Planning Notes for DRG Optimization Workshop
advertisement

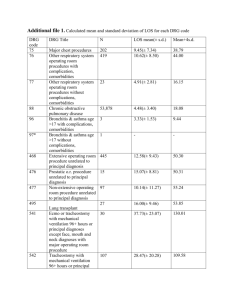
DRG Optimization Workshop Planning Notes Planning Notes for DRG Optimization Workshop Title: DRG Optimization Workshop Objective: To provide an in-depth, analytic approach to the process of enhancing inpatient reimbursement through better DRG Coding including an overall understanding of the DRG system, its development and utilization. Various severity refined DRGs along with update material for 2002 HCFA-DRGs, 2002 ICD-9-CM changes, APCs, ICD-10-CM and current HCFA compliance efforts will be reviewed. Upon Completion the Participants Will: 1. Understand the overall development and refinement of the DRG Payment System as it is used by HCFA. 2. Appreciate the DRG Grouping Logic and how it affects inpatient reimbursement. 3. Understand the necessity for correct ICD-9-CM Coding (diagnoses and procedures) for proper reimbursement under DRGs. 4. Have reviewed the 2001 update for both the HCFA-DRG System and the new and changed ICD-9-CM codes. 5. Be able to delineate the systematic steps in assessing and addressing DRG assignment. 6. Understand the importance of proper DRG assignment and the optimization process for reimbursement under the DRG system. 7. Have knowledge of computer groupers and optimizers and their utilization. 8. Understand and appreciate the knowledge, background and capabilities of personnel coding for and optimizing reimbursement under DRGs. 9. Appreciate the differences between 'concurrent' coding and 'after-the-fact' coding for DRG assignment. 10. Appreciate the current compliance efforts in the DRG area currently underway by the OIG, DOJ and HCFA. October 2001 Page - 1 - DRG Optimization Workshop Planning Notes 11. Have reviewed the interface of the DRG payment system to the outpatient payment reform in the form of APCs (Ambulatory Payment Classifications). 12. Appreciate the research being performed relative to systems such as AP-DRGs and APR-DRGs, and other severity refined DRGs. 13. Understand the changes that will be made in transitioning to ICD-10-PCS and ICD10-CM. 14. Be able to relate the DRG process to areas such as UR, QA, physician documentation and cost accounting. 15. Have knowledge of the future changes that are anticipated for the DRG system. Audience: Hospital coders, medical records personnel, data processing support personnel, business office personnel, insurance clerks, nursing supervisors, nurses as appropriate, and administrative staff as appropriate. Method of Presentation: The primary method is Lecture-Recitation with the use of case studies. Interaction and questions from the audience are HIGHLY encouraged. Exercises in the form of coding scenarios will be used. Course Materials: Extensive Class Notes (including copies of Overhead Transparencies). Class Notes will include copies of selected readings and special materials as appropriate. Student Materials: ICD-9-CM Manuals. DRG Assignment Manuals (if available). Laptop computer DRG Groupers and/or Optimizers are welcome. Course Times: 9:00 a.m. to 12:00 p.m., 1:00 p.m. to 4:00 p.m. Outline: I. Introduction A. The DRG System B. Historical Development and Utilization C. The Future of the DRG System 1. SR-DRGs 2. AP-DRGs October 2001 Page - 2 - DRG Optimization Workshop Planning Notes 3. APR-DRGs D. DRGs and APCs E. ICD-10-PCS and ICD-10-CM II. DRG Assignment Process A. Use of ICD-9-CM Coding 1. Diagnoses 2. Procedures B. Use of Groupers C. Related DRGs D. Medical Record Reviews E. Complications & Comorbidities F. Special Parameters 1. Relative Weight 2. GMLOS 3. Outlier Threshold G. Special Resources 1. Computer Optimizers 2. Reference Optimizers III. Reimbursement Process Under DRGs A. Systematic Process B. Calculation Examples C. Differences In Payment For Better DRGs D. Case-Mix Index Considerations IV. 2002 Update A. New/Changed ICD-9-CM Codes B. 2002 DRG Update 1. Payment Rates 2. New Rules/Regulations 3. Transfer Situation V. Compliance And Overcoding For DRGs A. Determination Of Principal Diagnosis B. Upcoding and Monitoring C. Justifying Secondary CCs D. 72-Hour Pre-Admission Rule E. HCFA As Secondary Payer VI. DRGs and APCs October 2001 Page - 3 - DRG Optimization Workshop Planning Notes A. Overview of APCs B. Commonality of DRGs and APCs C. Payment System Interface VII. DRG Optimization Case Studies (Selected Areas) A. Nervous System B. Ear, Nose, Mouth & Throat C. Respiratory System D. Circulatory System E. Digestive System F. Musculoskeletal System G. Endocrine System H. Neoplasms IX. Severity Refined And Modified DRG Systems A. Introduction 1. Refinement Processes 2. 'Severity' Versus 'Mortality' Concerns A. HCFA's SR-DRGs 1. Special Report 2. Important Features B. New York's AP-DRGs 1. Pediatric Modified DRGs 2. Key Features C. 3M's APR-DRGs 1. Development 2. Key Features D. Optimizing Reimbursement Under The 'New' Systems X. Physician Involvement in DRG Coding A. After-The-Fact Coding B. Concurrent Coding C. Interacting With Physicians D. Pros & Cons For Different Approaches XI. DRGs And Related Areas A. Utilization Review/Quality Assurance B. Cost Reporting Process C. Medical Records D. PRO Review E. Cost Accounting & Internal Studies October 2001 Page - 4 - DRG Optimization Workshop Planning Notes XII. DRGs and The Future A. ICD-10-PCS B. ICD-10-CM B. "H-Codes" Notes: 1. This is an intensive one-day workshop emphasizing practical applications. 2. Questions submitted prior to the class are encouraged! 3. Reference materials, including actual cases, will be made available to class participants as a part of their notes. October 2001 Page - 5 -