngoscope 1999; 109(6):845-854. Gray SD, Titze IR, Alipour F, Hammond TH. Biomechanical and histologic observations of vocal fold fibrous proteins. Ann Otol Rhinol Laryngol 2000; 109(1):77-85. Hertegard S, et al. Viscoelasticity in scarred rabbit vocal folds after hyaluronan injectionshort term results. AAO-HNSF/ARO Research Forum during the 2004 Annual Meeting of the American Academy of Otolaryngology-Head and Neck Surgery Foundation, NY, NY, September 19-22, 2004. 38) 39) 40) 41) 42) 43) 44) Hirano S, Bless D, Heisey D, Ford C. Roles of hepatocyte growth factor and transforming growth factor beta1 in production of extracellular matrix by canine vocal fold fibroblasts. Laryngoscope 2003; 113(1):144-8. Hirano S, Bless DM, Heisey D, Ford CN. Effect of growth factors on hyaluronan production by canine vocal fold fibroblasts. Ann Otol Rhinol Laryngol 2003; 112(7):617-24. Hertegard S, Hallen L, Laurent C, Lindstrom E, Olofsson K, Testad P et al. Crosslinked hyaluronan used as augmentation substance for treatment of glottal insufficiency: safety aspects and vocal fold function. Laryngoscope 2002; 112(12):2211-2219. Hallen L, Testad P, Sederholm E, Dahlqvist A, Laurent C. DiHA (dextranomers in hyaluronan) injections for treatment of insufficient closure of the vocal folds: early clinical experiences. Laryngoscope 2001; 111(6):1063-1067. Dang C, Ting K, Soo C, Longaker MT, Lorenz HP. Fetal wound healing current perspectives. Clinics in plastic surgery 2003; 30:13-23. 45) Hirano S, Bless DM, Rousseau B, et al. Fibronectin and adhesion molecules on canine scarred vocal folds. Laryngoscope 2003; 113(6):966-72. 46) Chan RW, Gray SD, Titze IR. The importance of hyaluronic acid in vocal fold biomechanics. Otolaryngol Head Neck Surg 2001; 124(6):607-14. Camenisch TD, Spicer AP, Brehm-Gibson T, et al. Disruption of hyaluronan synthase-2 abrogates normal cardiac morphogenesis and hyaluronan-mediated transformation of epithelium to mesenchyme. J Clin Invest 2000; 106(3):349-60. 47) 48) Toole BP. Hyaluronan is not just a goo! J Clin Invest 2000; 106(3):335-6. 49) Hellstrom S, Laurent C. Hyaluronan and healing of tympanic membrane perforations. An experimental study. Acta Otolaryngol Suppl 1987; 442:54-61. 50) Weindl G, Schaller M, Schafer-Korting M, Korting HC. Hyaluronic acid in the treatment and prevention of skin diseases: molecular biological, pharmaceutical and clinical aspects. Skin Pharmacol Physiol 2004; 17(5):207-13. Sato K, Hirano M, Nakashima T. Stellate cells in the human vocal fold. Ann Otol Rhinol Laryngol 2001; 110(4):319-25. 51) 52) Catten M, Gray SD, Hammond TH, et al. Analysis of cellular location and concentration in vocal fold lamina propria. Otolaryngol Head Neck Surg 1998; 118(5):663-7. 53) Shimizu T, Yamato M, Akutsu T, et al. Electrically communicating three-dimensional cardiac tissue mimic fabricated by layered cultured cardiomyocyte sheets. J Biomed Mater Res 2002; 60(1):110-7. Shimizu T, Yamato M, Kikuchi A, Okano T. Cell sheet engineering for myocardial tissue reconstruction. Biomaterials 2003; 24(13):2309-16. Hirano S, Thibeault S, Bless DM, Ford CN, Kanemaru SI. Hepatocyte Growth Factor and its Receptor C-Met in Rat and Rabbit Vocal Folds. Ann Otol Rhinol Laryngol 111:661-666, 2002. 54) 55) 56) 57) 58) 59) 60) 61) 62) 63) 64) 65) 66) 67) 68) 69) Hirano S, Bless DM, Rousseau B, et al. Prevention of vocal fold scarring by topical injection of hepatocyte growth factor in a rabbit model. Laryngoscope 2004; 114(3):548-56. Yang GP, Lim IJ, Phan TT, et al. From scarless fetal wounds to keloids: molecular studies in wound healing. Wound Repair Regen 2003; 11(6):411-8. Zhou LJ, Ono I, Kaneko F. Role of transforming growth factor-beta 1 in fibroblasts derived from normal and hypertrophic scarred skin. Arch Dermatol Res 1997; 289(11):646-52. Wilgus TA, Bergdall VK, Tober KL, et al. The impact of cyclooxygenase-2 mediated inflammation on scarless fetal wound healing. Am J Pathol 2004; 165(3):753-61. Ward P, Thibeault S, Gray S. Hylauronic Acid: its role in voice. J Voice. 2002,16:303=9 Titze IR. Phonation threshold pressure: a missing link in glottal aerodynamics. J Acoust Soc Am 1992; 91(5):2926-2935. Fisher KV, Swank PR. Estimating phonation threshold pressure. J Speech Lang Hear Res 1997; 40(5):1122-1129. Berry DA, Verdolini K, Montequin DW, Hess MM, Chan RW, Titze IR. A quantitative outputcost ratio in voice production. J Speech Lang Hear Res 2001; 44(1):29-37. Alipour, F., Berry, D.A., Titze, I.R. (2000). A finite element model of vocal fold vibration, J. Acoust. Soc. Am. 108, 3003-3012. Berry, D.A., Reininger, H., Alipour, F., Bless, D.M., Ford, C.N. (in press). The influence of vocal fold scarring on phonation: predictions from a finite element model, Annals of Otology, Rhinology, and Laryngology. Chan, R.W., Titze, I.R., and Titze, M.R. (1997). Further studies of phonation threshold pressure in a physical model of the vocal fold mucosa, J. Acoust. Soc. Am. 101, 37223727. Titze, I.R., Schmidt, S.S., and Titze, M.R. (1995). Phonation threshold pressure in a physical model of the vocal fold mucosa, J. Acoust. Soc. Am. 97, 3080-3084. Thomson, S.L., Mongeau, L., Frankel, S.H., Neubauer, J., Berry, D.A. (2004). Selfoscillating laryngeal models for vocal fold research, 8th International Conference on Flow-Induced Vibrations, Ecole Polytechnique, Paris, France. Thomson, S.L. (2004). Fluid-structure interactions within the human larynx, Ph.D. Dissertation, Purdue University, West Lafayette, IN. 70) Goodyer E, Gunter, H, Masaki A, and Kobler J. Mapping the visco-elastic properties of the vocal fold. Advances in Quantitative Laryngology. Voice and Speech Research, April 2003. 71) Hess M, Mueller F, Kobler J, Zeitels S, Goodyer E. Measurements of vocal fold elasticity using the linear skin Rheometer. Folia Phoniatrica 2005 (in press). 72) Berke G, Blumin J, Sebastian J, et al. Vocal cord augmentation with cultured autologous fibroblasts. Bull Exp Biol Med 2000; 130(8):790-2. 73) Ito W, et al. Hepatocyte grow factor attenuates airway hyperresponsiveness, inflammation and remodeling. Am J Respir Cell Jol Biol. 2004. Dec 30. Peacock EE. Wound Repair. Philadelphia: Saunders, 1984. Daher A, de Boer W, El-Marjou A et al. Epidermal growth factor receptor regulates normal urothelial regeneration. Lab Invest 2003; 83:1333-41. Kriesel K, Thibeault S, Chan RW, Suzuki T, VanGroll PJ, Bless DM, Ford CN. Treatment of Vocal Fold Scarring: Rheological and Histological Measures of Homologous Collagen Matrix. Ann Otol Rhinol Laryngol 111:884-889, 2002. Yan, Y., Ahmad, K., Kunduk, M., & Bless, D. M. (in press). Analysis of vocal-fold vibrations from high-speed laryngeal images using a Hilbert transform based. 74) 75) 76) 77) 78) Feldchtein, F.I., Gelikonov, G.V., Gelikonov, V.M., Kuranov, R.V., Sergeev, A.M., Gladkova, N.D., Shaknov, A.V., Sharkhova, N.M., Snopova, L.B., Terent’eva, A.B., Zagainova, E.V., Chumakov, Yu.P., Kuznetzova, I.A. (1998). Endoscopic applications of optical coherence tomography, Optics Express 3, 257-270. 79) 80) 81) 82) 83) 84) 85) 86) 87) 88) 89) 90) 91) 92) Shakhov, A.V., Terentjeva, A.B., Kamensky, V.A., Snopova, L.B., Gelikonov, V.M., Feldchtein, F.I., Sergeev, A.M. (2001). Optical coherence tomography monitoring for laser surgery of laryngeal carcinoma, J Surgical Oncology 77, 253-258. Luerssen, K., Lubatschowski, H., Ptok, M. (2005). Optical characterization of vocal folds with OCT, , Photonics West, Proceedings Vol. 5686, paper no. 73, San Jose, CA. Pierce, M., Strasswimmer, J., Park, B.H., Cense, B., de Boer, J.F. (2004). Advances in optical coherence tomography imaging for dermatology, J. Invest Dermatol 123, 458463. Hutchison, R., Sharp, T., Harberger, S., Lovec, R.J., Icenogle, T., Gheewala, N., Jackson, R.P., Guo, S., Haskell, R.C., Orwin, E., Wolf, R., Chen, Z., Wong, B.J. (2005). Office-based OCT imaging of the human larynx, Photonics West, Proceedings Vol. 5686, paper no. 134, San Jose, CA. Oakley B. A simplified ultra-sensitive sliver stain for detecting proteans. Anal biochem. 1980;105:361-3. Takebayashi K, Akazawa C, Nakanishi S, Kageyama R. Structure and promoter analysis of the gene encoding the mouse helix-loop-helix factor HES-5. Identification Jiang J. 2005 Newbauer, 2001 computational model Herweijer H, Wolff J. Progress and prospects: naked DNA gene transfer and therapy. Gene Ther 2003; 10:453-8., Wolff J, Budker V. The mechanism of naked DNA uptake and expression. Adv Genet. 2005; 54:3-20. Kanemaru S, Nakamura T, Omori K, et al. Regeneration of mastoid air cells: clinical applications. Acta Otolaryngol Suppl 2004(551):80-4. Tabata Y, Ikada Y. Vascularization effect of basic fibroblast growth factor released from gelatin hydrogels with different biodegradabilities. Biomaterials 1999; 20(22):216975., Burd A. Hyaluronan and scarring. In Garg HG, Hales CA, eds. Chemistry and biology of hyaluronan. San Diego: Elsevier, 2004. pp. 367-394. Bibas, A.G., Podoleanu, A.GH., Cucu, R.G., Bonmarin, M., Dobre, G.M., Ward, V.M.M., Boxer, A., Gleeson, M.J., Jackson, D.A. (2004). 3-D optical coherence tomography of the laryngeal mucosa. Clin. Otolaryngol. 29, 713-720. 93) Pierce, M.C., Klein, A., Park, B.H., Zeitels, S.M., de Boer, J.F. (2005), Endoscopic imaging of the human vocal cords using polarization-sensitive optical coherence tomography, Photonics West, Proceedings Vol. 5686, paper no. 68, San Jose, CA. 5) Thibeault S, Gray S, Li W, Ford CN, Smith M, Davis RK. Genotypic and Phenotypic Expressions of Vocal Fold Polyps and Reinke’s Edema: A Preliminary Study. Ann Otol Rhinol Laryngol 111:302-309, 2002. H. CONSORTIUM/CONTRACTUAL ARRANGEMENTS None I. CONSULTANTS See the attached letters from David Berry, Shigeru Hirano, Eric Goodyer, Bernard Rousseau, Susan Thibeault, Ichiro Tateya, and Tomoko Tateya. J. RESOURCE SHARING Non-applicable