BILLING - Referred Laboratory Testing
advertisement

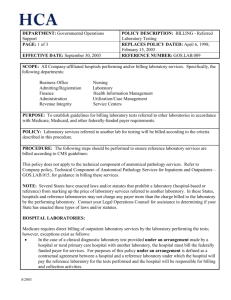
DEPARTMENT: Regulatory Compliance Support PAGE: 1 of 3 EFFECTIVE DATE: March 6, 2006 POLICY DESCRIPTION: BILLING - Referred Laboratory Testing REPLACES POLICY DATED: 4/6/98, 2/15/03, 9/30/03 (GOS.LAB.009) REFERENCE NUMBER: REGS.LAB.009 SCOPE: All Company-affiliated hospitals performing and/or billing laboratory services. Specifically, the following departments: Business Office Admitting/Registration Finance Administration Revenue Integrity Nursing Laboratory Health Information Management Utilization/Case Management Service Centers PURPOSE: To establish guidelines for billing laboratory tests referred to other laboratories in accordance with Medicare, Medicaid, and other federally-funded payer requirements. POLICY: Laboratory services referred to another lab for testing will be billed according to the criteria described in this procedure. PROCEDURE: The following steps should be performed to ensure reference laboratory services are billed according to CMS guidelines: This policy does not apply to the technical component of anatomical pathology services. Refer to Company policy, Technical Component of Anatomical Pathology Services for Inpatients and Outpatients – REGS.LAB.015, for guidance in billing these services. NOTE: Several States have enacted laws and/or statutes that prohibit a laboratory (hospital-based or reference) from marking up the price of laboratory services referred to another laboratory. In these States, hospitals and reference laboratories may not charge any payer more than the charge billed to the laboratory by the performing laboratory. Contact your Legal Operations Counsel for assistance in determining if your State has enacted these types of laws and/or statutes. HOSPITAL LABORATORIES: Medicare requires direct billing of outpatient laboratory services by the laboratory performing the tests; however, exceptions exist as follows: In the case of a clinical diagnostic laboratory test provided under an arrangement made by a hospital or rural primary care hospital with another laboratory, the hospital must bill the federally funded payer for services. For purposes of this policy under an arrangement is defined as a contractual agreement between a hospital and a reference laboratory under which the hospital will pay the reference laboratory for the tests performed and the hospital will be responsible for billing and collection activities. 2/2006 DEPARTMENT: Regulatory Compliance Support PAGE: 2 of 3 EFFECTIVE DATE: March 6, 2006 POLICY DESCRIPTION: BILLING - Referred Laboratory Testing REPLACES POLICY DATED: 4/6/98, 2/15/03, 9/30/03 (GOS.LAB.009) REFERENCE NUMBER: REGS.LAB.009 Hospitals that do not have an arrangement with a reference laboratory may bill the federally funded payer for the tests if the following criteria are met: Referring laboratory is located in or is part of a rural hospital, or Ownership rules apply (Referring laboratory is wholly-owned by the reference laboratory, referring laboratory wholly owns the reference laboratory, or both the referring laboratory and the reference laboratory are wholly-owned by a third entity), or No more than 30% of the total laboratory tests for which the referring laboratory performs annually are performed by a reference laboratory, other than an ownership-related laboratory. REFERENCE LABORATORIES: Medicare requires direct billing of outpatient laboratory services by the laboratory performing the tests; however, reference laboratories which send specimens to other laboratories for testing may bill for the tests if the reference laboratory meets any of the 3 following criteria: Referring laboratory is located in or is part of a rural hospital, or Ownership rules apply (Referring laboratory is wholly-owned by the reference laboratory, referring laboratory wholly-owns the reference laboratory, or both the referring laboratory and the reference laboratory are wholly-owned by a third entity), or No more than 30% of the total laboratory tests for which the referring laboratory performs annually are performed by a reference laboratory, other than an ownership-related laboratory. Additionally, all reference laboratories utilized by the facility must be certified in the testing specialty in order for Medicare to reimburse for the laboratory services. IMPLEMENTATION AND ANNUAL REVIEW 1. Laboratory personnel must identify all tests in the chargemaster that are referred to another laboratory for testing. 2. Laboratory personnel must identify the reference laboratory(s) that is utilized for each test. 3. Laboratory personnel must obtain and/or verify that documented CLIA (Clinical Laboratory Improvement Act) and/or CAP (College of American Pathologists) certificate information is available for each testing specialty used by each reference laboratory identified in previous step. 4. Laboratory and Business Office/Service Center personnel must determine if the reference laboratory is under arrangement to provide services for the facility laboratory. If the reference laboratory is under arrangement, the facility must bill for all laboratory services. Proceed to step 7 of the implementation process. 5. If the laboratory is not under arrangement, not part of a rural hospital, and not wholly-owned by a 2/2006 DEPARTMENT: Regulatory Compliance Support PAGE: 3 of 3 EFFECTIVE DATE: March 6, 2006 POLICY DESCRIPTION: BILLING - Referred Laboratory Testing REPLACES POLICY DATED: 4/6/98, 2/15/03, 9/30/03 (GOS.LAB.009) REFERENCE NUMBER: REGS.LAB.009 hospital under arrangement, then the laboratory must meet the 70/30 rule in order to bill Medicare for tests that are referred. In this case, laboratory personnel must: a. Review annual volumes of all referred tests and total tests performed. Determine the percentage of tests referred by dividing the number of referred tests by the total tests performed. Example: Total annual tests performed = 100,000 tests Total annual referred tests performed = 5,000 tests Percent Referred tests = 5,000/100,000 x 100 = 5% b. Determine whether laboratory meets the 30% exception rule (no more than 30% of testing may be referred in order for a laboratory to direct bill referred tests). In the example above, the laboratory may continue to direct bill referred tests. 6. If the laboratory refers more than 30% of its annual volume, the laboratory may no longer directly bill Medicare for those tests which are referred. In this case, the referring laboratory must provide billing information to the reference laboratory with instructions that the reference laboratory direct bill. 7. If the hospital will be billing for referred laboratory services, the following steps must be performed: a. Laboratory and Business Office/Service Center personnel must consult with Legal Operations Counsel to determine if State laws and/or statutes prohibit the marking up of laboratory services. b. If it is determined that such laws and/or statutes exist, the hospital must not charge any payer more than the charge billed by performing laboratory. 8. Laboratory and Business Office/Service Center personnel must educate all staff associates responsible for ordering, charging, or billing laboratory services on the contents of this policy. 9. The Facility Ethics and Compliance Committee (FECC) or a sub committee of the FECC must review the laboratory’s arrangements on an annual basis and deviations from this Policy should be documented and resolved in accordance with the Billing Monitoring Policy, REGS.GEN.001. 10. Facilities must adhere to specific intermediary and/or state requirements. Business Office/Service Center personnel must identify intermediary interpretations which vary from the interpretations in this policy. Specific intermediary documentation related to the variance(s) must be obtained and provided to Regulatory Compliance Support. Documentation may be sent via email to the Regs Helpline. The Facility Ethics and Compliance Committee is responsible for implementation of this policy within the facility. REFERENCES: OIG Model Compliance Plan for Clinical Labs (March, 1997) Medicare Claims Processing Manual (100-04), Chapter 16, Section 40.1 Med-Manual, Med-Guide 10,285.03, Independent Laboratory Services Med-Law, Med-Guide, SS Act Section 1861, Definitions of Services, Institutions, ETC. 42 U.S.C. Med-Law, Med-Guide, SS Act Section 1833, Payment of Benefits, Subse (h), Clinical Diagnostic Laboratory Tests 2/2006