Hereditary Colorectal Cancer Syndromes
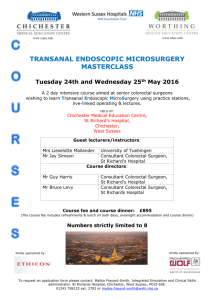
advertisement

Administrative Office St. Joseph's Hospital Site, L301-10 50 Charlton Avenue East HAMILTON, Ontario, CANADA L8N 4A6 PHONE: (905) 521-6141 FAX: (905) 521-6142 http://www.fhs.mcmaster.ca/hrlmp/ Issue No. 68 QUARTERLY NEWSLETTER April 2003 Hereditary Colorectal Cancer Syndromes Genetics centres across the province have coordinated the implementation of clinical and laboratory services for hereditary colorectal cancer syndromes. As a result, a new requisition form will be used to refer patients for laboratory testing. This form itemizes the clinical criteria to be considered. Counselling is offered at the Hamilton Regional Cancer Centre and at the McMaster site of Hamilton Health Sciences. For information in regard to referral of patients for counselling, risk assessment, laboratory testing, or clinical management, please call 905-521-5085, or fax 905-521-2651. The two major syndromes associated with hereditary colorectal cancer are HNPCC and FAP. HNPCC (hereditary nonpolyposis colorectal cancer) is caused by inheritance of mutations in any of several genes involved in DNA mismatch repair mechanisms; the major two genes are MLH1 and MSH2, but others include MSH6, PMS1, and PMS2. The proteins produced from these genes form a complex that excises and repairs mismatched nucleotides in DNA. Mutations of these genes are somewhat variable in clinical severity, depending upon which protein is affected and the type of mutation. HNPCC is the most common type of hereditary colorectal cancer, and is thought to account for about 6 – 8% of all colorectal carcinomas. The predominant pattern of clinical expression is unusually early onset of one or more polyps in the ascending (right) side of the colon, leading to colorectal carcinoma in a high proportion of mutation carriers. Other types of cancer may also be found in the family history, including pancreatic, uterine, or brain cancer (a more complete list is provided in Table 1). The mechanism of tumour formation is a defect in DNA repair, leading to an increased rate of accumulation of mutations throughout the genome, including oncogenes and tumour suppressor genes involved in the pathway to colorectal carcinogenesis. Diagnostic assessment includes a detailed review of the family history, confirmation of pathologic diagnosis of any suspected cancers, and then laboratory assessment of pathological specimens according to established selection criteria and analytical algorithms. Currently, laboratory testing has not been implemented in the Hamilton region, but we refer specimens to other test centres (principally Mount Sinai Hospital in Toronto). Reporting times have not been established. Informed consents are needed to initiate testing, which starts by obtaining paraffin blocks of tumour tissue from critical persons identified in the review of the family history. DNA is extracted from the pathological specimens and a molecular technique that screens for a specific type of defect in DNA repair (the Microsatellite Instability test) is applied. Immunohistochemistry (IHC) for the MSH1 and MLH2 proteins is also commonly applied. For specimens that are positive by either screening test, workup proceeds to include extensive molecular sequencing of the suspected gene(s) for specimens. Patients at high risk for HNPCC are offered a variety of options for increased surveillance and clinical management. Also, patients may be eligible to participate in a research study. Dr. Ed Chouinard of the Hamilton Regional Cancer Centre is participating in a multi-centre clinical study coordinated by the Ontario Cancer Genetics Network. The Hamilton Laboratory is planning to develop MSI and IHC services by the fall of 2003. Familial adenomatous polyposis coli (FAP) is the second major syndrome associated with hereditary colorectal carcinomas. FAP is relatively rare, accounting for less than 1% of all cases of colorectal cancer, and caused by mutations of the APC gene. Mutation carriers develop large numbers of polyps in the large colon and rectum, with the first polyps often detected in the mid-teens; one or more polyps progress to carcinomas with virtually all carriers receiving a diagnosis of cancer by age 40 if intervention does not occur. Clinical counselling includes a review of the family history and confirmation of pathological records. Testing is provided by Mount Sinai Hospital in Toronto. Clinical management for carriers primarily consist of increased surveillance for polyp formation followed by colostomy when necessary. The major clinical criteria for referral for these two colorectal cancer syndromes are summarized in the following table. Sydrome Criteria for Referral for Genetics Counselling HNPCC Multiple cancers in family fit HNPCC spectrum, with at least one relative with colorectal or endometrial cancer; especially if at least one diagnosis at <50 yrs and in more than one generation Colorectal cancer at <35 yrs Multiple primary cancers in HNPCC spectrum in one family member Family member with a colonic adenoma or cancer and abnormal Microsatellite Instability screen result Family member with documented mutation of an HNPCC gene Tumor spectrum: colorectal, gastric, small bowel, hepatobiliary, pancreatic, endometrial, ovarian, renal, ureteral, sebaceous carcinoma, brain FAP Family member with FAP, or with at least 10 histologically confirmed adenomatous polyps (i.e. suggestive of attenuated FAP variant) Family member with a known mutation causing FAP Hereditary Breast/Ovarian Cancer In January 2003, Minister of Health Tony Clement announced new funding to improve the diagnostic accuracy of laboratory testing for hereditary breast/ovarian cancer. This money will be used to implement DHPLC (denaturing high performance liquid chromatography) as a screening methodology for detecting mutations of the BRCA1 and BRCA2 genes. The current test protocol depends upon a protein truncation assay to screen for mutations. DHPLC, in comparison to the protein truncation test, is expected to detect a significantly higher proportion of all mutations at a lower cost per specimen and higher throughput. Evaluation and implementation of DHPLC will take about a year, because the new test will be added in parallel to the existing methodology to ensure that all test results are properly interpreted and analyzed. During the evaluation phase, the DHPLC testing will be coded and performed blindly; test results will be opened and analyzed at several points during the study. Therefore, a small proportion of patients may receive a supplemental report revising their test result based upon new information from the DHPLC studies. In recognition of this potential impact on counselling and clinical management, patient participation is optional; all patients will receive informed counselling about the DHPLC study and will sign a consent form if they wish to participate. We are also adding another test protocol for BRCA1. A new kit is available, commonly called the MLPA kit, which quickly and accurately detects large genomic deletions and duplications, such as loss or gain of whole exons. This kit provides a quick and definitive test for rearrangements that could only be detected previously by a slower Southern blot method. Dr. R. Carter Discipline Director - Genetics Hamilton Regional Laboratory Medicine Program McMaster University Medical Centre