Medical History Form
advertisement

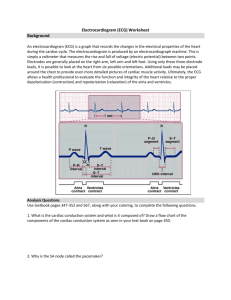
Medical History Form FORM CODE: MHX VERSION:A 02/10/10 ID NUMBER: Contact Occasion 0 1 SEQ # Administrative Information / 0a. Completion Date: Month / 0b. Staff ID: Day Year Part 1 Instructions: Part 1 of this form is completed by participant-response. Affix the participant ID label above. 1. Prior Angina ............................................................. No Yes [“Angina” refers to evidence or knowledge of symptoms before this acute event described as chest pain or pressure, jaw pain, arm pain, or other equivalent discomfort suggestive of cardiac ischemia] 1a. If YES, then choose one of the following: Existed > 2 weeks before admission Existed ≤ 2 weeks before admission 2. Previous Myocardial Infarction ............................... No [Diagnosed by physician and hospitalized for myocardial infarction] Yes 3. Prior Percutaneous Coronary Intervention ............ Yes / 3a. If YES, most recent PCI date: Month / Day 4. Prior Coronary Artery Bypass Surgery .................. / 4a. If YES, most recent CABG date : Month No Year No Yes / Day 5. History of Stroke...................................................... Year No 5a. If YES, then answer the following: Hemiplegia: ......... Yes No Yes 6. History of TIA ........................................................... No Yes [A focal neurological deficit (usually corresponding to the territory of a single vessel) that resolves spontaneously without evidence of residual symptoms at 24 hours] 7. History of peripheral arterial disease .................... No Yes [Peripheral arterial disease can include the following: (1) Claudication (pain in the muscles in the back of the legs), either with exertion or at rest (2) Amputation for arterial vascular insufficiency (3) Vascular reconstruction, bypass surgery, or percutaneous intervention to the extremities (4) Documented aortic aneurysm (5) Positive noninvasive test (e.g., ankle brachial index less than 0.8). Medical History (MHX) Page 1 of 11 ID #: 8. Do you have a history of congestive heart failure? ..................... No Yes 8a. If YES, then classify heart failure: NYHA Class I – No symptoms and no limitation in ordinary physical activity (e.g. shortness of breath when walking, climbing stairs etc). NYHA Class II – Mild symptoms (mild shortness of breath and/or angina) and slight limitation during ordinary activity. NYHA Class III – Marked limitation in activity due to symptoms, even during less-than-ordinary activity. Comfortable only at rest. NYHA Class IV – Severe limitations. Experiences symptoms at rest. Inability to carry out physical activity or symptoms at rest. 9. Do you currently smoke or have you smoked in the past? . No Yes If YES, answer the following: 9a. Current (within 1 month) Recent (stopped 1 month to 1 year prior) Former (stopped > 1 year prior) 9b. Years of smoking: 9c. Cigarettes smoked per day: cigarettes per day (1 = 1 or fewer per day) 10. Do you have a family history of coronary disease? ........... No Yes (As documented by direct blood relatives – parents, siblings, children – who have had any of the following before age 55: 1) angina, or 2) myocardial infarction, or 3) sudden cardiac death without obvious cause) In the seven days prior to this visit today: 11. Were you exercising regularly? ............................................... No Yes 12. Were you following a low-cholesterol, low-fat diet? ................. No Yes 13. Were you participating in a cardiac rehabilitation program? .... No Yes 14. Many people do not take their medications perfectly. In the past 7 days, did you ever miss taking your medications? .......................... No Yes 15. Did any medical professional discuss with you the importance of taking your medications? ...................................................... No Yes 16. Were you taking aspirin on a daily basis during the 7 days before you came to the hospital? ................................................................ No Yes 17. Were you taking vitamins or supplements? ................................................ No Yes If yes, please list: ________________________________________________________________ ____________________________________________________________________________ Medical History (MHX) Page 2 of 11 ID #: Part 2 Instructions: Part 2 of this form is completed by chart abstraction. A. RISK FACTORS 18. Height: .................................... inches 19. Weight: .................................. lbs Note: For Questions 20 – 42, Unknown = No documentation of Positive or Negative History OR Unclear documentation. 20. Hypertension ........................................ No Yes Unknown (As documented by 1) diagnosis by a health care provider, or 2) SBP > 140 or DBP > 90 mmHg on at least 2 occasions, or 3) current use of antihypertensive medication) 21. Diabetes ............................................... No Yes Unknown (As documented by 1) diagnosis by a health care provider, or 2) current use of antidiabetic medication) 22. Dyslipidemia ......................................... No Yes Unknown (As documented by (1) diagnosis by a health care provider, or (2) current use of hypolipidemic medication) 23. History of cigarette smoking ................. No Yes Unknown If Yes, answer the following: a. Current (within 1 month) Recent (stopped 1 month to 1 year prior) Former (stopped > 1 year prior) b. Years of smoking: c. Cigarettes smoked per day: Cigarettes per day (1 = 1 or fewer per day) 24. Family history of coronary disease ....... No Yes Unknown (As documented by direct blood relatives – parents, siblings, children – who have had any of the following before age 55: 1) angina, or 2) myocardial infarction, or 3) sudden cardiac death without obvious cause) B. CARDIOVASCULAR DISEASE HISTORY 25. Angina ............................................................ No Yes Unknown (As documented by evidence or knowledge of symptoms before the index ACS event described as chest pain or pressure, jaw pain, arm pain, or other equivalent discomfort suggestive of cardiac ischemia) Medical History (MHX) Page 3 of 11 ID #: 26. Myocardial infarction....................................... No Yes Unknown (As documented by 1) physician diagnosis, or 2) hospitalization for MI) / 26a. If Yes, most recent date: Month / Day Year 27. Percutaneous Coronary Intervention (PCI) ..... / 27a. If Yes, most recent date: Month No / Month No Unknown Yes Unknown Yes Unknown / Day / Month Yes Year Year 29. Stroke ............................................................. 29a. If Yes, most recent date: Unknown / Day 28. Coronary Artery Bypass Surgery (CABG) ....... 28a. If Yes, most recent date: Yes No / Day 30. TIA ................................................................. Year No (As documented by focal neurological deficit, usually corresponding to the territory of a single vessel, that resolves spontaneously without evidence of residual symptoms at 24 hour) 31. Peripheral Arterial Disease ............................. No Yes Unknown (As documented by 1) claudication, either with exertion or at rest, 2) amputation for arterial vascular insufficiency, 3) vascular reconstruction, CABG, or PCI to the extremities, 4) aortic aneurysm, 5) positive noninvasive test (e.g., ankle brachial index < 0.8)) 32. Congestive heart failure .................................. a. If Yes, NYHA class: .. Medical History (MHX) I II III No Yes Unknown IV Page 4 of 11 ID #: C. OTHER COMORBID ILLNESS HISTORY 33. Chronic lung disease ............................ No Yes Unknown (As documented by 1) asthma, 2) chronic obstructive pulmonary disease, 3) chronic bronchitis, or 4) emphysema) 34. Kidney disease ..................................... No Yes Unknown 35. Liver disease ........................................ No Yes Unknown 35a. If Yes, severity: Mild (e.g. chronic hepatitis, or cirrhosis without complications such as varices, portal hypertension, encephalopathy, GI bleeding) Moderate/Severe (e.g. cirrhosis with complications such as varices, portal hypertension, encephalopathy, GI bleeding) 36. Rheumatologic disease ........................ No Yes Unknown (As documented by lupus (SLE), polymyagia rheumatica (PMR), polymyositis, mixed connective tissue disease, polymyalgia rheumatica, or rheumatoid arthritis (RA)) 37. Peptic ulcer disease ............................. No Yes Unknown (As documented by treatment for ulcer or history of GI bleed due to ulcer) Note: gastritis without ulcer does not count as peptic ulcer disease 38. AIDS ..................................................... No Yes Unknown No Yes Unknown No Yes Unknown Yes Unknown Note: not including those with asymptomatic HIV+ 39. Any cancer treated in the past 5 years.. (e.g., breast, lung, colon, prostate, brain, etc.) 40. Leukemia (blood cancer) ...................... (e.g., AML, CML, ALL, CLL, polycythemia vera) 41. Lymphoma (lymph node cancer) ......... No (e.g., Hodgkins, lymphosarcoma, Waldenstrom’s macroglobulinemia, myeloma, and other lymphomas) 42. Thyroid disease ................................... a. If Yes, type: ...................................... 43. Other co-morbid illness ......................... No Yes Hyperthyroidism No Unknown Hypothyroidism Yes a. _______________________________ b. _______________________________ c. _______________________________ Medical History (MHX) Page 5 of 11 ID #: D. INDEX ACUTE CORONARY SYNDROME (ACS) EVENT 27. Hospital Name: ________________________________________ / 28. Hospital admission date: / Month Day 29. Transferred from another hospital? ........ Year No Yes If Yes: a. Hospital Name: ________________________________________ / b. If Yes, transfer date: / Month Day / 30. Date of ACS diagnosis: / Month Day / 31. Hospital discharge date: Year Year / Month Day Year 32. Heart rate at initial hospital presentation: ................................. bpm 33. SBP/DBP at initial presentation:............................................... / 34. Killip class at initial presentation: .......... I 35. Cardiac arrest at initial presentation? No II III mmHg IV Yes 36. Heart rate at discharge: ........................................................... bpm 37. SBP/DBP at discharge: ............................................................ / mmHg E. ECG FINDINGS FOR INDEX ACS EVENT 38a. Admitting ECG available? No / a. Date of ECG: / Month Day Year : b. Time of ECG: Hour 38b. Pre-discharge ECG available? AM / PM Minute (circle one) No Yes / a. Date of ECG: Month / Day : b. Time of ECG: Hour Medical History (MHX) Yes Year AM / PM Minute (circle one) Page 6 of 11 ID #: 39. ECG changes? .................... No Yes (If Yes, retain copy of ECG on which diagnosis is made, and a subsequent ECG after “evolution” of the changes) a. For the diagnostic ECG, indicate type(s) of ECG changes (check all that apply): ST-segment elevation 0.1 mV elevation in 2 or more contiguous leads Q waves greater 0.04 seconds in width and 0.1 mV in depth in at least 2 contiguous leads ST-segment depression > 0.05 mV in 2 more contiguous leads (includes reciprocal changes) T-wave inversion of at least 0.1 mV b. For the ECG after evolution of the changes, indicate the pattern: ..... 40. Paced rhythm? ................... No Yes 41. Atrial fibrillation or flutter? ... No Yes 42. Bundle branch block? ......... No Yes a. Type ............................... RBBB LBBB b. Timing ............................ New Old Q wave non-Q wave Unknown F. LABORATORY TESTS DURING HOSPITALIZATION FOR INDEX ACS EVENT 43. Troponin I or T performed? ............ a. Instrument: ............... No Yes cTnI (cardiac troponin I) cTnT (cardiac troponin T) Other, specify: ________________ b. Assay: ..................... Abbott AxSYM ADV Radiometer AQT90 Abbott Architect Response RAMP Abbott i-STAT Roche E170 Beckman Access Accu Roche Elecsys 2010 Beckman Access hs-cTnI Siemens Centaur Ultra bioMerieux Vidas Ultra Siemens Dimension RxL Innotrac Aio! Siemens Immulite 2500 Inverness Biosite Triage Siemens Stratus CS Mitsubishi PATHFAST Siemens VISTA Nanosphere hs-cTnI Singulex hs-cTnI Ortho Vitros ECi ES Tosoh AIA II Other, specify: _____________________ Medical History (MHX) Page 7 of 11 ID #: c. Troponin at initial hospital presentation: .............................. ng/mL d. Troponin during hospitalization: .......................................... ng/mL (peak - prior to PCI or CABG if done) ‘INITIAL’ IS DEFINED AS THE FIRST VALUE RECORDED DURING THE INDEX ACS HOSPITALIZATION 44. Initial creatinine........................................................................ mg/dL 45. Initial total cholesterol: ............................................................. mg/dL 46. Initial triglycerides: ................................................................... mg/dL 47. Initial LDL: ............................................................................... mg/dL 48. Initial HDL: ............................................................................... mg/dL 49. Initial hemoglobin A1c: ............................................................. % G. PROCEDURES DURING HOSPITALIZATION FOR INDEX ACS EVENT 50. Stress test? ........................ No Yes If Yes, then answer the following: / a. Date of test: Month b. Stress test type ............... / Day Exercise If Exercise, to target heart rate? ................ Year Pharmacological No Yes c. Imaging type: .................. EKG only Nuclear PET d. Ischemia Result .............. Positive Negative Equivocal Present Absent e. Fixed defect indicating an old MI .................. Echocardiogram f. Other findings (e.g, hypotension, delayed hysteresis): __________________________ Medical History (MHX) Page 8 of 11 ID #: 51. LV function assessed during hospitalization? No Yes If Yes, then answer the following: a. Initial LVEF: % or check one b. Mitral regurgitation noted? .......... Normal/Low normal Mildly reduced Mild-moderately reduced Moderately reduced Moderate-severely reduced Severely Reduced No Yes c. EF method: (check one) Echocardiography (by ultrasound) Contract ventriculography (by cath/angiogram) Radionuclide ventriculography or SPECT on stress testing (nuclear) 52. Diagnostic cardiac catheterization? No Yes If Yes, then answer the following: / a. Date: Month / Day Year b. Maximum stenosis (%): LAD LCx RCx LM 53. PCI performed? ............................... No Yes If Yes, then answer the following: / a. Date: Month / Day Year b. Stents placed: c. Stent type: ......................... Bare metal d. Complications of PCI? ................ If Yes, type (check all that apply): Medical History (MHX) No Drug-eluting Yes Bleeding Vascular complication Cardiac tamponade Arrhythmia Stroke Contrast reaction Acute renal failure Page 9 of 11 ID #: 54. Coronary Artery Bypass Surgery performed? / a. Date: Month Medical History (MHX) No Yes / Day Year Page 10 of 11 ID #: H. CURRENT MEDICATIONS No Yes Unknown Name Daily Dose Units 55. ACE inhibitors ............................... ______________ _________ 56. Angiotensin II receptor blockers . ______________ _________ 57. Aspirin ............................................ ______________ _________ 58. Clopidogrel .................................... ______________ _________ 59. Other antiplatelet agents ............. ______________ _________ 60. Anticoagulants (e.g., Warfarin) ....... ______________ _________ 61. Beta-blockers ................................ ______________ _________ 62. Calcium channel blockers ........... ______________ _________ 63. Digitalis/Digoxin ............................ ______________ _________ 64. Other inotropic agent (not digitalis) ______________ _________ 65. Diuretics ......................................... ______________ _________ 66. Statin lipid-lowering agents ......... ______________ _________ 67. Non-statin lipid-lowering agents . ______________ _________ 68. Nitrates ........................................... ______________ _________ 69. Vasodilators (not ACE inhibitors) ..... ______________ _________ 70. PO hypoglycemic antidiabetic .... ______________ _________ 71. Insulin ........................................... ______________ _________ 72. Antiarrhythmics ............................. ______________ _________ 73. Female hormone replacement therapy .................... ______________ _________ 74. Thyroid replacement therapy ...... ______________ _________ 75. Antipsychotics ............................... ______________ _________ 76. Other drug class ........................... ______________ _________ 77. Other drug class ........................... ______________ _________ 78. Other drug class ........................... ______________ _________ 79. Other drug class ........................... ______________ _________ 80. Other drug class ........................... ______________ _________ 81. Other drug class ........................... ______________ _________ Medical History (MHX) Page 11 of 11