13: Skin - Gateshead

13: Skin
Please select a topic:
13.2 Emollient and barrier preparations
13.4 Topical corticosteroids
13.6 Acne and rosacea
13.8 Sunscreens and camouflagers
13.10 Anti-infective skin preparations
13.11b Other preparations
13.3 Topical local anaesthetics and antipruritics
13.5 Preparations for eczema and psoriasis
13.7 Preparations for warts and calluses
13.9 Shampoos and some other scalp preparations
13.11a Disinfectants and skin cleansers
13.13 Wound management products and elastic hosiery
Changes to the Formulary since previous version
(5.10.12)
Section Reason for change
13.5
13.6
Change
ADDED: Oral retinoids – reminder of measures to minimise teratogenic risk
ADDED: Dianette®: balance of benefits & risks remains positive
MHRA Drug Safety Alert
MHRA Drug Safety Alert
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 1 of 25
Drug Formulary
Date: 19.7.2013
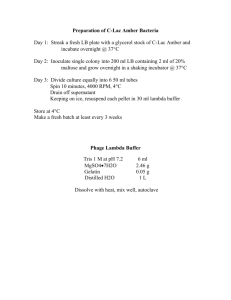
13.1 Management of skin conditions
The vehicle used in topical preparations influences skin hydration, has a mild antiinflammatory effect and facilitates penetration of the active component.
Creams are more cosmetically acceptable than ointments. Gels are suitable for application to
the face and scalp while lotions are used for moist conditions and hairy areas. Ointments are much less likely to sensitise and are suitable for chronic dry lesions.
Possible contact sensitivity to preservatives or antiseptics is the reason for the range of topical agents.
Body area Non-corticosteroid cream/ointment
(Qty based on twice daily application for 1 week in adults)
Corticosteroid cream/ointment
(Qty based on single daily application for 2 weeks in adults)
Face
Face and neck
Both hands
Scalp
Both arms
15 to 30g
25 to 50g
50 to 100g
100 to 200g
Both legs
Trunk
100 to 200g
400g
Groins and genitalia 15 to 25g
15 to 30g
15 to 30g
15 to 30g
30 to 60g
100g
100g
15 to 30g
Fire Hazard with Paraffin-based Emollients
Emulsifying ointment or 50% liquid paraffin and 50% white soft paraffin ointment in contact with dressings and clothing is easily ignited by a naked flame. The risk will be greater when these preparations are applied to large areas of the body, and clothing or ointment become soaked with the ointment. Patients should be told to keep away from fire or flames and not to smoke when using these preparations. The risk of fire should be considered when using large quantities of any paraffin-based emollient.
For further information refer to NPSA Rapid Response Report 4 dated 26.November 2007
The following products are known to be paraffin based:
STEROIDS EMOLLIENTS
Betnovate ointment
Betnovate RD ointment
Cetreban Cream & bath additive
Dermol Cream, 500 lotion & 600 Bath Additive
Diprobase and Diprobath
Doublebase
E45 Cream and Bath Oil
Emulsifying Ointment
Epaderm
Hydromol Ointment and Bath additive
Oilatum Cream and Bath additive
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 2 of 25
Drug Formulary
Date: 19.7.2013
Yellow soft paraffin
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 3 of 25
Drug Formulary
Date: 19.7.2013
13.2 Emollient and barrier preparations
Emollients (moisturisers)
Aqueous cream 100g & 500g
Aveeno cream 100g
Balneum Plus cream 100g
Calmurid cream 100g
Cetraben emollient cream 500g
Dermol cream 500g
Diprobase cream 500g
Diprobase ointment 500g
E45 cream 50g & 100g
Emulsifying ointment 500g
Epaderm ointment 500g
Eucerin Intensive 10%w/w Urea Treatment Lotion 250ml
Hand cream 50g (STAFF USE ONLY)
Hydromol Ointment 125g & 500g
Oilatum cream 40g
Oilatum emollient 250ml
Oilatum Junior Cream 500ml & 1050ml
Yellow soft paraffin 15g
Dose
- Aqueous cream BP (emulsifying ointment 30%, phenoxyethanol 1% in freshly boiled and cooled
purified water) (100g): massage into skin 2-3 times daily; may be used as a soap substitute.
- Aveeno® cream (colloidal oatmeal in emollient basis) (100mL): apply as often as required.
- Balneum® Plus cream (urea 5%, lauromacrogols 3%): apply as often as required.
- Calmurid cream (urea 10%, lactic acid 5%): apply twice a day.
- Cetraben emollient cream (white soft paraffin 13.2%, light liquid paraffin 10.5%): apply twice a day.
- Dermol cream (Benzalkonium Chloride 0.1% w/w; Chlorhexidine Hydrochloride 0.1% w/w; Liquid
Paraffin 105% w/w; Isopropyl Myristate 10% w/w): apply as often as required
- Diprobase® cream (cetomacrogol 2.25%, cetostearyl alcohol 7.2%, liquid paraffin 6%, white
soft paraffin 15%) (50g tube, 500g dispenser): apply as often as required.
- Diprobase® ointment (liquid paraffin 5%, white soft paraffin 95%) (50g tube, 500g dispenser): apply as often as required.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 4 of 25
Drug Formulary
Date: 19.7.2013
- E45 Cream (light liquid paraffin 12.6%, white soft paraffin 14.5%, hypoallergenic anhydrous wool
fat 1% in self-emulsifying monostearin): apply as often as required.
- Epaderm® ointment (emulsifying wax 30%, yellow soft paraffin 30%, liquid paraffin 40%)
(125g, 500g): massage into skin as often as required; may be used as a soap substitute.
- Eucerin® Intensive cream (urea 10%): apply thinly and rub into area twice a day.
- Hydromol® ointment (yellow soft paraffin 30%, emulsifying wax 30%): apply as often as required; may be used as a soap substitute.
- Oilatum emollient (light liquid paraffin 63.4%): apply as often as required.
- Oilatum cream (light liquid paraffin 6%, white soft paraffin 15%): apply as often as required.
- Oilatum Junior Cream (light liquid paraffin 6%, white soft paraffin 15%)
- Yellow soft paraffin (yellow petroleum jelly): apply as often as required.
Prescribing notes
Choice is guided by individual patient tolerance, preference and ease of use. It is dependent on previous use and adverse skin reactions (some may cause irritation or burning so advise testing on a small area of skin first and stop if a reaction occurs).
Emollients soothe, smooth and hydrate the skin and are indicated for all dry scaling disorders.
Emollients should be applied regularly to maintain improvement; most are best applied after a shower or bath.
Use an oil-based emollient at night and during the day if skin is very dry/flaky.
Use a cream which is easier to apply and less greasy throughout the day to aid compliance.
These products, apart from white soft paraffin 50%/liquid paraffin 50%, may be used as soap substitutes by firstly wetting the skin, washing with the cream or ointment, then rinsing off.
If emollients are being applied to the whole body twice daily, children may need 250g – 500g per week and adults 500g per week.
It is most cost effective to prescribe emollients in very large quantities
Hydromol contains less additives that Epaderm.
Aqueous cream and emulsifying ointment should be used for washing only.
Preparations that come in a pump dispenser presentation are good when product needed for use at school as more hygienic.
Ointments should be used for dry skin and chronic eczema. Creams should be sued for acute inflammatory eczema.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 5 of 25
Drug Formulary
Date: 19.7.2013
Emollient bath additives
Aveeno bath oil 250ml
Balneum bath oil 200ml
Diprobath 500ml
Dermol 600 600ml
E45 emollient bath oil 500ml
Hydromol emollient bath additive 500ml
Oilatum emollient bath additive 500ml
Oilatum Plus bath additive 500ml
Cetraban emollient bath additive 500ml
Dose
- Cetraban Emollient bath additive (light liquid paraffin 82.8%) (500mL): add 1-2 capfuls to bath
(1/2 to 1 capful if child).
- Oilatum® Emollient bath additive (acetylated wool alcohols 5%, liquid paraffin 63.4%)
(250mL, 500mL): add 5-15 mL/bath (2.5-10mL if an infant).
- Balneum® bath oil (soya oil 84.75%) (200mL, 500mL, 1L): add 20mL/bath (5mL, if an infant).
- Aveeno® bath oil (colloidal oatmeal, white oat fraction in emollient basis (250mL): up to
30mL/bath (child, up to 30mL).
- Oilatum® Plus bath additive (benzalkonium chloride 6%, triclosan 2%, light liquid paraffin
52.5%) (500mL, 1L): 1-2 capfuls/bath (infant over 6 months, 1mL).
- Dermol® 600 Bath Emollient (benzalkonium chloride 0.5%, liquid paraffin 25%, isopropyl
myristate 25%) (600mL): up to 30mL/bath (infant up to 15mL).
- Hydromol® Emollient Bath Additive (isopropyl myristate 13%, light liquid paraffin 37.8%)
(500ml): up to 1-3 capfuls/bath.
- Diprobath® Bath Additive (isopropyl myristate 39%, light liquid paraffin 46%) (500ml): up to
25-50ml/bath.
- E45® Emollient Bath Oil (cetyl dimeticone 5%, liquid paraffin 95%) (500ml): up to 15ml/bath.
Prescribing notes
Bath additives with antiseptic should be used in patients with infected eczema.
Oilatum® Plus bath additive is not suitable for use in the shower.
Preparations containing benzalkonium chloride can cause skin irritation with continued use.
E45® Emollient Bath Oil contains no irritants or allergens.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 6 of 25
Drug Formulary
Date: 19.7.2013
Soap substitutes
Aqueous cream 100g & 500g
Emulsifying ointment 500g
Epaderm ointment 500g
Hydromol ointment 500g
Dermol 500 lotion 500ml
Dermol 200 shower emollient 200ml
Oilatum shower emollient gel 150g
Dose
- Emulsifying Ointment (emulsifying wax 30%, white soft paraffin 50%, liquid paraffin 20%)
- Aqueous cream BP (emulsifying ointment 30%, phenoxyethanol 1% in freshly boiled and cooled
purified water) (100g)
- Epaderm® ointment (emulsifying wax 30%, yellow soft paraffin 30%, liquid paraffin 40%)
(500g)
- Hydromol® ointment (yellow soft paraffin 30%, emulsifying wax 30%) (500g)
- Dermol 500 lotion (Benzalkonium Chloride 0.1% w/w; Chlorhexidine Hydrochloride 0.1% w/w;
Liquid Paraffin 2.5% w/w; Isopropyl Myristate 2.5% w/w): apply as often as required; may be used as a soap substitute.
- Dermol 200 shower emollient (Benzalkonium Chloride 0.1% w/w; Chlorhexidine Hydrochloride
0.1% w/w; Liquid Paraffin 2.5% w/w; Isopropyl Myristate 2.5% w/w): apply as often as required; may be used as a soap substitute.
- Oilatum shower emollient gel (light liquid paraffin 70%): apply as often as required.
Prescribing notes
Most emollients may be used as soap substitutes by firstly wetting the skin, washing with the cream or ointment, then rinsing off.
Doublebase® Emollient Wash Gel and E45® Emollient Wash Cream come in pump dispensers so are more hygiengic to use a school and home particularly if Dermol products are not tolerated. They are available on a non-formulary basis.
White soft paraffin 50%/liquid paraffin 50% is not suitable as a soap substitute.
Hydromol contains less additives than Epaderm®
Preparations containing benzalkonium chloride can cause skin irritation with continued use.
A convenient way to apply emulsifying ointment and Hydromol® ointment is as "soap balls", which are made by putting a scoop of the ointment into tubinette or stockinette.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 7 of 25
Drug Formulary
Date: 19.7.2013
Barrier preparations
Vasogen cream 50g
Drapolene cream 100g
Metanium ointment 30g
Dose
- Vasogen Cream (dimeticone 20%, calamine 1.5%, zinc oxide 7.5%)): for nappy and urinary rash and eczematous conditions, apply several times daily as necessary or after each nappy change.
- Drapolene Cream (benzalkonium chloride 0.01%, cetrimide 0.2% in a basis containing white soft
paraffin, cetyl alcohol and wool fat): for nappy and urinary rash and eczematous conditions, apply several times daily as necessary or after each nappy change.
- Metanium Ointment (titanium dioxide 20%, titanium peroxide 5%, titanium salicylate 3% in
basis containing dimeticone, light liquid paraffin, white soft paraffin, and benzoin tincture): for nappy and urinary rash and eczematous conditions, apply several times daily as necessary or after each nappy change.
Prescribing notes
Urinary (nappy) rash may clear if skin is left exposed to air; if associated with yeast
(candida) infection, an antifungal cream such as clotrimazole cream is useful.
For information on the use of Cavilon® please consult the separate Trust Wound Care
Formulary.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 8 of 25
Drug Formulary
Date: 19.7.2013
13.3 Topical local anaesthetics and antipruritics a) Topical antipruritics
Calamine lotion 200ml
Dose
- Calamine lotion: apply 2-3 times daily.
Prescribing notes
Emollient preparations may be useful for pruritus due to dry skin; sedating oral antihistamines may also be helpful for itch
(b) Topical local anaesthetics
LMX 4® cream
Dose
- LMX 4® cream (lidocaine 4%) (5g): for children & adults over 1 month, anaesthesia before e.g. venepuncture, apply a thick layer under an occlusive dressing 30 minutes before procedure
Prescribing notes
Topical local anaesthetics may be absorbed through mucosal surfaces.
Local anaesthetics may occasionally cause sensitisation.
For information on the use of Ethyl Chloride Spray please consult the Anaesthetics Chapter of the formulary.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 9 of 25
Drug Formulary
Date: 19.7.2013
13.4 Topical corticosteroids
Hydrocortisone 0.5% and 1% cream
Hydrocortisone 0.5% and 1% ointment
Hydrocortisone 1% plus clotrimazole 1% cream (Canesten HC)
Hydrocortisone 0.5% plus nystatin and chlorhexidine cream (Nystaform HC)
Hydrocortisone 0.5% plus nystatin and chlorhexidine ointment (Nystaform HC)
Hydrocortisone 0.5% plus nystatin, benzalkonium and dimeticone (Timodene)
Hydrocortisone 1% plus miconazole 2% (Daktacort)
Betamethasone valerate 0.1% cream (Betnovate) 100g & 30g
Betamethasone valerate 0.1% ointment (Betnovate) 100g & 30g
Betamethasone valerate 0.1% scalp application (Betnovate)
Betamethasone valerate 0.025% cream (Betnovate RD) 100g
Betamethasone valerate 0.025% ointment (Betnovate RD) 100g
Betamethasone valerate 0.1% plus clioquinol 3% ointment (Betnovate C)30g
Betamethasone valerate 0.1% plus neomycin 0.5% cream (Betnovate N) 30g
Betamethasone valerate 0.1% plus neomycin 0.5% ointment (Betnovate N) 30g
Clobetasol propionate 0.05% cream (Dermovate) 30g
Clobetasol propionate 0.05% ointment (Dermovate) 30g
Clobetasone butyrate 0.05% cream (Eumovate) 30g & 100g
Clobetasone butyrate 0.05% ointment (Eumovate) 30g & 100g
Clobetasone butyrate 0.05%, oxytetracycline and nystatin 0.05% ointment (Trimovate) 30g
Fluocinolone 0.025% ointment (Synalar) 30g
Dose
- Topical corticosteroids should be applied thinly as follows:
Mild steroids = 1-2 times daily.
Moderate, Potent & Very potent steroids = 1 x daily.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 10 of 25
Drug Formulary
Date: 19.7.2013
Prescribing notes
Topical corticosteroids are divided into four groups according to potency (see table) below).
Mild or moderately potent corticosteroids should control most cases of eczema. Therapy should be stepped-down once control achieved.
Potency
Mild
Examples
Hydrocortisone 0.5% and 1%
Hydrocortisone with antimicrobials
Fluocinolone acetonide
0.0025%
Trade Name
Non-proprietary
Canesten HC, Timodene,
Dakatacort, Vioform-HC
Synalar 1 in 10
Moderate
Potent
Betamethasone 0.025%
Clobetasone butyrate 0.5%
Clobetasone with antimicrobials
Betnovate RD
Eumovate
Trimovate
Fluocinolone acetonide
0.00625% Synalar 1 in 4
Betamethasone 0.1%
Betamethasone 0.1% with antimicrobials
Betnovate
Fluocinolone acetonide 0.025% Synalar
Betnovate C, Betnovate N
Clobetasol propionate 0.05% Dermovate Very Potent
Topical corticosteroids are not recommended in urticaria, rosacea, acne or undiagnosed, possibly infective, disorders.
Topical corticosteroids must not be applied more than twice a day.
To minimise the risk of side-effects, the smallest effective amount should be used, reducing strength and frequency of application as the condition settles. The risk of systemic sideeffects increases with prolonged use on thin, inflamed or raw skin surfaces, use in flexures, or use of more potent corticosteroids. Occlusion increases efficacy and side-effects. Only mild corticosteroids should be used on the face.
Gloves should be worn during, or hands washed after, application of large quantities of steroid preparations.
The occlusive effect of ointments increases penetration of the corticosteroid.
Cream based preparations contain preservatives.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 11 of 25
Drug Formulary
Date: 19.7.2013
Topical corticosteroids should not be used on infected skin unless the infection is being treated.
Antibacterials and antifungals with corticosteroids may have a role if there is associated infection.
Palms and soles may require potent or very potent steroids.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 12 of 25
Drug Formulary
Date: 19.7.2013
13.5 Preparations for eczema and psoriasis
Preparations for eczema
PB7 Viscopaste bandages
Prescribing notes
Medicated bandages are flammable
All patients with eczema should use an emollient and soap substitute and/or bath oil.
Emollients with antiseptics should be used to in patients with infected eczema.
Exacerbation of eczema may represent secondary bacterial or viral infection. Appropriate swabs should be taken, and topical antibacterials applied. Systemic antibiotics may be required in widespread infected eczema.
Ciclosporin, azathioprine or systemic corticosteroids should be initiated on specialist advice only, with responsibility for monitoring agreed.
Topical corticosteroids should be reduced and withdrawn as the condition settles.
Sedating antihistamines may be used short-term for pruritus.
Preparations for psoriasis
Acitretin 10mg and 25mg capsules
Exorex lotion 100ml (prepared coal tar 1% in an emollient basis)
Calcipotriol 50microgram/gram cream 60g (Dovenex®)
Prescribing notes
Treatment choice depends on site, extent of psoriasis and patient preference and tolerance.
Potent and very potent topical corticosteroids should be used on specialist advice only; they may precipitate unstable and pustular psoriasis after stopping.
Phototherapy, methotrexate, ciclosporin, acitretin should be initiated on specialist advice only, with responsibility for monitoring agreed.
Drugs affecting the immune response
Ciclosporin 25mg, 50mg and 100mg capsules
Methotrexate 2.5mg tablets
Tacroliumus 0.03% ointment
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 13 of 25
Drug Formulary
Date: 19.7.2013
13.6 Acne and rosacea
Preparations for acne
Isotretinoin 5mg and 20mg capsules (on advice on specialist only)
Dianette tablets
Prescribing notes
Topical treatment takes at least 30 days to become effective.
Benzoyl Peroxide is available to prescribe by GPs or for sale over the counter.
Topical antibiotics are as effective as oral antibiotics but encourage resistance and are more expensive.
Topical retinoids are recommended for comedonal acne; they may initially cause redness of the skin.
Oxytetracycline may take up to 6 months of compliant use to achieve maximum benefit.
Dianette® (cyproterone acetate with ethinylestradiol) is a treatment for severe acne and only in those patients may it also be used as an oral contraceptive. In those who do not require contraception, Dianette® should be withdrawn 3-4 cycles after the treated condition has completely resolved. If ongoing contraception is required, substitution with another COC is likely to maintain the improvement.
Some drugs, including enzyme-inducers and antibiotics, may impair the efficacy of oral contraceptives; see BNF for details.
Doxycycline can cause photosensitivity in some patients. Minocycline may be an alternative but prolonged use should be avoided due to the rare risk of liver damage; liver function tests should be monitored 3 monthly.
Tetracyclines and retinoids (systemic or topical) must be avoided in pregnancy.
Severe acne requires oral antibiotics and referral for consideration of isotretinoin for treatment failures. Oral isotretinoin (Roaccutane®) is a toxic and teratogenic drug that is only prescribable by a consultant dermatologist.
There is no effective treatment for redness of the skin due to rosacea; camouflagers may be required.
Mild rosacea is best treated with a topical agent.
Pustular rosacea is best treated with systemic antibiotics.
MHRA Drug Safety Update
Cyproterone acetate with ethinyloestradiol (co-cyprindiol): balance of benefits and
Article date: June 2013
Summary risks remain positive – updated prescribing advice
Following a Europe-wide review of cyproterone acetate with ethinylestradiol (co-cyprindiol), the balance of benefits and risks of Dianette (brand leader) and its generics remains positive. To
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 14 of 25
Drug Formulary
Date: 19.7.2013
further improve the benefit-risk balance some important changes have been made to clarify the indication—these are discussed below. Although the indications for co-cyprindiol relate to androgen-sensitive skin conditions and hirsuitism, the medicine also provides effective contraception for women who require it. Use of additional hormonal contraception with cocyprindiol is therefore contraindicated. The risk of venous thromboembolism is rare, but healthcare professionals and patients should remain vigilant for signs and symptoms of this important side effectine.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON287002
MHRA Drug Safety Update
Oral retinioids: pregnancy prevention – reminder of measures to minimise teratogenic risk
Article date: June 2013
Summary
The risk of foetal malformation with oral retinoids is extremely high, even when used at a low dose or for a short time during pregnancy. All oral retinoids have an associated Pregnancy
Prevention Programme (PPP), which is supported by educational material for prescribers, pharmacists, and patients. Women of child-bearing potential should have pregnancy excluded before starting treatment. While taking these medicines, one—or preferably two—different forms of contraception must be consistently used.
Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON287004
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 15 of 25
Drug Formulary
Date: 19.7.2013
13.7 Preparations for warts and calluses
Cuplex gel 5g (salicylic acid 11%, lactic acid 4% in collodion basis)
Silver nitrate caustic pencil 95%
Salicyclic acid 10% in colloidion solution (chiropody)
Imiquimod 5% cream 5g
Prescribing notes
These preparations are contra-indicated in facial or genital warts.
The wart surface should be rubbed with a file or pumice stone, and the surrounding skin protected, before each application. If application becomes painful, treatment should be withheld for a few days then recommenced.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 16 of 25
Drug Formulary
Date: 19.7.2013
13.8 Sunscreens and camouflagers
Uvistat SPF 30 125g
Uvistat SPF 50 125g
Prescribing notes
Sunscreens with SPF > 15 are prescribable for photosensitive skin disorders including genetic disorders, vitiligo, following radio-therapy, photo-aggravated rosacea, or recurrent herpes simplex labialis.
Prescriptions should be endorsed "ACBS".
The choice of sunscreens depends on individual patient need, tolerance and evidence of sensitivity to excipients.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 17 of 25
Drug Formulary
Date: 19.7.2013
13.9 Shampoos and some other scalp preparations
Polytar shampoo 250ml
Ketoconazole 2% shampoo 120ml
Cocois scalp ointment 40g
Oilatum shampoo
Eucerin Dry Scalp Relief shampoo with 5% urea
Dose
- Ketoconazole 2% shampoo (120mL): for seborrhoeic dermatitis and dandruff apply twice weekly for 2-4 weeks; for pityriasis versicolor, once daily for up to 5 days.
- Cocois® scalp ointment (coal tar solution 12%, salicylic acid 2%, precipitated sulphur 4% in a
coconut oil emollient basis): for scaly scalp disorders including psoriasis, eczema, seborrhoeic dermatitis and dandruff, apply to scalp once weekly as necessary, shampoo off after 1 hour.
- Polytar® liquid (arachis (peanut) oil extract of crude coal tar 0.3%, cade oil 0.3%, coal tar
solution 0.1%, oleyl alcohol 1%, tar 0.3%) (250mL): scalp disorders, including psoriasis, seborrhoea, eczema, pruritus and dandruff, apply 1-2 times weekly.
-
Oilatum® shampoo: Wet the hair and massage OILATUM Scalp Treatment gently over the scalp to produce a lather. Leave on for 3-5 minutes. Rinse thoroughly, and repeat if necessary. Use twice weekly for two weeks to clear the scales and improve the condition of your scalp. Then just use once a week to maintain a clear scalp.
Prescribing notes
Shampoo formulations are preferred for moderate scaly slap conditions whereas more severe conditions may require an ointment.
Ketoconazole shampoo is often helpful for seborrhoeic dermatitis of the scalp.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 18 of 25
Drug Formulary
Date: 19.7.2013
13.10 Anti-infective skin preparations
Antibacterial preparations
Mupirocin 2% ointment 15g
Silver sulfadiazine 1% cream 50g (Flamazine®)
Fusidic acid 2% cream 15g
Fucidin-H cream 15g
Metronidazole 0.75% gel (Anabact) 15g
Potassium permanganate solution tablets 400mg (Permitabs®)
Octenisan
Oilatum Plus
Dermol 600
Dose
- Fusidic acid 2% cream, gel; sodium fusidate 2% ointment (15g, 30g): apply 3-4 times daily.
- Metronidazole gel 0.75% : apply 1-2 times daily.
- Silver sulfadiazine cream 1% (20g, 50g, 250g, 500g): burns, apply daily or more frequently if required; leg ulcers, apply every 1 to 2 days; fingertip injuries, apply every 2-3 days.
- Potassium permanganate solution tablets 400mg (Permitabs®): 1 tablet dissolved in 4 litres of water provides a 0.01% (1 in 10,000) solution.
- Mupirocin 2% ointment; cream (15g): apply up to 3 times daily for up to 3 days.
- Fucidin H cream (hydrocortisone acetate 1%, fusidic acid 2%): apply 1-2 times daily.
Prescribing notes
Topical antibiotics should only be used short-term and for localised infections.
If potassium permanganate tablets are prescribed, ensure tablets are dissolved in a jug prior to being poured into the bath as direct contact with the skin can cause burning.
Antifungal preparations
Clotrimazole 1% cream 20g
Canesten-HC cream 30g
Amorolfine 5% nail lacquer 5ml
Nystatin 100 000 unit/g cream 30g
Miconazole 2% cream 15g & 30g
Dose
- Clotrimazole cream 1% (20g): apply 2-3 times daily.
- Terbinafine cream 1% (30g): apply 1-2 times daily.
- Clotrimazole HC cream 1% (20g)(clotrimazole 1%, hydrocortisone 1%): apply 2-3 times daily.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 19 of 25
Drug Formulary
Date: 19.7.2013
- Amorolfine nail lacquer 5% (5ml): apply 1-2 weekly.
- Miconazole cream 2% (30g): apply 1-2 times daily.
Antiviral preparations
Aciclovir 200mg and 400mg tablets
Parasiticidal preparations
Malathion 0.5% in an aqueous basis (Derbac-M) 50ml
Permethrin 5% dermal cream (Lyclear) 30g
(a) Scabies
Dose
- Malathion 0.5% liquid in an aqueous basis (Derbac-M®) (50ml): apply over whole body and wash off after 24 hours; if hands are washed with soap within 24 hours they should be retreated. In young children, application may need to be extended to the face, neck, scalp and ears; this extended application may also be necessary for the elderly, immunocompromised and those who have experienced treatment failure.
- Permethrin 5% dermal cream (Lyclear® Dermal Cream, 30g): apply over whole body and wash off after 8-12 hours. In young children, application may need to be extended to the face, neck, scalp and ears; this extended application may also be necessary for the elderly, immunocompromised and those who have experienced treatment failure. If hands are washed with soap within 8 hours of application, they should be treated again with cream.
Prescribing notes
Aqueous preparations are preferable to alcoholic lotions.
All members of the household and close contacts should be treated.
Clothes and bedlinen should be washed at normal temperatures at time of treatment.
In pregnancy, malathion in an aqueous basis is preferred.
(b) Head lice
Dose
- Malathion 0.5% liquid in an aqueous basis (Derbac-M®) or alcoholic basis (Prioderm® lotion)
(50ml): rub into dry hair and scalp, allow to dry naturally, remove by washing after 12 hours.
Prescribing notes
Head lice should be treated with lotion or liquid formulations; shampoos are diluted too much during use to be effective and should not be used. Products with short application times (e.g. cream rinse & mousse formulations) are not recommended.
A second application 7 days after the first is needed.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 20 of 25
Drug Formulary
Date: 19.7.2013
Aqueous formulations are preferred in severe eczema, asthmatic patients and small children.
A rotational policy for insecticides is outmoded; a mosaic strategy is suggested whereby if a course of treatment fails then a different insecticide is used for the next course.
Malathion should not be applied at intervals of less than 1 week or for more than 3 consecutive weeks since effectiveness is not increased.
In pregnancy, dimeticone or wet combing are preferred. If malathion is required the liquid in aqueous basis should be used.
Malathion should not be applied at intervals of less than 1 week or for more than 3 consecutive weeks since effectiveness is not increased.
Permethrin is not recommended for the treatment of head lice since currently available formulations are diluted too much during use.
(c) Crab lice
Dose
- Malathion 0.5% aqueous liquid (Derbac-M®) (50mL): apply over whole body, allow to dry naturally, wash off after 12 hours or overnight.
Prescribing notes
An aqueous preparation should be applied to all parts of the head and body for 12 hours or overnight; a second treatment is needed after 7 days to kill lice emerging from surviving eggs.
Alcoholic lotions are not recommended due to irritation of excoriated skin and genitalia.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 21 of 25
Drug Formulary
Date: 19.7.2013
Preparations for minor cuts and abrasions
Proflavine cream BPC 100ml (Theatres only)
Prescribing notes
For information on the use of Cavilon® and Opsite® please consult the separate Trust
Wound Care Formulary.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 22 of 25
Drug Formulary
Date: 19.7.2013
13.11 Disinfectants and cleansers
Alcohols and saline
Methylated spirit external solution 70%
Sodium chloride 0.9% sachets 100ml (Normasol)
Isopropyl alcohol swabs
Chlorhexidine salts
Chlorhexidine gluconate 0.05% sachet (Unisept) 25ml & 100ml
Chlorhexidine gluconate 0.5% solution (Hibisol and Hydrex) 500ml
Chlorhexidine gluconate 4% surgical scrub (Hydrex) 500ml
Chlorhexidine gluconate 1% obstetric cream 250g
Chlorhexidine gluconate 0.015% and cetrimide 0.15% solution 1L (Travasept)
Chlorine and iodine
Povidone iodine 7.5% surgical scrub(Videne) 500ml
Povidone iodine 2.5% dry powder spray (Betadine) 150g
Povidone iodine 10% ointment (Betadine) 80g
Povidone iodine 10% antiseptic solution (Videne) 500ml
Povidone iodine 10% alcoholic antiseptic solution (Videne) 500ml
Other
Oilatum Plus 500ml
Octenisan 450ml
Astringents, oxidisers and dyes
Hydrogen peroxide 3% solution 200ml
Prescribing notes
Sodium chloride solution 0.9% is suitable for irrigation of skin and wounds.
Povidone-iodine may produce systemic adverse effects, such as metabolic acidosis, hypernatraemia and renal impairment, if applied to large wounds or severe burns.
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 23 of 25
Drug Formulary
Date: 19.7.2013
Other preparations
Infacare bath solution 500ml
Iodine alcoholic solution BP 25ml
Plaster remover solution 50ml
Sterile water for irrigation 1L
Sodium dichloroisoocyanurate external tablets (Haz-tabs)
Sodium hypochlorite 2% solution 500ml (Milton)
Sodium chloride 0.9% for irrigation 1L
Aluminium chloride hexahydrate 20% roll-on 60ml
Hirudoid cream 50g
Lubricating jelly 42g & sachets
Gigasept PA solution 5L
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 24 of 25
Drug Formulary
Date: 19.7.2013
13.13 Wound management products and elastic hosiery
See separate wound management formulary
Red = Hospital use only
Green = GP & Hospital use. Drugs not classified as Red, Amber or Amber 2 are classified as Green by default
Amber 1 = Drugs with shared care agreement
Amber 2 = Initiated by Hospital specialist only
Gateshead Health NHS Foundation Trust Page 25 of 25
Drug Formulary
Date: 19.7.2013