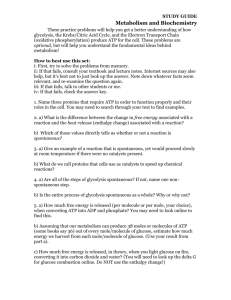
Objectives 26
advertisement

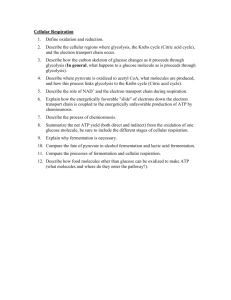
INTRODUCTION - human tumors are heterogeneous in perfusion large volumes of tumors are chronically hypoxic - oxygen is necessary for energy production via mitochondrial respiration - absence of oxygen tumor cells have to produce energy via anaerobic glycolysis leads to acidosis of tumor tissues and both hypoxia and acidosis lead to more aggressive tumor phenotypes 1. PASTUER AND WARBURG EFFECTS - blood vasculature delivers glucose and oxygen to tissues; glucose diffuses to cells in tissues where it is taken up via specific glucose transporters (GLUT1); once inside cells, glucose metabolize via glycolysis to pyruvate; in this oxidative process H+ is released - at pyruvate continued to oxidizing pyruvate to CO2 (hydrated to HCO3- + H+) via citric acid cycle and mitochondrial respiration or re-reduce it to lactate (transported out of cell) - H+ ions produced in both cases result is an acid load on tissue - tumor cells consume more glucose for energy production via anaerobic glycolysis when oxygen perfusion is diminished (anaerobic conditions) - 18X more energy from one glucose molecule is derived aerobically when compared to anaerobic glycolysis - Pasteur effect inhibition of glycolysis by oxygen; this inhibition is mediated quickly (the cells respond immediately to the presence of oxygen) - Warburg noted that the extent to which tumors produce acid under aerobic conditions is remarkable; he showed that tumors consume glucose rapidly and produce large amounts of lactic acid (even under aerobic conditions) Warburg effect 2. FdG PET shows high glycolysis in tumors - positron emission tomography (PET) can accurately pinpoint source of positron-emitting isotopes - positrons are positively charged electrons produced when a proton decays to a neutron; these positrons migrate and reaction with electron in an annihilation reaction result is two gamma rays (511 keV in energy) and radiate 180 degrees apart - these gamma rays pass through tissue and are captured by a ring of detectors, which are set up to register events that occur simultaneously in two detectors at the same time (coincidence detection) line drawn between two detectors; more lines pinpoint source of positronemitting isotopes - 18F (isotope) attached to glucose analog, deoxy-glucose fluorodeoxyglucose (FdG) transported by GLUT-1 and trapped in cells by phosphorylation - tissues that are actively consuming glucose show up positive in FdG PET scans - conclusion virtually all metastatic cancer have elevated rate of glucose uptake; FdG PET has high sensitivity and high specificity Tumor perfusion - tumor perfusion is heterogeneous and is illustrated by technique called dynamic contrast enhanced MRI (DCE-MRI) - patient injected with contrast reagent (CR), contains chelate lanthanide ion, gadolinium; gadolinium enhances the magnetization such that signal intensity is higher in volumes that contain gadolinium - volumes with highest perfusion take up more CR and have highest signal intensity - time-dependent enhancement affected by: 1.) vascular volume and 2.) vascular permeability - first component CR in vasculature increases rapidly and decreases slower due to recirculation-dilution and through kidney clearance magnitude of peak is directly proportional to the vascular volume in the individual pixel - second component leakage of CR from blood interstitium, which is affected by permeability and the surface area of the blood vessel endothelium Perfusion and Angiogenesis - angiogenesis is sprouting and growth of new blood vessels; requirement for tumor growth (drug targets) - angiogenic tissue is poorly perfused though; vascular beds that are normally finely tuned such that the resistances across capillary banks are balanced such that flow occurs evenly - angiogenesis in tumors occurs in the absence of a defined morphogenetic gradient such that it results in long, tortuous vessels (series, high resistance) or in shunts and extra capillaries (parallel, low resistance) resistances are no longer balanced blood flow is unevenly shunted to beds with lower resistance - excessive angiogenesis heterogeneous perfusion - angiogenesis induced by specific growth factors: fibroblast growth factor (b-FGF), vascular endothelial growth factor (VEGF) and angiopoeitins, Ang-1 and Ang-2 - VEGF induced by hypoxia induces growth of new vessels which relieve hypoxia generates balanced vasculature HYPOXIA INDUCIBLE FACTOR (HIF) - HIF is the major TF responsible for VEGF induction - HIF also induces expression of erythropoietin (EPO) expression; HIF is a major transcription factor (TF) regulating expression of proteins involved in energy metabolism, iron metabolism, and angiogenesis HIF-1 is a dimeric transcription factor - HIF TF is a dimer comprised of HIF-1alpha and HIF-1beta subunits - HIF-1beta subunits is thought to be constitutively and ubiquitously expressed - HIF-1alpha is also constitutively expressed, yet its levels are reduced in presence of oxygen - absence of oxygen HIF-1alpha increases to levels where it can combine with HIF-1beta to form an active transcription factor complex binds to DNA containing sequence CCGCT (hypoxia response element, HRE) glycolytic enzymes, EPO, VEGF increased glycolysis, increased angiogenesis (VEGF), increased RBCs (EPO, iron) HIF-1alpha is regulated by oxygen dependent proteolysis - reduction of HIF-1alpha in presence of oxygen mediated by cytosolic prolyl hydroxylase, PH (family of iron sulfur hydroxylases that contains the ER prolyl hydroxylase used in the maturation of collagen) - oxygen present PH hydroxylates two proline residues on HIF-1alpha hydroxylated HIF-1alpha subunits are recognized by a ubiquitin ligase (vH-L protein, its gene is an oncogene) transfers ubiquitin polypeptides to HIF-1alpha polyubiqiunated HIF-1alpha recognized by 28S proteosome (its gene is an oncogene) that is responsible for degradation/turnover of cytoplasmic proteins - genetic defects in vH-L lead to hereditary renal cell carcinoma (von Hippel-Lindau syndrome) Coordinated regulation of glucose metabolism, iron metabolism, and angiogenesis by HIF1 - three categories of genes know to be upregulated by HIF-1: energy metabolism, iron metabolism, angiogenesis (vasoactive proteins), and hormones/receptors - genes of energy metabolism exclusively involved in regulation of glucose metabolism; a lack of oxygen compensated by upregulation of glycolysis provides cells with energy in absence of oxygen - iron metabolism upregulated because iron is essential in hemoglobin and myoglobin for transport of oxygen to tissues - vasoactive proteins induce angiogenesis (VEGF) or increase vessel tone promotes movement of solutes form blood interstitium HIF-1alpha is dysregulated in cancers - genetic defects in vH-L cause constitutive upregulation of HIF (familial renal cell carcinoma) - HIF is elevated in many cancers (not a direct consequence of hypoxia); HIF remains elevated under normoxic conditions - continued expression of HIF-1alpha under normoxic conditions means that tumors continue to produce VEGF (even if they are adequately oxygenated); this products disrupts normal morphogenetic gradients for angiogenesis and will lead to imbalanced vasculature (which is a hallmark of all tumors) - overproduction of HIF-1alpha also be responsible for the Warburg effect and the elevated uptake of glucose observed in virtually all metastatic tumors THE HOSTILE TUMOR MICROENVIRONMENT - tumors are heterogeneously perfused gives rise to significant volumes that are hypoxic/acidic and substrate-limited - such microenvironmental conditions have significant impact in the genotypic/phenotypic characteristics of tumors, including altered gene expression, increase metastasis, and therapy resistance - only a few of these are due to alteration in HIF-1alpha - look at table for therapeutic consequences of this microenvironment 26-8