Eszopiclone
advertisement
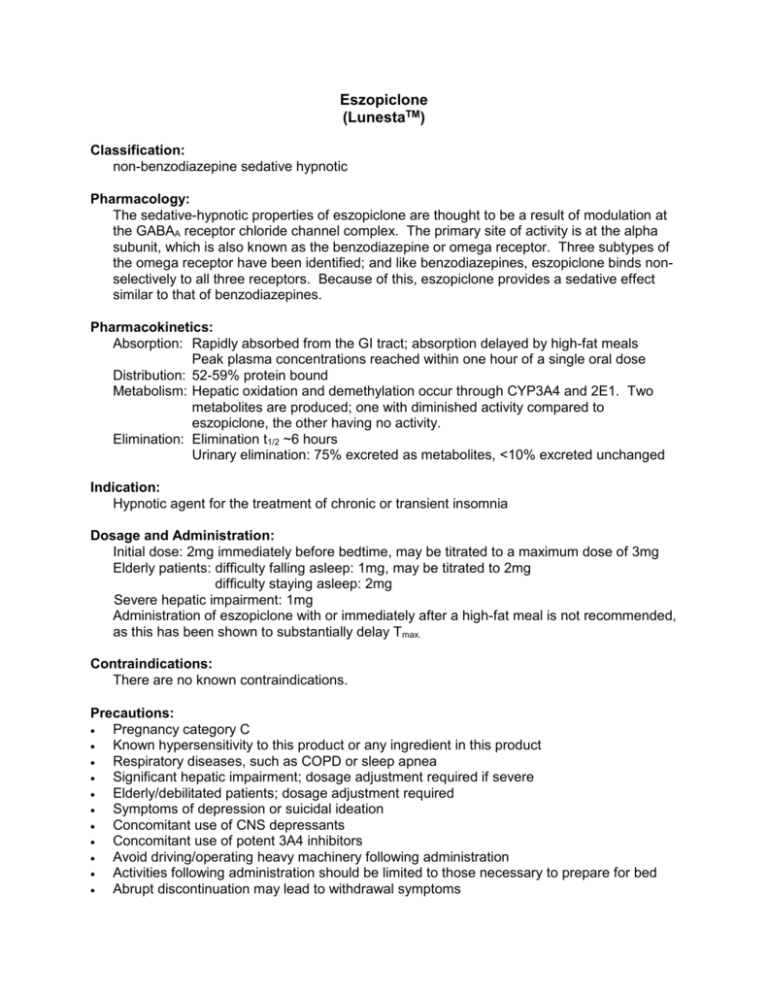
Eszopiclone (LunestaTM) Classification: non-benzodiazepine sedative hypnotic Pharmacology: The sedative-hypnotic properties of eszopiclone are thought to be a result of modulation at the GABAA receptor chloride channel complex. The primary site of activity is at the alpha subunit, which is also known as the benzodiazepine or omega receptor. Three subtypes of the omega receptor have been identified; and like benzodiazepines, eszopiclone binds nonselectively to all three receptors. Because of this, eszopiclone provides a sedative effect similar to that of benzodiazepines. Pharmacokinetics: Absorption: Rapidly absorbed from the GI tract; absorption delayed by high-fat meals Peak plasma concentrations reached within one hour of a single oral dose Distribution: 52-59% protein bound Metabolism: Hepatic oxidation and demethylation occur through CYP3A4 and 2E1. Two metabolites are produced; one with diminished activity compared to eszopiclone, the other having no activity. Elimination: Elimination t1/2 ~6 hours Urinary elimination: 75% excreted as metabolites, <10% excreted unchanged Indication: Hypnotic agent for the treatment of chronic or transient insomnia Dosage and Administration: Initial dose: 2mg immediately before bedtime, may be titrated to a maximum dose of 3mg Elderly patients: difficulty falling asleep: 1mg, may be titrated to 2mg difficulty staying asleep: 2mg Severe hepatic impairment: 1mg Administration of eszopiclone with or immediately after a high-fat meal is not recommended, as this has been shown to substantially delay Tmax. Contraindications: There are no known contraindications. Precautions: Pregnancy category C Known hypersensitivity to this product or any ingredient in this product Respiratory diseases, such as COPD or sleep apnea Significant hepatic impairment; dosage adjustment required if severe Elderly/debilitated patients; dosage adjustment required Symptoms of depression or suicidal ideation Concomitant use of CNS depressants Concomitant use of potent 3A4 inhibitors Avoid driving/operating heavy machinery following administration Activities following administration should be limited to those necessary to prepare for bed Abrupt discontinuation may lead to withdrawal symptoms Interactions: Eszopiclone is a substrate of 3A4 (major) and 2E1 (minor). Inhibitors of CYP3A4 (i.e. ciprofloxacin, clarithromycin, doxycycline, erythromycin, fluoxetine, fluvoxamine, isoniazid, protease inhibitors, verapamil) can significantly increase the levels and effects of eszopiclone. Likewise, inducers of CYP3A4 (i.e. carbamazepine, phenobarbital, phenytoin) can decrease the levels and effects of eszopiclone. Concomitant use of ethanol or other CNS depressants can increase the risk of sedation. Adverse Reactions: Sleep related behaviors such as sleep-driving, sleep-walking, eating while sleeping, or making phone calls while sleeping may possibly be experienced while taking eszopiclone. Other side effects include headache, unpleasant taste, somnolence, dizziness, nervousness, depression, hallucinations, rash, and xerostomia. Cost comparison of sedative-hypnotics: Generic Name Brand Name eszopiclone Lunesta® zaleplon Sonata® zolpidem Ambien® Strength 1, 2, 3mg 5mg 5mg Unit Price $4.09 $2.67 $0.05 Shape Round tablet Round tablet Round tablet Imprint S190 S191 S193 Monitoring Parameters: No standard monitoring is required. Product Identification: Dose 1mg 2mg 3mg Color Light blue White Dark blue Efficacy: The efficacy of eszopiclone in reducing sleep latency and improving sleep maintenance was established in six placebo controlled studies involving 2100 patients with chronic and transient insomnia. Chronic insomnia: Five controlled trials studied the effectiveness of eszopiclone on chronic insomnia; three studies in adult subjects, and two in elderly subjects. Adults with chronic insomnia were studied in a 6-week double-blind trial comparing eszopiclone 2mg and 3mg with placebo. Overall, both the 2mg and 3mg eszopiclone were superior to placebo. Adults with chronic insomnia were evaluated for safety and efficacy of eszopiclone 3mg compared to placebo in a 6 month double-blind trial. Eszopiclone was shown to be superior to placebo using subjective measures. Adults with chronic insomnia were studied in a 6 period cross-over polysomnograph trial comparing eszopiclone doses of 1 to 3mg. Response was shown to be dose related. Elderly subjects with chronic insomnia were evaluated in 2 double-blind trials lasting 2 weeks, comparing eszopiclone 1 and 2 mg to placebo. Both studies showed eszopiclone to be superior to placebo. Transient insomnia: Healthy adults with transient insomnia were evaluated in a double-blind single-night trial comparing eszopiclone to placebo. Eszopiclone was superior to placebo on all measures of sleep latency and maintenance. Conclusions: Eszopiclone has been shown to be effective in reducing sleep latency and improving sleep maintenance in both chronic and transient insomnia. Despite the added benefit of approval for long-term use, the cost-effectiveness of eszopiclone remains unclear without head-tohead clinical trials comparing the efficacy of eszopiclone to the other sedative-hypnotic agents available. In addition, other less costly agents, such as zolpidem, have also demonstrated efficacy and tolerability on a long-term basis in clinical trials. Recommendation: Addition to the formulary is not recommended. References: 1. Amato DA, Caron J, Krystal AD, Roach J, Roth T, Rubens R, et al. Nightly treatment of primary insomnia with eszopiclone for six months: effect on sleep, quality of life, and work limitations. Sleep 2007; 30(8):959-68. 2. Amato DA, Erman M, McCall W, Rosenberg R, Seiden D, Scharf M, et al. A 2-week efficacy and safety study of eszopiclone in elderly patients with primary insomnia. Sleep 2005; 28(6):720-7. 3. Erman M, Krystal AD, McCall W, Rosenberg R, Scharf M, Wessel T, et al. A polysomnography study of eszopiclone in elderly patients with insomnia. Current Medical Research and Opinion 2006; 22(9):1633-42. 4. Erman M, Krystal AD, Roth T, Soubrane MD, Zammit GK. Long-term efficacy and safety of zolpidem extended release 12.5 mg, administered 3 to 7 nights per week for 24 Weeks, in patients with chronic primary insomnia: a 6-month, randomized, doubleblind, placebo-controlled, parallel-group, multicenter study. Sleep 2008; 31(1):71-90. 5. Krystal AD, Roehrs T, Roth T, Walsh J, Wessel T. An evaluation of the efficacy and safety of eszopiclone over 12 months in patients with chronic primary insomnia. Sleep Medicine 2005; 6(6):487-98. 6. Krystal AD, McCall W, Perlis ML, Walsh JK. Long-term, non-nightly administration of zolpidem in the treatment of patients with primary insomnia. Journal of Clinical Psychiatry 2004; 65(8):1128-37. 7. LunestaTM (eszopiclone) [package insert]. Marlborough, MA: Sepracor Incorporated; April 2006. Prepared by: Angela Bird Pharmacy Volunteer April 2008