Questions on Evdidence and science
advertisement
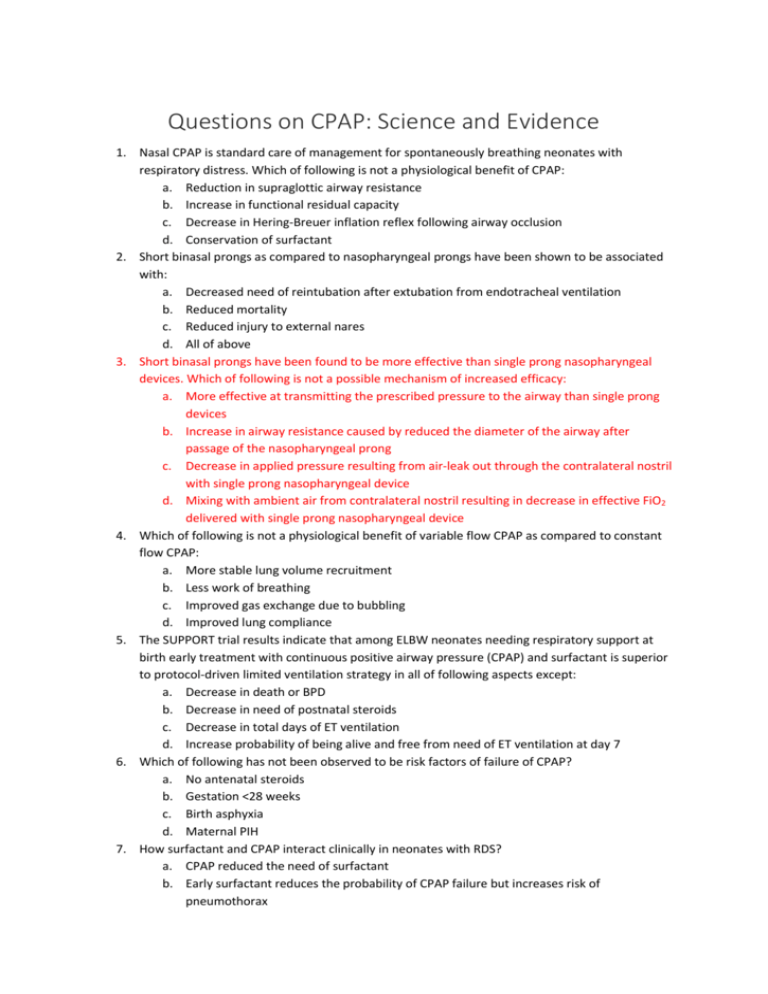
Questions on CPAP: Science and Evidence 1. Nasal CPAP is standard care of management for spontaneously breathing neonates with respiratory distress. Which of following is not a physiological benefit of CPAP: a. Reduction in supraglottic airway resistance b. Increase in functional residual capacity c. Decrease in Hering-Breuer inflation reflex following airway occlusion d. Conservation of surfactant 2. Short binasal prongs as compared to nasopharyngeal prongs have been shown to be associated with: a. Decreased need of reintubation after extubation from endotracheal ventilation b. Reduced mortality c. Reduced injury to external nares d. All of above 3. Short binasal prongs have been found to be more effective than single prong nasopharyngeal devices. Which of following is not a possible mechanism of increased efficacy: a. More effective at transmitting the prescribed pressure to the airway than single prong devices b. Increase in airway resistance caused by reduced the diameter of the airway after passage of the nasopharyngeal prong c. Decrease in applied pressure resulting from air-leak out through the contralateral nostril with single prong nasopharyngeal device d. Mixing with ambient air from contralateral nostril resulting in decrease in effective FiO2 delivered with single prong nasopharyngeal device 4. Which of following is not a physiological benefit of variable flow CPAP as compared to constant flow CPAP: a. More stable lung volume recruitment b. Less work of breathing c. Improved gas exchange due to bubbling d. Improved lung compliance 5. The SUPPORT trial results indicate that among ELBW neonates needing respiratory support at birth early treatment with continuous positive airway pressure (CPAP) and surfactant is superior to protocol-driven limited ventilation strategy in all of following aspects except: a. Decrease in death or BPD b. Decrease in need of postnatal steroids c. Decrease in total days of ET ventilation d. Increase probability of being alive and free from need of ET ventilation at day 7 6. Which of following has not been observed to be risk factors of failure of CPAP? a. No antenatal steroids b. Gestation <28 weeks c. Birth asphyxia d. Maternal PIH 7. How surfactant and CPAP interact clinically in neonates with RDS? a. CPAP reduced the need of surfactant b. Early surfactant reduces the probability of CPAP failure but increases risk of pneumothorax 8. 9. 10. 11. 12. 13. 14. c. None of the above d. Both of the above In a neonate ready to be weaned off from CPAP which of following is most suitable based on current best available evidence? a. Taken ‘OFF’ CPAP with the view to stay ‘OFF’ b. Cycled on and off CPAP with incremental time ‘OFF’ c. Alternating with nasal cannula d. All the methods are equal The systematic review on use of CPAP in neonates with respiratory distress demonstrated increased risk of pneumothorax with CPAP as compared to oxygen therapy (Number need to harm 7). Which of following statement is most correct? a. This increased risk can most likely be attributed to lack of exposure to antenatal steroids non-availability of surfactant. Therefore, in present era this risk is non-existent b. Neonates with normal to increased FRC continue to be at risk of pneumothorax if given CPAP and therefore CPAP should not be used in neonates with TTNB or MAS c. Pressure delivered with bubble CPAP varies with input air flow and can increase dangerously to cause pneumothorax if not monitored proximally d. Pneumothorax in neonates on CPAP is due to underlying disease and cannot be avoided CPAP machines should be available in special care neonatal units at district hospitals. Which of the following is true statement supporting this recommendation? a. Use of CPAP in neonates with respiratory distress decrease the need to up-transfer to higher center b. Availability of CPAP allows use of surfactant in these small hospitals c. Use of CPAP does not need extensive monitoring and therefore neonates on CPAP can be easily managed by nurses alone d. All of the above In which type of CPAP expiratory limb is open to environment? a. Bubble CPAP b. Ventilator CPAP c. Infant flow driver d. Indigenous CPAP Amount of gas flow is as an important determinant of CPAP delivery. Which of the following statement is most correct about gas flow? a. Infant flow driver needs low gas flow to maintain the distending pressure b. High flow in bubble CPAP can increase the work of breathing c. Adequacy of gas flow is difficult to determine with bubble CPAP d. Leak through open mouth does not alter the needed gas flow Which of following is not a possible side effect of use of inappropriately high pressure? a. Respiratory acidosis b. Metabolic acidosis c. Increased pulmonary blood flow leading to pulmonary hemorrhage d. None of the above Which of following is not true about gastrointestinal effect of CPAP? a. Tone of upper and lower esophageal sphincter is lower than CPAP and therefore air can easily enter stomach and cause CPAP belly b. Due to risk of CPAP belly, feeds should be introduced and increased very cautiously is neonates on CPAP c. 15. 16. 17. 18. 19. 20. CPAP can cause reflux of gastrointestinal contents and therefore neonates on CPAP should be nursed in head up position d. All of the above Which of following is not a contraindication to use of CPAP? a. Meconium aspiration syndrome b. Cleft palate c. Tracheoesophageal fistula d. Diaphragmatic hernia Which of following is possible advantage of heated-humidified high flow nasal cannula? a. Lesser nasal trauma b. Lesser chances of extubation failure c. Lesser pneumothorax d. All of the above Bi-level CPAP is a. Alternating high and low CPAP pressure during inspiration and expiration b. Alternating low and high CPAP pressure during inspiration and expiration c. Providing two alternating levels of CPAP in order to switch the functional residual capacity (FRC) of the neonate between two different levels d. Providing two different levels of CPAP before and after extubation Which of following patient interface is not commonly used to provide CPAP? a. Nasal mask b. Sealed oxygen hood c. Nasopharyngeal endotracheal tube d. Binasal prongs In an infant having good respiratory efforts which type of nasal CPAP is most likely to maintain constant pressure at the level of patient interface? a. Bubble CPAP b. Infant flow driver c. Ventilator CPAP d. Heated humidified high flow nasal cannula CPAP or intubation study (COIN) study compared nasal CPAP with intubation and ventilation among neonates born at less than 28 weeks of gestation. Incidence of pneumothorax was three times higher in CPAP group. In your view which factor was least likely to contribute to high incidence of pneumothorax in CPAP group? a. Use of high distending pressure of 8 cm water b. Decreased and delayed use of surfactant c. Not sedating neonates on nasal CPAP d. None of the above