interstitial cystitis in india
advertisement

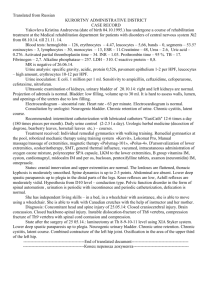
INTERSTITIAL CYSTITIS IN INDIAA SIMPLE PRACTICAL APPORACH NAGENDRA MISHRA, MD CONSULTANT UROLOGIST Jivraj Mehta Hospital, Ahmedabad, India nagendraad1@yahoo.com Interstitial cystitis (IC) is a chronic, inflammatory disorder of the urinary bladder characterized by variable degrees of bladder pain, urinary frequency and urgency. It is more common in women. IC is a clinical entity not well defined poorly understood, inadequately treated and extraordinary bothersome. The aware ness about IC is increasing in INDIA. When I was trained in urology some 18 years back it was believed that IC is a disease of western world and does not exist in INDIA. The symptoms of IC are very much similar to tuberculosis and all the patients of IC were being treated as tuberculosis of genitourinary symptoms. My tryst with IC started when some of the patients diagnosed as tuberculosis and adequately treated did not respond . I did augmentation cystoplasy in one of these patients for thimble bladder and realized that the patient did not have thick fibrous thimble bladder but some other pathology. This is how I made my first diagnosis of interstitial cystitis I have around 150 patients of IC . In INDIA male to female patient ratio is 1:2. I did an international survey on IC in 2002 with Jane Meijlink from Netherlands. Questionnaire containing 24 questions was sent to urologist all over the world by email. We had 151 responses from 32 countries which proved that IC is a global disease. The surprising fact was that none of two researchers thought alike on any aspect of IC. This survey emphasized beyond doubt that there is need to frame new guidelins and criteria for interstitial cystitis .It is very sad as no international consensus has been reached till now even five years after that. In 1987, the NIDDK formed a consensus definition of IC. The criteria were revised in 1988..Today, some 20 years after these research guidelines were first drawn up, the original aim has not been fulfilled. The guideline has not served its purpose since it was basically a concept of exclusions and not based on evidence. Very few patients with interstitial cystitis fulfilled the criteria and for every patient diagnosed with IC, many remained undiagnosed. It has been estimated that if the guidelines are strictly followed, around 60% of patients will fail to be diagnosed. BLADDER PAIN AND PELVIC PAIN In 2002 first time ICS described interstitial cystitis as painful bladder syndrome. Bladder pain is defined as suprapubic or retropubic pain which usually increases with bladder filling and may persist after voiding. Pelvic pain localizes to the anatomic pelvis abdominal wall at or below the umbilicus , lumbrosacral back or the buttocks DEFINITION OF IC Syndrome of pelvic pain with urinary, frequency and urgency in the absence of definable pathology. PROPOSED PATHOPHYSIOLOGY OF IC It is believed that the primary defect lies in the urothelium which allows absorption of substances such as potassium and urea into the bladder wall. This eventually leads to tissue damage and pain as well as symptoms of frequency and urgency. Activation of mast cells with histamine release and neurogenic inflammation are also considered important factors in the etiopathology of IC. These changes cause upregulation of the sensory nerves of the bladder resulting in a state of “neurologic wind -up” which presents as hyperalgesia. SYMPTOMS The symptoms of IC patients are by no means uniform. These symptoms are related to urological, gynecological, gastrointestinal and pelvic floor organs. They may originate from the bladder, urethra, prostate, vagina, uterus, rectum and pelvic floor muscles. The hallmark of IC is a triad of pain, frequency and urgency. Pain is the most important symptom. Pain is felt in suprapubic, retropubic, infrapubic, urethral, genital and /or rectal regions. Pain may be continuous or related to the micturition cycle. Sometimes patients cannot define the exact location of pain and feel it is situated deep in the pelvis. Some patients mention burning, pressure sensation of urinary discomfort instead of pain. Males may complain of painful ejaculation while women present with dyspareunia. Frequency more than eight times is considered abnormal. While most of the patients with IC have frequency and urgency, it is not a must. Patients with normal frequency and without urgency can also have IC. Nocturia may or may not be present. In other words, patients can have a variety of different symptom combinations. Initially a patient may present with only one symptom and develop the fully-fledged syndrome over a span of 5 years. IC is a chronic disease, so the above-mentioned symptoms must be present for more than 3 months to diagnose IC. UNUSUAL SYMPTOMSA typical patient of IC may present with triad of pain frequency and urgency but few patients may present with unusual symptoms like incomplete evacuation, dribbling, desire to pass urine immediately after micturition, difficulty in sitting and walling with urinary symptoms, anal discomfort. These symptoms are not mentioned in the standard textbooks but patients commonly complain like that. I feel that these symptoms must be included in the textbooks. These symptoms are not due to obstruction but they are felt by the patients as they pass little amout of urine every void and have problems of increased sensation. IC should also be considered in those patients of urinary tract infection who do not improve after adequate therapy, patients of urge incontinence with pain and patients of chronic abacterial prostatitis who do not improve . I believe that IC and chronic abacterial prostatitis are the same diseases. PHYSICAL EXAMINATIONOn examination, the patient is essentially normal except for suprapubic tenderness or anterior vaginal wall tenderness in females and prostatic tenderness in males. INVESTIGATIONS Urine routine and culture Urine cytology USG of KUB Voiding log Urodynamics Cystoscopy Potassium sensitivity test Symptom scales Urine analysis, urine culture, and sonography of kidney, ureter and bladder are important for the exclusion of other diseases with similar symptoms and are considered very important investigations. On ultrasonography, presence of a small capacity bladder (normal bladder wall thickness) with normal upper tracts should raise the suspicion of IC. I do urine routine , urine culture and sonography in all the patients and if they all are normal I subject the patietnt to cystoscopy and hydrodistension. Voiding diary, urodynamics, potassium test and symptom scales are not routinely done in all the patients. voiding diary can be helpful as it shows that patients void small quantities every time. Some of severe cases of IC may void 50 times in the day. Urodynamics and potassium tests are not very important and are considered optional tests. It is believed that urodynamics does not give any additional information and should be reserved for those patients where OAB is also suspected. Intravesical PST ( Potassium Sensitivity test) detects the permeability of bladder epithelium. This test has been shown to be positive in 75% of patients with IC and is also positive in patients with detrusor instability, radiation cystitis and bacterial cystitis. This test is not diagnostic of IC. It has its own drawbacks and is painful. PST is therefore not recommended. Cystoscopy with or without hydrodistension is a very controversial investigation. While Europeans feel that cystoscopy with bladder biopsy is essential to diagnose IC, others feel that there is no need to perform cystoscopy. In the presence of hematuria, cystoscopy becomes mandatory to rule out malignancy in patients over the age of 40 years. Glomerulations and Hunner’s ulcer have been reported to be present in all patients with IC, but this is not the case. Moreover, these findings are very subjective and differ from observer to observer. In an attempt to standardize cystoscopic findings, ESSIC ( European Society for the Study of Interstitial Cystitis) described various grades of bladder mucosa appearance on cystoscopy. Copenhagen Cystoscopic classification of bladder mucosa (May 2003) Grade 0= normal mucosa Grade I = petechiae in at least two quadrants Grade II = large submucosal bleeding (ecchymosis) Grade III = diffuse global mucosal bleeding Grade IV = mucosal disruption, with or without bleeding/oedema CYSTOSCOPIC APPEARANCE OF BLADDER MUCOSA SHOWING PATECHIAE AND ECCHYMOSIS Cystoscopy is done under anaesthesia using either saline or glycine as irrigation solution, the height of the reservoir is kept at 80 cm and the bladder is filled under gravity. Then the bladder is evacuated and refilled again. The colour of the evacuated fluid is noted. It is necessary to distend the bladder again as the petechiae and ecchymosis develop on evacuation of the bladder and can be seen when we distend the bladder again. In few cases patechiae and ecchymosis develop on distension. Some patients bleed from all over the mucosa .If hydrodistension is to be done, the bladder is kept distended for 3 minutes and then evacuated again. After this, bladder biopsies can be taken. Now I do not do routine biopsy as I have not found it useful after 15 years of biopsy taking. My indication for taking the biopsy is presence of a lesion before I distend the bladder(predistension lesion) .The bladder capacity under anaesthesia is also noted. The colour of the terminal draining fluid is red in the cases where pethechiae and ecchymosis develop. It is important to note that bladders with normal mucosal findings (grade 0) can also have IC. The bladder of an IC patient can have any capacity and there is no limit beyond which IC can be ruled out depending on bladder capacity. Do not hydrodilate the bladder by increasing the reservoir height. I do not keep foleys catheter after hydrodistension as patients find it very uncomfortable when they wake up from anaesthesia. As a precautionary measure I do not distend the bladder more that 750 ml of saline as I fear that bladder may rupture. After cystoscopy when patients wake up they have a desire to pass urine though their bladder is empty. SCREENING AND DIAGNOSTIC TOOLS: Clinical scales such as the O’Leary-Sant questionnaire, the University of Wisconsin interstitial cystitis scale and the Pelvic pain and Urgency/Frequency (PUF) scale are available for clinical use but cannot diagnose IC. It is believed that they need further evaluation.These scales are not used in INDIA. URINARY MARKERS: They can be of help in future to diagnose IC. Antiproliferative factor (APF) is currently the most extensively studied marker and most promising, but still not available for clinical use. Other markers being studied are HP-EGF. EGF, Insulin-like growth factor 1 etc. but need further evaluation. TREATMENT: I use a protocol of staged treatment. All the patients are subjected to cystoscopy and therapeutic hydrodistension after their urine culture, urine routine and sonography are normal. Around 40% patients inprove with hydrodistension and do not need further therapy. Hydrodistension is a very controversial modality of treatment but gives immediate relief in most of the patients. A few patients also enjoy long-lasting benefit. If a patient remains symptom-free after hydrodistension for more than a year, it can be repeated when the symptoms develop again. On cystoscopy under anasthesia if patient has less than 150 ml capacity he is advised for surgical therapy . If patients do not improve after hydrodistension then they are put on triple drug therapy including amytrptaline, hydroxyzine and gabapantin for 3 months. PPS is not available in India. It is important to note that the routine analgesics do not act on such patients and should not be prescribed alone. Antibiotics also do not work so they should also be avoided. If the patient does not respond or there is flare-up during oral therapy, the patient is treated with intravesical rescue solutions. The rescue solutions are prepared by mixing an anaesthetic agent with steroid and heparin and sodium bicarbonate is added to facilitate absorption. The solution is usually kept in the bladder for 15-20 minutes and 6-8 treatments are given at intervals of 2 weeks. My favourite rescue solution consists of 40 ml sensorcaine 0.5%, 20 ml sodabicarb , 2cc dexamethasone and 10000 unit of heparin. Some patients do not respond and continue to suffer. These patients are offered intravesical Botulinum toxin injections or neuromodulation. 200 to 300 units of botulinum toxin is injected in the bladder cystoscopically at 20 to 30 sites (10 units per injection site) using a specially designed needle. Botulinum toxin improves the symptoms in around half of the patients with intractable IC, but the effect is temporary and lasts for 6 to 12 months, making re-injection necessary. Neuromodulation is found effective in around one third of patients with intractable IC when sacral stimulation is used. First a test stimulation is carried out for a period of 7 days. If the patient improves, a permanent generator is implanted to stimulate the S3 nerve root. Although both these modalities are effective in some patients, they should only be attempted if patients do not improve with routine treatment. Surgery is offered as a last resort and various procedures are available with varying success rates. It includes augmentation cystoplasty, substitution cystoplasty, neobladder with or without cystectomy. Bladder lesions are ablated with Laser. Surgery is offered to those patients who have a miserable life and have failed all other therapies. DIET AND SELF HELPI do not give any specific diet advise. Patients are advised not to take those food items which cause a flare. Patients are advised to drink less water as it decrease frequency but a group of patients can not tolerate concentrated urine and need large amount of fluids. Alternate modalities of treatment like physical therapy, yoga, pelvic floor relaxation are not popular in India. NO PROGRESS IN TREATMENTThough lot of basic research has been done no drug is yet developed which cures IC .Treatment of IC is a challenge and development of oral effective cure should be goal of international researchers interested in IC. Patients are interested in cure. CHANGE OF NOMENCLATURE: In 2002 the ICS for the first time described IC as PBS (Painful bladder syndrome). In 2006 ESSIC adopted the name Bladder Pain Syndrome. The disease is still popularly known as IC. There are many differences of opinion amongst scientists, urologists and patient support groups about changing the name of the disease and nothing has been decided yet. IC IN CHILDREN Patients under the age of 18 years were automatic exclusions in the 1987 NIDDK research criteria. The diagnosis of IC in children is controversial. Children do indeed present with dysfunctional voiding. There is no theoretical reason why IC cannot exist in children. It should always be considered in differential diagnosis in children who present with pelvic pain, frequency and urgency. INDIAN SURVEY ON INTERSTITIAL CYSTITISA survey was done at two urological meetings in INDIA. 400 questionnaires were distributed amongst the urologists who attended the meeting. 131 filled up the questionnaire and returned back. The analysis was very encouraging,109 believed that IC exists in INDIA. 104 see patients with IC. 122 agreed that they do see patients with frequency, urgency, pain syndrome where no disease can be identified. Around 85percent of responders did urine culture and sensitivity, ultrasonography, and cystoscopy. 50% believed in performing bladder biopsy. The potassium test is done by only 8%. Very few urologist did cystoscopy under local anaesthesia. In treatment, hydrodistension is done by 70 % and oral therapy also prescribed by 70%. Intravesical therapy is uncommon (30%) and botox and neuromodulation rarely done. Out of these 131 urologists, 34 preferred IC as the name, 60 PBS and 37 PBS/IC. 104 urologists want Elmiron to be made available in India, 13 do not want it and 14 had no idea what Elmiron is. 75 of the responders were from major medical institutes in India while 54 had their own solo practice.( see annexure 1 and annexure 2) AWARENESS OF IC The situation amongst urologist is better but not amonst other physicians. We are trying to increase awareness during conferences by distributing leaflets. International painful bladder foundation is active in INDIA and I am founder executive member of the organization based in AMSTERDAM.(www.painful-bladder.org) ESSIC CHAIRMAN JORGEN NORDLING SPEAKING IN UROLOGICAL SOCIETY OF INDIA MEETING. INTERSTITIAL CYSTITIS PATIENT MEETING IN PROGRESS IMPORTANT GUIDELINES Suspect IC if patient prefers to move by train over road transport as toilet facility is available in train . Patient goes to toilet during consultation with physician,. IC can be present even if cystoscopic findings are normal. IC can be present in normal capacity bladder. Do not say to the patient that he/she does not have any disease as all the reports are normal . Do not send the patient to psychiatrist. Do not do any thing which causes pain to the patient. Do not do hysterectomy for urinary symptoms. Do not follow NIH 1987-88 guidelines. Do not do cystoscopy without anesthesia. Do not hydrodilate bladder at the time of cystoscopy.by increasing the height of the reservoir. CONCLUSION In 2007 there is consensus that a big change is needed in the IC world. There is a need to draw up a definition and establish criteria for the disease. It is also believed that the new definition and criteria should be evidence-based and should not be only opinion-based. All the researchers agree that it is very difficult task but that a start has to be made. Until the final diagnostic criteria are established, there is a need to work together. There is a need to follow a common algorithm so that a large amount of data can be collected and compared. There should be a working algorithm for history-taking, physical examination, investigations, cystoscopy, biopsy and treatment. Furthermore, basic research has to be done to find cure for this debilitating condition. Annexure 1 INDIAN SURVEY ON INTERSTITIAL CYSTITIS DATE- 8 FEB 2007 PLACE- PATNA, INDIA, USICON- 2007. DATE- 1ST MAR 2007, PLACE- GOA , INDIA, UROLOGICA 2007 QUSTIONNAIRE DISTRIBUTED- 400. RESPONSE RECEIVED- 131 TH QUESTIONNAIRE Do you think IC exists in INDIA. YES/NO Do you see patients of IC YES/NO Do you see patients of pain, frequency and urgency YES/NO Where no diagnosis can be made and patient do not Improve in spite of treatment How do you treat such patients antibiotics Analgesics Alpha blockers As IC what investigations will you do in such a case X-RAY KUB USG kub Urine C/S VOIDING DIARY Cytology Cystoscopy KCL TEST URODYNAMICS BLADDER BIOPSY In a suspected case of IC you will do cystoscopy under local anesthesia General anaesthesia Spinal anaesthesia If you diagnose a patient of IC how do you treat hydrodistension Oral therapy Intravesical drugs Intravesical BOTOX INTERSTIM What term will you prefer for such syndrome IC PBS PBS/IC What best describes you solo practicing Institute based Do you think elmiron should be made available in India YES/NO ANNEXURE 2 SURVEY RESULTS 1. do you believe IC exists in India 2. do you see patients of IC 3 do you see patients of pain frequency and urgency yes 109 no 22 yes 104 no 25 yes 122 no 06 where no cause is diagnosed 4. how you treat such patients- antibiotics 45 analgesics 58 alfa blockers 58 as IC 55 5.what investigations will you do in IC patient XRAY KUB 54 USG KUB 110 Urine C/S 115 Voiding diary 98 Cytology 85 Cystoscopy 116 Kcl test 09 Urodynamics 72 Bladder biopsy 71 6. under which anaesthesia you will do cystoscopy Local 22 General 94 Spinal 17 7.what treatments do you offer to such patients hydrodistension 89 oral therapy 88 intravesical 42 botox 17 interstim 02 8. what terminology will you prefer IC 34 PBS 60 PBS/IC 37 9. what describes your practice solo 54 institute based 75 10. do you think elmiron should be made available yes 104 no 13 in India. 14 did not know what elmiron is