SUPPORTING MATERIAL:
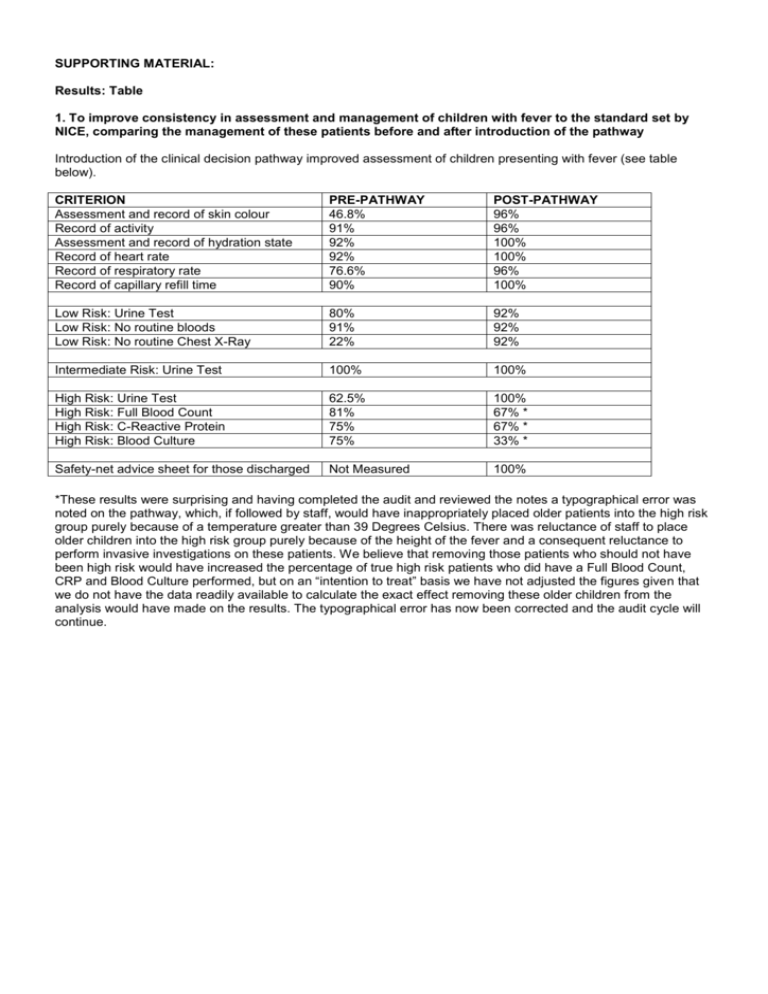
Results: Table
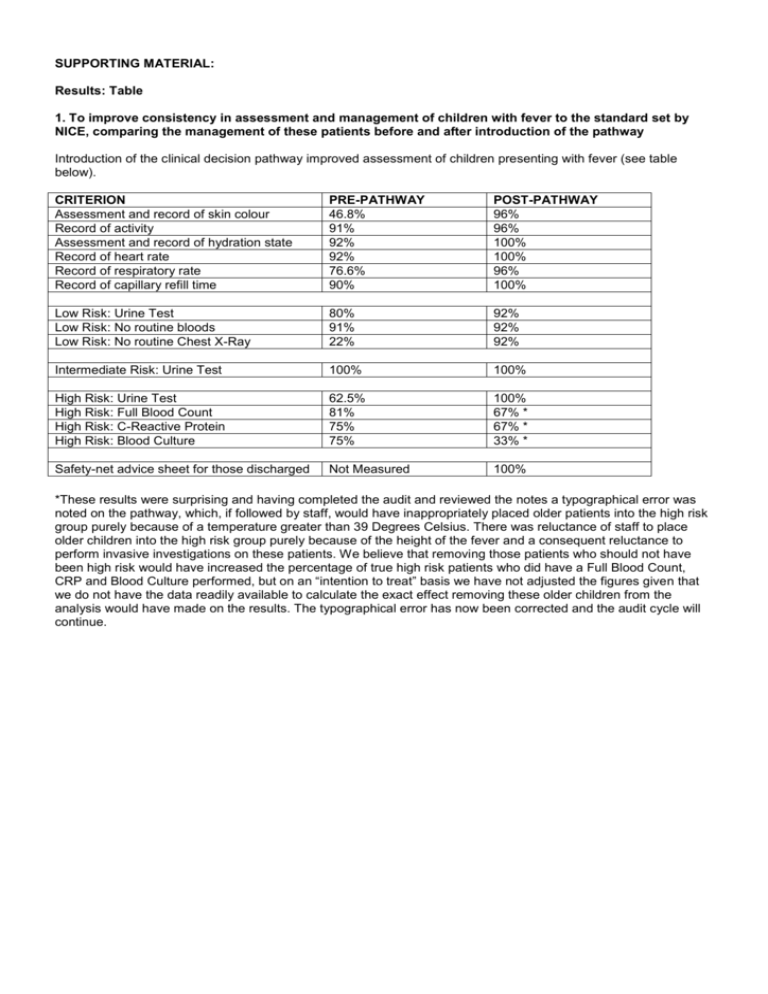
1. To improve consistency in assessment and management of children with fever to the standard set by
NICE, comparing the management of these patients before and after introduction of the pathway
Introduction of the clinical decision pathway improved assessment of children presenting with fever (see table
below).
CRITERION
Assessment and record of skin colour
Record of activity
Assessment and record of hydration state
Record of heart rate
Record of respiratory rate
Record of capillary refill time
PRE-PATHWAY
46.8%
91%
92%
92%
76.6%
90%
POST-PATHWAY
96%
96%
100%
100%
96%
100%
Low Risk: Urine Test
Low Risk: No routine bloods
Low Risk: No routine Chest X-Ray
80%
91%
22%
92%
92%
92%
Intermediate Risk: Urine Test
100%
100%
High Risk: Urine Test
High Risk: Full Blood Count
High Risk: C-Reactive Protein
High Risk: Blood Culture
62.5%
81%
75%
75%
100%
67% *
67% *
33% *
Safety-net advice sheet for those discharged
Not Measured
100%
*These results were surprising and having completed the audit and reviewed the notes a typographical error was
noted on the pathway, which, if followed by staff, would have inappropriately placed older patients into the high risk
group purely because of a temperature greater than 39 Degrees Celsius. There was reluctance of staff to place
older children into the high risk group purely because of the height of the fever and a consequent reluctance to
perform invasive investigations on these patients. We believe that removing those patients who should not have
been high risk would have increased the percentage of true high risk patients who did have a Full Blood Count,
CRP and Blood Culture performed, but on an “intention to treat” basis we have not adjusted the figures given that
we do not have the data readily available to calculate the exact effect removing these older children from the
analysis would have made on the results. The typographical error has now been corrected and the audit cycle will
continue.
OTHER SUPPORTING INFORMATION:
1. Implementation of a clinical decision-making pathway improved the assessment of children with fever and
helped clinicians identify those patients who were at risk of serious illness. We anticipate this will have had a
significant impact for patients given the diverse aetiology of fever in children
2. Whilst the pathway was very good at improving recognition of ill children, it is difficult for a pathway to ensure
that the next steps (investigations and management) are consistently applied given that subjective clinician
preferences can have an impact on the care of children
3. Review of the NICE guideline revealed some inconsistencies and discrepancies that we had to address and
agree an interpretation of. Clinicians have difficulty differentiating between “pale” and “pallor”. Such
differentiation is important within the guidance as it is one of the determinants of whether a patient is low or
intermediate risk. In future more objective terms should be used
3. There was difficulty in using the NICE guideline criteria of a Capillary Refill Time of >3 seconds to place a
patient into the Intermediate Risk group. This was not consistent with other guidance familiar to clinical staff
which referred to a capillary refill time of less than 2 seconds as normal. The department therefore decided
to use the familiar standard of 2 seconds for this section of the guidance
4. There were difficulties communicating introduction of the pathway to all clinical staff, including those who
visited the Emergency Department but who did not routinely work here. This was overcome by presenting
the pathway in a number of fora, and using coloured posters around the department to refresh staff
memories. The presence of clinically-based senior staff within our Emergency Department for 16 hours out
of every 24 helped facilitate implementation of this guidance
5. The Trust employs a dedicated clinical pathways coordinator and this key member of staff makes
implementing national guidance significantly easier, and enables standardisation to take place throughout
the Trust
6. Having a system to be able to collect the notes of patients where the pathway was used facilitated easier
audit of implementation of the guidance. We are grateful to the medical students from the University of
Liverpool who assisted us with this (John Canny, Helen Moore, Claire Sweeney).
Important Information
Disclaimer
The Fever without a Focus Care Pathway has been produced by Dr Andrew Rowland at Alder Hey Children’s NHS
Foundation Trust for use internally at Alder Hey Children’s NHS Foundation Trust as a fever without a focus
screening tool for children aged <5 years.
The information contained in the Fever without a Focus Care Pathway is provided for use by appropriately qualified
professionals and the making of any decision regarding the suitability of appropriate health care support and of a
particular treatment or therapy for a patient, is subject to the reader’s professional judgement. Whilst every
reasonable care has been taken to ensure the accuracy of its contents, neither the author nor the publisher can
accept any responsibility for any action taken, or not taken, on the basis of this information.
The Fever without a Focus Care Pathway is not a substitute for the exercise of appropriate professional
skill and judgement.
Alder Hey Children’s NHS Foundation Trust shall not be liable to any person for any loss or damage which may
arise from the use of any of the information contained in this publication.
The above disclaimer is not intended to restrict or exclude liability for death or personal injury caused by the
negligence of Alder Hey Children’s NHS Foundation Trust.
Copyright
© 2008 Alder Hey Children’s NHS Foundation Trust. All rights reserved. Not to be reproduced in whole or in part
without the permission of the copyright holder.
The document may only be reproduced for non-commercial clinical internal use provided that the existing copyright
statement is retained.
This document must not be used, distributed or the content changed in any way other than with the express written
consent of the Alder Hey Children’s NHS Foundation Trust and on such terms as the Alder Hey Children’s NHS
Foundation Trust may specify.
The document must not be sold, licensed, transferred, copied or reproduced in whole or in part in any manner or in
or on any media to any person without the prior written consent of the Alder Hey Children’s NHS Foundation Trust.
In case of any kind of publication or presentation mentioning use of the document it shall be acknowledged that the
document originated from Alder Hey Children’s NHS Foundation Trust.
Any intention to publish or present material mentioning the document must be authorised in writing prior to
publication by Alder Hey Children’s NHS Foundation Trust.
Enquiries regarding copyright should be addressed to Elvina.White@Alderhey.nhs.uk
FEVER WITHOUT A FOCUS
Screening tool for children aged <5 years
OTHERS
RESPIRATORY
HYDRATION
ACTI VITY
COLOUR
Patient Name:
This document is a screening tool for the risk of serious illness
after a diagnosis of ‘fever without a focus’ has been made by
AE Number:
full history and clinical examination in a child aged under 5 years.
All patients with ‘fever without a focus’ should be assessed for shock and dehydration and treated according to
Emergency Department guidelines. Also consider using other departmental pathways, as appropriate eg: Limping Child
Tick all boxes which apply, and follow the HIGH, MEDIUM or LOW risk management pathways overleaf as indicated.
A patient with any one or more high risk sign(s) or symptom(s) should be managed as high risk. Only manage as
low risk if all ticks are in low risk boxes.
Pale OR Mottled OR Ashen OR Blue
HIGH RISK
Pallor OR Pallor reported by parent or carer
M EDIUM
None of the above AND Normal colour of skin, lips and tongue
LOW RISK
No response to social cues OR
Looks unwell OR
Unable to rouse or does not stay awake OR
Cry is weak OR High pitched OR Continuous
HIGH RISK
Does not respond normally to social cues OR
Wakes only with prolonged stimulation OR
Decreased activity OR
No smile
M EDIUM
Has a normal response to social cues AND
Content or smiles AND
Stays awake or awakens quickly AND
Strong normal cry or No cry
LOW RISK
Reduced skin turgor OR Weak pulse
Assess % dehydration & treat
HIGH RISK
Dry mucus membranes OR
Poor feeding in infants OR
Capillary Refill Time ≥ 2 seconds OR
Decreased urine output
Assess % dehydration & treat
M EDIUM
Normal skin and eyes AND
Moist mucus membranes AND
Capillary Refill Time <2 seconds
LOW RISK
Grunting OR
Respiratory Rate > 60 breaths/min OR
Moderate or severe chest wall recession OR
Exhausted OR
Abnormal respiratory pattern
HIGH RISK
Nasal Flaring OR
Respiratory Rate >50 breaths/min (age <12 months) or >40 (age >12 months) OR
Oxygen Saturations ≤ 95% in air OR
Crackles heard on chest auscultation
M EDIUM
None of the above respiratory signs AND Normal respiratory examination
LOW RISK
Temperature ≥ 38oC aged < 3 months OR ≥ 39oC aged 3 to 6 months
HIGH RISK
Non-blanching rash OR
Bulging Fontanelle OR Neck Stiffness OR
Status Epilepticus OR Focal Seizures OR Focal Neurological Signs OR
Bile-stained vomiting
HIGH RISK
Fever for > 5 days OR
Swollen joint OR Swollen limb OR
Child is non-weight bearing OR Child is not using an extremity OR
New neck lump > 2 cm
M EDIUM
No HIGH OR MEDIUM symptoms or signs from any of the above sections
LOW RISK
FEVER WITHOUT FOCUS: Management of a child aged <5 yrs at HIGH RISK of serious illness
Refer to medical on-call team for admission and proceed with investigations.
If symptoms or signs of shock and/or dehydration are present, treat according to departmental guidelines.
Also see departmental guidelines for lumbar puncture and NICE guidelines for UTI investigation.
INVESTIGATIONS TO BE COMPLETED IN THE EMERGENCY DEPARTMENT
Child aged
< 3 months
Time
sent
Time
checked
Comment
Child aged
3 months to 5yrs
FBC
FBC
CRP
CRP
Chest X-Ray
Chest X-Ray
Blood culture
Blood Culture
Lumbar puncture
Urine test for UTI
Urine test for UTI
Time
sent
Time
checked
Comment
Consider the following for a child aged 3 months - 5yrs
Faeces culture
(if diarrhoea present)
Discuss with senior Emergency Department doctor or Medical Registrar
(ST3/4) and document reason for decision in clinical notes below
ALL HIGH RISK PATIENTS SHOULD HAVE:
Lumbar puncture
½ hourly observations and intravenous antibiotics
Blood gas
Referral to Medical on call team
Serum electrolytes
Review within 1 hour
at ____ : ____
by Medical Registrar (ST3/4) or above at ____ : ____
Faeces culture
(if diarrhoea present)
Please document reasoning for clinical decisions, including any deviation from the guidelines
CLINICAL NOTES (time all entries)
Attach urine test printout here
Identification of clinician
Surname:
Grade:
Signature:
Specialty:
Intravenous antibiotics given
Date: ___ / ___ / _____
FEVER WITHOUT FOCUS: Management of a child aged <5 yrs at MEDIUM RISK of serious illness
Upon completion of your history and examination discuss the need for further investigations with a senior
Emergency Department doctor (if available) or the 1st on-call Medical Registrar (ST3/4). Document discussion
and reasons for decision in clinical notes section below. As a minimum all patients should have an appropriate
urine test for UTI, as per the NICE UTI Guidelines.
If symptoms or signs of shock and/or dehydration are present, treat according to departmental guidelines.
Also see departmental guidelines for lumbar puncture and NICE guidelines for UTI investigation.
INVESTIGATIONS
(if appropriate)
Urine test for UTI
Needed
YES / NO
YES
Time
sent
Time
checked
Comment
FBC
CRP
Blood culture
Lumbar puncture
Chest X-Ray
ALL MEDIUM RISK PATIENTS SHOULD HAVE:
Hourly observations
Review of clinical condition & results with a senior doctor (within 2 hours of starting this pathway)
DISPOSAL Discharge with Fever Management Advice leaflet
(Record reasons for decision in clinical notes)
at ____ : _____
Admit
(Record reasons for decision in clinical notes)
Please document reasoning for clinical decisions, including any deviation from the guidelines
CLINICAL NOTES (time all entries)
Attach urine test printout here
Identification of clinician
Surname:
Grade:
Signature:
Specialty:
Date: ___ / ___ / _____
FEVER WITHOUT FOCUS: Management of a child aged <5 yrs at LOW RISK of serious illness
Upon completion of your history and examination all children should have an appropriate urine test
for UTI, as per the NICE UTI guidelines
INVESTIGATION
Needed
Urine test for UTI
YES
Time
sent
Time
checked
Comment
ALL LOW RISK PATIENTS SHOULD HAVE:
Re-examination for signs or symptoms of pneumonia and record details in the clinical notes below
(remember that signs may be subtle)
Respiratory rate and respiratory effort re-recorded on the Emergency Department observation sheet
DISCHARGE CRITERIA
UTI & pneumonia excluded
Fever Management Advice leaflet given
Please document reasoning for clinical decisions, including any deviation from the guidelines
CLINICAL NOTES (time all entries)
Attach urine test printout here
Identification of clinician
Surname:
Grade:
Signature:
Speciality:
Date: ___ / ___ / _____
DOES YOUR PATIENT HAVE A
FEVER BUT NO FOCUS?
USE THE FEVER PATHWAY: INVESTIGATE AND MANAGE
PATIENTS APPROPRIATELY!
AGE
HIGH RISK
(Give all patients iv
antibiotics)
<3
months
MEDIUM
RISK
FBC
Urine Test for
CRP
UTI*
Blood Culture
…and DISCUSS the
Chest X-Ray
need for other
* investigations with a
Urine Test for UTI
doctor and
Lumbar Puncture senior
document this
LOW RISK
Urine Test
for UTI*
discussion clearly on
the pathway
>3
months
FBC
Urine Test for
CRP
UTI*
Blood Culture
…and DISCUSS the
Chest X-Ray
need for other
* investigations with a
Urine Test for UTI
Consider Lumbar Puncture,
Blood Gas, Serum
Electrolytes, Faeces Culture
senior doctor and
document this
discussion clearly on
the pathway
(DISCUSS with a senior
doctor and document this
discussion clearly on the
pathway)
*See NICE guidelines for the investigation of possible UTI
Urine Test
for UTI*
Alder Hey Children’s NHS Foundation Trust
Shared Learning Award submission – Feverish Illness in Children
Emergency Department Discharge Advice Sheet
We think that your child is well enough to go home now, but please telephone the
number below if:
your child’s health gets worse
you are worried about your child
you have concerns about looking after your child at home
your child has a fit
your child develops a rash that does not disappear with pressure (see
the ‘tumbler test’ at the end of this sheet)
your child has a fever lasting longer than 5 days.
Phone this number for further advice: 0845 46 47 (NHS Direct)
or take your child to your GP or the nearest Accident and Emergency Department
as soon as possible.
What to do when your child has a fever
Preventing dehydration
Offer your child regular drinks (where a baby or child is breastfed the most appropriate fluid
is breastmilk).
Look for signs of dehydration:
sunken fontanelle (soft spot on a baby’s head)
dry mouth
sunken eyes
no tears
If you find signs of dehydration encourage your child to drink more fluids and seek further
advice if you are worried.
Clothing
Alder Hey Children’s NHS Foundation Trust
Shared Learning Award submission – Feverish Illness in Children
Children with fever should not be under or over dressed. If your child is shivering or
sweating a lot, change the amount of clothes they are wearing.
Medicines to reduce temperature
It is not necessary to use medicines (paracetamol or ibuprofen) to treat your child’s
temperature. But if your child has a fever and is distressed or very unwell, you can help
to make them feel more comfortable by giving them either paracetamol or ibuprofen
(please read the instructions on the bottle first and do not exceed the maximum daily
doses). Don’t give these medicines at the same time. If your child has not improved 2-3
hours later, you may want to try giving the other medicine.
Please ask your local community pharmacist for more advice about medicines.
Never give aspirin to a child.
Sponging
Do not sponge your child with water. This does not help to reduce fever.
Checking on your child
Check your child during the night for rashes and to see if they are getting better. If a rash
appears, do the tumbler test (see below). If you are concerned that your child is not
improving phone the number on the front of this sheet to seek advice.
Keep your child away from nursery or school while they have a fever and notify the
school or nursery of the illness.
Alder Hey Children’s NHS Foundation Trust
Shared Learning Award submission – Feverish Illness in Children
The tumbler test
Do the 'tumbler test' if your child has a
rash. Press a glass tumbler firmly against
the rash. If you can see the spots
through the glass and they do not fade
this is called a ‘non-blanching rash’. If
this rash is present seek medical advice
immediately. The rash is harder to see
on dark skin so check paler areas, such
as palms of the hands, soles of the feet,
tummy and inside the eyelids.
(Photo courtesy of the Meningitis Research Foundation)