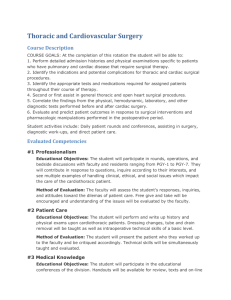
avstsautumn09manuscript
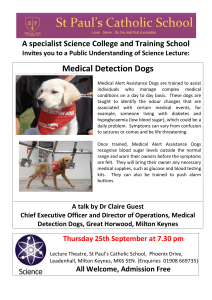
advertisement

Page |1 AVSTS meeting October 2009 Program and Contents Page Friday October 16th 2009 9:30 to 10:00 Registration 10:00 to 10:45 Lecture– Surgical management of pyothorax– M Radlinsky 3 10:45 to 11:15 Lecture– Medical management of pyothorax– K Murphy 6 11:15 to 11:45 Coffee 11:45 to 12:45 Lecture – Non-cardiac thoracic surgery in people – T Batchelor 12:45 to 13:00 Panel discussion on Pyothorax – Radlinksy/ Batchelor /Murphy 13:00 to 13:10 Case report: Thoracoscopic pericardectomy in a cat P Nelissen 13:15 to 13:30 Presentation by Duncan Henderson of Freelance Surgical 13:30 to 14:30 Lunch 14:30 to 15:15 Lecture – Chylothorax - M Radlinsky 11 15:15 to 15:30 Panel discussion - Chylothorax – Radlinsky/Brockman 15:30 to 16:00 Coffee 16:00 to 17:00 Lecture – Reconstruction of the thoracic wall - DJ Krahwinkel 14 Saturday October 17th 2009 09:00 to 10:00 Lecture – Tracheal collapse – stent or rings? - DJ Krahwinkel 17 10:00 to 10:45 Lecture – Thoracoscopy: overview and technique tips – M Radlinsky 20 10:45 to 11:00 Coffee 11:00 to 11:30 Lecture – Thoracoscopy for bullous emphysema – H Brissot 23 11:30 to 11:45 Panel discussion - Thoracoscopy – Radlinksy/Brissot 11:45 to 12:30 Lecture – Open versus thoracoscopic pericardectomy - H Brissot 25 12:30 to 13:30 Lunch 14:00 to 15: 00 Lecture – Surgical management of Thymomas - D Brockman 27 15:00 to 15:30 Coffee 15:30 to 16:30 Lecture – Laryngeal paralysis and associated polyneuropathy- DJ Krahwinkel 33 AVSTS meeting October 2009 Non-cardiac thoracic surgery Page |2 Invited Speakers Dr Mary Anne Radlinsky DVM MS DipACVS Diplomate of the American College of Veterinary Surgeons Associate Professor in Small Animal Surgery University of Georgia Athens Georgia USA Ms Kate Murphy BVSc (Hons) DSAM DipECVIM-CA MRCVS PG Cert (HE) European Veterinary Specialist in Internal Medicine Medicine Team Leader Senior Clinical Fellow in Small Animal Emergency Medicine and Intensive Care Division of Companion Animals University of Bristol Langford Mr Tim Bachelor FRCS(CTh) Consultant in General Thoracic Surgery Bristol Royal Infirmary Bristol Professor DJ Krahwinkel DVM, MS, DipACVS, DipACVA, DipACVECC Diplomate of the American College of Veterinary Surgeons Diplomate of the American College of Veterinary Anesthesiologists Diplomate of the American College of Veterinary Emergency & Critical Care Professor of Surgery The University of Tennessee Knoxville Tennessee USA Dr Herve Brissot DMV, DipECVS, MRCVS. European Specialist in Small Animal Surgery DAVIES Veterinary Specialists Higham Gobion Hertfordshire. Professor Dan Brockman BVSc CertVR CertSAO DipACVS DipECVS European and American Specialist in Small Animal Surgery Head of Veterinary Clinical Sciences The Royal Veterinary College Hertfordshire AVSTS meeting October 2009 Non-cardiac thoracic surgery Page |3 SURGICAL TREATMENT OF PYOTHORAX MaryAnn Radlinsky, DVM, MS, DACVS University of Georgia, Athens, GA, USA Pyothorax in dogs and cats may not be the same disease. It has long been presumed that the condition in dogs is related to migration of plant material, trauma, or hematogenous spread. The occurrence of disease in hunting breeds associated with the hunting season has led to the theory that plant material is aspirated and slowly migrates into the pleural space due to the negative pressure generated during ventilation. Unfortunately, plant material is rarely identified in cases undergoing surgery and cannot be identified in medically managed patients. The condition in cats has been related to young age, perhaps the male condition, and oropharyngeal flora. The same study showed an increased occurrence in cats with outdoor exposure and multicat households and concluded that bite wounds may have been the source of infection. Other researchers have concluded that a lack of sex and breed predisposition and oropharyngeal flora with adjacent involvement of intrathoracic structures made parapneumonic spread the likely cause of pyothorax in cats. They postulated that aspiration of oropharyngeal flora and colonization of the lower respiratory tract was likely. It has long been known that the respiratory tract is occasionally contaminated with oropharyngeal flora, and concurrent conditions such as viral upper respiratory tract infection may increase the risk of the development of pyothorax. This would agree with the earlier reports of outdoor cats and multicat households, which would likely have an increased exposure to many viral agents. Identification of the underlying cause is at times quite elusive. The percentage can range from 4 to 78% having a known etiology. Cats and dogs developing pyothorax tend to be young, with medium to large breeds of dog more commonly affected. The disease is thought to be slowly progressive and chronic by the time it is diagnosed. Most cases are bilaterally affected (only 11-24% were reported with unilateral effusion), with inappetance, lethargy, and dyspnea being common historical and physical examination findings. The CBC is consistent with significant infection, and the biochemical profile often is consistent with dehydration and secondary effects of significant inflammation (SIRS). Both aerobic and anaerobic cultures should be made of the fluid, and cytological examination is important to differentiate contaminants from infectious organisms. Polymicrobial infection is common in most studies and ranges from 24% to 78% of the cases having multiple organisms identified. Plenty of fluid should be made available for culture and susceptibility testing, anaerobic culture, gram staining, fungal culture, and PCR and DNA sequencing. The diagnostic plan for cases of pyothorax also includes thoracic imaging. Radiographs made after thoracocentesis are helpful in identification of pulmonary or mediastinal lesions. Ultrasound may also be helpful for examining the mediastinum and pericardium and pericardial sac for lesions. The use of CT and MRI has yet to be elucidated in cases of pyothorax. Identification of lesions in thoracic structures (esophagus, mediastinum, pulmonary parenchyma, etc) is important in the therapeutic plan for a patient. Identification of lesions associated with these structures prompts surgical intervention in most practices. Removal of the source of bacteria is important in the treatment of any abscess, and pyothorax is simply the accumulation of exudate within the pleural space. The rest of medical therapy is similar to the treatment of any abscess: stabilization of the patient, appropriate antimicrobial therapy, and drainage and lavage. Most published studies include each of these procedures for the treatment of pyothorax. An early study did not recommend thoracostomy tube placement, however, chest tubes are widely recommended for appropriate drainage and lavage of the pleural space. Chest tubes were more commonly placed in survivors in one study, were recommended in another for the treatment of feline pyothorax. Chest tubes are commonly used to treat canine pyothorax as well. Outcome with chest tube AVSTS meeting October 2009 Non-cardiac thoracic surgery Page |4 placement, pleural drainage and lavage, stabilization therapy as necessary, and antibiotic therapy based on culture and susceptibility testing has been associated with good outcomes in dogs and cats, ranging from 66 – 95% success, with the highest success in cats. Cats treated with chest tubes were more likely to survive than those without and the tubes decrease the risk associated with repeated thoracocentesis and result in better drainage of the pleural space. Whether one-time drainage alone with antimicrobial therapy will be as successful likely requires a larger study. This option may be appropriate for cases in which financial constraints limit diagnostic and therapeutic abilities of the client. Surgery is usually recommended in cases that have intrathoracic pathology on diagnostic evaluation, but the decision to perform surgery in other cases is not well defined. Failure to respond to medical management is a nebulous entity for recommending surgical intervention. Medical therapy must be adequate, with adequate being in the eye of the beholder. Ideally, medical management involves a complete diagnostic workup, fluid analysis to include cytology, gram stain, aerobic, fungal, and anaerobic culture, and culture aimed at Actinomyces and Nocardia spp. The presence of Actinomyces in the effusate was associated with a poorer outcome with medical management in one study, thus the presence of Actinomyces in culture or gram stain prompts some clinicians to immediate surgery. The decision to change from medical management also may be time dependent. How many days of medical therapy are enough to say that a case has failed medical management? Most use a minimum of 3 days of appropriate therapy and base the decision on daily cytological evaluation of the effusate, physical examination, or CBC results. Surgery has been associated with a better outcome in both cats and dogs with pyothorax in 2 studies. The most recent study in dogs suggested that medical management was 5 x more likely to fail (result in recurrence, progression of disease, or death) compared to surgical treatment. That study also reported the significantly decreased disease free interval of dogs with Actinomyces identified and treated medically. Complications of therapy should be considered when choosing a route of treatment. Complications of surgery include DIC, abdominal effusion, death, and complications of the procedure done (pneumolobectomy, etc). Complications of medical management that includes thoracostomy tube placement have included incomplete removal of fluid from the pleural space, poor tube placement, leakage of fluid and adjacent cellulitis, pneumothorax, and hemorrhage requiring transfusion associated with chest tube placement. Prolonged management of thoracostomy tubes may also result in granulation of the tract surrounding the tube and subsequent leakage of fluid or air from or into the pleural space, respectively. Each form of treatment should be discussed with the owner and the decision based on the literature and client education. Surgery has been associated with an improved outcome in cases of canine and feline pyothorax and should be considered in every patient. Unfortunately, medical management in an intensive care unit for at least 3 days is costly, so complete diagnostic evaluation for thoracic pathology is imperative. Thoracoscopy has been considered in human medicine as a diagnostic and therapeutic tool for decision making in cases of pyothorax. Early thoracoscopy may allow evaluation of the pleural space for significant adhesions and pathology that would prompt earlier surgical intervention (instead of monitoring the progression with medical management alone for a period of days). Thoracoscopy in veterinary medicine has been used mainly in the treatment of pyothorax. Once the decision for surgical intervention is made, thoracoscopy may be performed to debride the mediastinum, with the pericardium if necessary. The patient is placed in dorsal recumbency, and a paraxiphoid port is placed. The endoscope is introduced into the chest to evaluate the extent and severity of disease. If significant pleural thickening and loculation by adhesions is present, median sternotomy is opted for. Severely thickened mediastinum may require a significant intercostal thoracotomy for retrieval if morcellating devices are not available, and AVSTS meeting October 2009 Non-cardiac thoracic surgery Page |5 they are often not available yet in veterinary practices. Moderate pleural thickening in the absence of multiple adhesions may be amenable to thoracoscopic mediastinal debridement. Two to three more ports are placed in the ventral intercostal spaces, located ventral to the pulmonary excursions, for introduction of grasping and cutting tools. The entire ventral mediastinum with or without the pericardium is debrided from the thoracic inlet to the diaphragm and pleural recesses. Thoracoscopy provides phenomenal illumination and magnification for debridement. Thoracoscopy can be used to guide placement of thoracostomy tubes and is associated with significantly less pain and morbidity than thoracotomy. Care must be taken to remove all pleural fluid prior to commencement of debridement, as the lungs will “float” ventrally and interfere with visualization and increase the risk of parenchymal trauma and pneumothorax. Partial pneumolobectomy and complete pneumolobectomy have also been done in dogs via thoracoscopy. Cats require small instrumentation and probably more practice due to space limitations. Specialized equipment greatly increases efficiency during thoracoscopic or open surgical debridement of the mediastinum. Monopolar and bipolar cautery are rapidly becoming antiquated with the advent of stapling devices, which are soon to be obsolete in the face of vessel sealing devices. These devices apply bipolar cautery to tissue, sense the resistance present, and seal vessels closed. They do not require or cause large amounts of coagulation and are associated with decreased lateral spread of tissue damage. They have become so specialized as to obviate the need for dissection of fat from the structures being sealed, signaling the surgeon that the seal is complete, and include a cutting blade for immediate transaction of tissue without the need for an instrument change. There are limitations to the vessel size that can be sealed and transected, but most mediastinal vessels are amenable to their use. Thoracoscopy and vessel sealing devices may make surgical intervention for pyothorax less invasive and may be associated with shortened hospital stay in cases of pyothorax. The use of specialized equipment and duration of time in the surgery suite have not been associated with a decrease in financial output by the client, however. Pyothorax is an accumulation of exudate within the pleural space, requires significant diagnostic testing, and most cases respond more favorably to surgical intervention. Care should be taken when considering which bacteria are present, intrathoracic lesions, and potential outcome associated with each case. Thoracoscopy may increase our ability to debride the chest with decreased morbidity and hospital stay, thereby decreasing the time associated with medical management of pyothorax to that required for stabilization. AVSTS meeting October 2009 Non-cardiac thoracic surgery Page |6 MEDICAL MANAGEMENT OF PYOTHORAX IN DOGS AND CATS Kate Murphy BVSc(Hons) DSAM DipECVIM-CA MRCVS PGCert(HE) Senior Clinical Fellow in Small Animal Emergency Medicine and Intensive Care University of Bristol Pyothorax describes infection of the pleural space. Infection may result from haematogenous or lymphatic spread, extension from an adjacent structure (bronchopneumonia, parapneumonic spread, oesophageal perforation, mediastinitis) or direct introduction (thoracic trauma, penetrating bite, foreign body, thoracocentesis/surgery). In many cases both in cats and dogs, the exact aetiology is not identified. In cats, the incidence is higher in multi-cat households and antecedent upper respiratory tract infection has been recognised as a predisposing event. Pyothorax can have an insidious onset and is more common in young adult, male cats and adult large breed dogs. Reports of pyothorax in neonates exist. Clinical signs relate to pleural effusion, decreased lung expandability and impaired gas exchange and include: Tachypnoea Dyspnoea Orthopnoea Exercise intolerance Lethargy Anorexia Pyrexia Reluctance to lie down Cough Physical examination may reveal Poor body condition Tachypnoea/Dyspnoea/Orthopnoea Muffled heart sounds Decreased lung sounds Hyporesonant/dull thoracic percussion particularly ventrally May be evidence of sepsis The diagnosis of pyothorax is made using a combination of history, physical findings, minimum database (evidence of inflammation, hypoalbuminaemia, possibly electrolyte derangements), diagnostic imaging (radiography and ultrasonography) and most importantly fluid analysis (cytology, proteins, culture). Assessment of haemostasis should also be included as these patients are at risk of DIC. Pyothorax is often a polymicrobial infection. Isolates from dogs and cats include 1: AVSTS meeting October 2009 Non-cardiac thoracic surgery Page |7 Aerobic Pasteurella spp (common in both dogs and cats, most common isolate in cats) Escherichia coli (dog) Proteus spp (dog) Streptococcus spp (dog) Staphylococcus intermedius (dog) Actinomyces spp (dog) Nocardia spp (dog > cat) Anaerobic Bacteroides spp (dog and cat) Peptostreptococcus anaerobius (dog) Fusobacterium spp (dog) Clostridium spp (dog) Unidentified gram negative rods (cat) Barrs et al 2recently reported pyothorax in cats associated with some unusual organisms including Mycoplasma spp, Salmonella typhimurium, and Cryptococcus gattii. Extension of infection from an adjacent intrathoracic structure was considered the most likely mechanism of infection in that study. There are a number of different aspects to management of pyothorax including: Supportive care o Fluid therapy o Oxygenation o Nutrition o Good nursing care Appropriate antibiotic therapy Drainage of the effusion Thoracic lavage Surgery? Analgesia Monitoring o Clinical parameters o Progress Supportive care The fluid requirements of these patients can be underestimated, particularly in the speaker’s experience in patients with “dry” pyothorax. Once the patient’s hydration and volume abnormalities are addressed we sometimes find that the chest becomes more effusive. Oxygen supplementation should be considered if the patient is showing signs of respiratory distress. Arterial blood gas analysis or pulse oximetry can be used to provide baseline data and to follow response to oxygen supplementation. Nutritional status should be assessed since often these patients’s present quite cachectic likely due to a combination of poor intake coupled with high protein exudates. Consider appetite stimulation and if not effective the use of tube feeding. Appropriate antibiotic therapy AVSTS meeting October 2009 Non-cardiac thoracic surgery Page |8 This should be based upon culture and sensitivity. Initial guidance is achieved by cytological evaluation of the effusion (gram positive vs gram negative organisms). It is important to remember that pyothorax is a polymicrobial infection. Antibiotics are given intravenously initially to ensure adequate therapeutic levels are achieved rapidly. This dictates to a certain extent the antibiotics which are selected. An appropriate antibiotic would be amoxicillin (potentiated can be used) which provides good gram positive and negative aerobic cover and good anaerobic cover. In addition metronidazole could be considered to extend the anaerobic spectrum. If gram- negative organisms are cultured which are resistant to penicillins then fluroquinolone might be considered based upon the sensitivity data. Protracted oral antibiotics are indicated once the patient is stable and we usually recommend at least 6-8 weeks with radiographic +/- ultrasonographic re-evaluation during and after cessation of treatment. Drainage of the effusion & lavage This is one of the more controversial aspects of medical management of pyothorax. Drainage can be achieved by either: Needle thoracocentesis Chest drain placement Either technique can be used for single drainage or for repeated drainage. If lavage is to be performed this is usually performed using an indwelling chest drain. The literature contains some recent studies describing successful treatment of canine pyothorax with single drainage using a chest drain3 and also the use of small bore chest drains placed via a modified seldinger technique 4 for a variety of pleural space diseases. A previous study using small bore drains (home made seldinger kit) for pleural space drainage 5 reported treatment of pyothorax in 10 cases with a mean drain dwell duration of 8.5 days (3-18 days), however there is no mention as to whether lavage was also used. In my institution we see a wide spectrum of cases with pyothorax from the recently diagnosed healthy patient to the chronic patient with severe accumulation of inflammatory tissue to the SIRS patients. Currently my practice is to assess the patient and use certain features to guide management. 1. Cats with mild-moderate effusion – can be managed with intermittent thoracocentesis using butterfly needle. Sometimes only require single drainage. 2. Cats with more effusive disease, a chest drain is placed and intermittent drainage performed. Lavage is considered if the chest is not draining effectively with intermittent suction alone. Recommend consideration of seldinger chest drains. 3. In dogs with mild-moderate effusion – thoracocentesis attempted but often unsuccessful in achieving effective drainage (usually obtain diagnostic samples) unless a chest drain is placed – small or large bore chest drain can be considered. Drain is usually left in situ to assess how effusive the patient will remain. If little fluid is produced and the patient is well hydrated, chest drain is removed. If producing significant effusion then the drain remains in situ until the volume of fluid production approaches 2ml/kg/day. 4. In dogs with chest drain placed, thoracic lavage is performed at least twice daily until the fluid retrieved has become less flocculent. Warmed normal saline or Hartmann’s is used at 1020ml/kg. 5. If a chest drain was placed and little fluid was obtained even at time of placement and despite rehydration the volume of effusion remains small, then the chest drain is removed and the patient managed as per Johnson & Martin3. 6. Usually unilateral drain placed in most cases, however if severe bilateral effusion is present which does not drain effectively via unilateral drain, then second drain is placed. The decision to place the second drain is based on the patient’s respiratory pattern, rate and oxygenation status not simply on the presence of fluid. AVSTS meeting October 2009 Non-cardiac thoracic surgery Page |9 7. Continuous suction is not used routinely. If the patient also has pneumothorax, it would be considered. It is not uncommon for the respiratory signs to persist despite effective drainage of the fluid and this often reflects reduced lung expandability or persistent of lung consolidation/collapse. If this lung changes do not improve further investigation should be considered. Surgery Surgery is reserved for patients with poor response to medical management (ideally having received aggressive management for 3-5 days) or who have a structural lesion which requires exploring e.g. possible abscess or lung mass, pneumothorax which is not reducing. We have a number of cases that present with very solid material in the mediastinum some of these have been surgically managed but others have resolved with protracted antibiotics and short term intravenous fluids and thoracic drainage. Therefore we do not view the presence of solid tissue as an indication for surgery. Analgesia As always, analgesia is very important and combination of local and systemic analgesia should be considered and adjusted according to patient assessment. Monitoring Progress can be monitored clinically based upon physical examination and cardiovascular parameters but also by cytological examination. One would expect the fluid cell count to decrease, the neutrophil degeneration to reduce and that bacteria should not be evident. Additionally radiographs might be used to evaluate tube problems e.g. kinking, odd position or stopped working (e.g. tube in situ but fluid in thorax increasing). Thoracic ultrasound can also be valuable to quickly assess the extent of fluid accumulation. References: 1. Demetriou JL, Foale RD, Ladlow J, McGrotty Y, Faulkner J and Kirby BM. Canine and feline pyothorax: a retrospective study of 50 cases in the UK and Ireland. Journal of Small Animal Practice, 2002, 43, 388-394 2. Barrs VR, Allan GS, Martin P, Beatty JA, Malik R. Feline pyothorax: a retrospective study of 27 cases in Australia. Journal of Feline Medicine and Surgery, 2005, 7, 211-222 3. Johnson MS, Martin MWS. Successful medical treatment of 15 dogs with pyothorax. Journal of Small Animal Practice 2007, 48, 12-16 4. Valtolina C, Adamantos S. Evaluation of small-bore wire-guided chest drains for management of pleural space disease. Journal of Small Animal Practice, 2009, 50, 290-297 5. Frendin J, Obel N. Catheter drainage of pleural fluid collections and pneumothorax. Journal of Small Animal Practice, 1997, 38, 237-242 Additional references/further reading: AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 10 1. Barrs VR, Beatty JA. Feline pyothorax – New insights into an old problem. Part 1. Aetiopathogenesis and diagnostic investigation. The Veterinary Journal, 2009, 179, 163-170 2. Barrs VR, Beatty JA. Feline pyothorax – New insights into an old problem. Part 2. Treatment recommendations and prophylaxis. The Veterinary Journal, 2009, 179, 171-178 3. King LG Textbook of Respiratory disease in dogs and cats. WB Saunders. 4. Rooney MB, Monnet E. Medical and surgical treatment of pyothorax in dogs: 26 cases (19912001) Journal of American Veterinary Medical Association, 2002 221, 86-92 5. Waddell LS, Brady CA, Drobatz KJ. Risk factors, prognostic indicators, and outcome of pyothorax in cats: 80 cases (1986-1999). Journal of American Veterinary Medical Association, 2002, 221, 819-24 6. Walker AL, Jang SS, Hirsh DC. Bacteria associated with pyothorax of dogs and cats: 98 cases (1989-1998). Journal of American Veterinary Medical Association. 2000, 216, 359-63 7. Scott JA, Macintire DK. Canine Pyothorax: Pleural Anatomy and Pathophysiology. Compendium on Continuing education for the practicing veterinarian, 2003, 25, 172-179 8. Scott JA, Macintire DK. Canine Pyothorax: Clinical Presentation, Diagnosis, and Treatment. Compendium on Continuing education for the practicing veterinarian, 2003, 25, 180-194 AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 11 CHYLOTHORAX MaryAnn Radlinsky, DVM, MS, DACVS University of Georgia, Athens, GA, USA Chylothorax is a very difficult condition to cure. It is important to rule out the many primary causes of chylous effusion, but the condition is usually idiopathic. This makes the financial input high even prior to considering surgical intervention. The typical diagnostic plan includes: CBC, biochemical profile, heartworm test, urinalysis, thoracic radiographs, thoracic ultrasound, cardiac ultrasound, abdominal radiographs, abdominal ultrasound, pleural fluid analysis, fluid triglyceride and cholesterol levels, serum triglyceride and cholesterol levels, and fluid culture. Some clinicians recommend cultures for L form bacteria as well as aerobic and anaerobic cultures. In cases of more chronic and previously treated chylothorax, we make sure to obtain fluid culture, as the risk of infection secondary to thoracocentesis has been associated with infection on some of our clinical cases. Treatment of the primary cause is important and the prognosis can depend on the primary process, if present. We have operated some cases of restrictive pericarditis with concurrent chylothorax. In those few cases we have seen a change in the central venous pressure or right atrial pressure following pericardectomy. The vast majority of idiopathic chylothorax cases seem to have lymphangiectasia of the cranial thorax, and the true etiology of the condition may be multifactorial and different in each case. Until we better understand the pathophysiology of the condition, we are left with symptomatic therapy. The goal of surgery is to eliminate the accumulation of chyle within the pleural space. Many surgical options exist, providing further evidence that we do not understand the pathophysiology and that we have not identified the ideal treatment. Surgery seems to be aimed at: 1) causing the formation of new lymphaticovenous anastomoses, 2) redirecting the absorption of chyle, 3) aid in the passage of fluid across the lymphaticovenous junction. Thoracic duct ligation (TDL) causes new lymphaticovenous anastomoses to form, pericardectomy may aid in the flow of lymph across the lymphaticovenous junction, and omentalization may redirect the absorption of chyle. Currently described techniques include TDL and concurrent pericardectomy, TDL with concurrent cistern chyli ablation, and thoracic omentalization. There are many variations on a theme for achieving complete ligation, which is necessary if a cure is even to be hoped for. The thoracic duct anatomy seems to be minimal in the caudal thorax, so a caudal approach is desired. Open and thoracoscopic approaches have been described. Concurrent pericardectomy has been advocated. Pericardectomy was used as the sole form of therapy in a cat and pericardectomy was used in cases of failed TDL. TDL and pericardectomy resulted in up to 90% success, but failed in 2 cats in the published report. The increased success was attributed to surgeon skill, improved right-sided pressures, and improved technique for TDL. The improved technique was attributed to intense, local illumination and magnification via ocular loupes. Thoracoscopy offers even greater illumination and magnification, so a technique for TDL was developed. Thoracoscopy may also allow a further caudal dissection and ligation, where the fewest duct branches are usually present. The dissection is typically caudal to the entry of the azygous vein, avoiding dissection of that structure. Clips or ligation may be done, the author currently does both, clips are useful in identifying the site of ligation on radiographs, which may be as far caudal as in the lumbar region and may be unseen on typical thoracic radiographs. Care must be taken if the cisterna chyli is seen coming through the diaphragm, as it is large, thin-walled, and fragile! Thoracoscopy is also the standard of care in many practices for pericardectomy, and can be done concurrently via a lateral or ventral approach. The author prefers a ventral approach and collects pericardium for histopathology and culture. A pericardial window is made, and 3 incisions are made in the pericardium in a ventral to dorsal direction, taking care to avoid the phrenic nerves. This adequately frees the pericardium and decreases the risk of adhesion to the epicardium. Trochars are located according to each patient’s anatomy in the caudo-lateral thorax on the right for the initial exploration and TDL. The author places the endoscope in the mid- thorax in the 10th intercostal space, then places subsequent instrument ports so that dissection is achieved perpendicular to the longitudinal axis from right to left. Incise the mediastinum longitudinally along the VENTRAL aspect of the aorta, then free the mediastinum and thoracic duct branches from the lateral and dorsal surfaces of the aorta. Upon reaching the dorsal aorta, retract it ventrally with a curved dissector until the left hemothorax is entered. The author has added 2 ports in the left hemothorax so that a second, 0 degree AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 12 endoscope can be used to ensure that the dissection includes all visible branches of the thoracic duct on the left side. The dorsal mediastinum is similarly incised longitudinally, ventral to the sympathetic trunk and should progress into the left hemothorax as well. Since many of the affected patients are large, suture may be used to ligate the branches en masse. Clips are also applied. The 2 ports in the left hemothorax can be used to pass the suture around the thoracic ducts, and an extracorporeally tied knot is slid down into the chest from the right side. Clips may be applied from the left and right to further ensure (hope) that all branches are completely ligated. The tips of the clips are manipulated to encompass all mediastinum and branches and are guided by the endoscopist viewing from the contralateral side. Dissection and ligation of individual branch may be done, or ligation can be attempted in an en bloc fashion. The ability to visualize the thoracic duct branches may be hindered by the clarity of the lymphatic fluid and thickness of the mediastinal pleura. The lymph may be turned opaque by feeding oil or whipping cream prior to surgery, but the author does reliably obtain opacity, even when multiple doses are used before surgery. Some clinicians believe in performing lymphangiography prior to and after TDL. Access to the lymphatics can be through a central or peripheral approach. Mesenteric lymphatic catheterization has long been the standard of care when performing lymphangiography. Open techniques for treating chylothorax could then require 3 different approaches: 2 thoracotomies (1 for TDL, 1 for pericardectomy) and an abdominal approach for lymphatic catheterization. Catheterization of a mesenteric lymphatic is beneficial, in that allows for lymphangiography to be done and allows intra-operative coloration of the thoracic duct branches with methylene blue. Different techniques have been developed to avoid mesenteric lymphatic catheterization, which is often difficult, especially in small patients. Laparoscopic mesenteric lymph node injection has been described. It was successful in 6/10 experimental dogs, but problems existed with poor flow, leakage, and lack of the ability to properly stabilize the lymph node for injection. The author has not attempted mesenteric injection via laparoscopy and has investigated peripheral lymph node injection instead, to decrease access to multiple body cavities. Coloration of the popliteal lymph node was possible with a mini-approach to the node and injection of 0.5 ml of dilute methylene blue. Please note that methylene blue will still color the thoracic duct when greatly diluted. The research study for development of the thoracoscopic technique used 0.8 cc of methylene blue in 100 cc of sterile saline. (Full strength methylene blue is not necessary; however, the author has no proof that this decreases complications that may be associated with its use). One time injection of the popliteal lymph node resulted in coloration of 6/10 dogs’ thoracic ducts. When the contralateral popliteal lymph node was then injected, 3 more were colored blue. The final dog also failed coloration when the mesenteric lymph node was injected. Personal preference likely dictates the timing of coloration. The single injection of methylene blue resulted in coloration for 60 minutes in the experimental dogs in one study. Some clinicians mix the methylene blue with contrast to perform lymphangiography prior to dissection and re-evaluate with lymphangiography and visualization after TDL. Iohexol injection of the popliteal lymph node has also been described in the dog as a method of lymphangiography. One apparent benefit of lymphatic catheterization would be the ability to not only inject the lymphatic system, but to also inject under some pressure. It has been theorized that some thoracic duct branches remain patent yet invisible despite lymphangiography and coloration. Pressurization of the lymphatics is the only way that the author postulates will avoid this complication. The use of a butterfly catheter in the popliteal lymph node has increased the volume of dye injected and has led to obvious distention of the thoracic duct following TDL. The popliteal lymph node must be approached enough to allow stabilization and placement of the butterfly catheter. SLOW injection of methylene blue (we currently use 0.5 -1.0 ml in 60 ml saline) allows coloration and distention of the lymphatic system. Up to 10-20 ml may be injected; the dose is decided upon observing distention and /or coloration of the thoracic ducts in the thorax and whether coloration is seen beyond the site of TDL. The maximum dose of stock solution methylene blue using this system is 0.15-0.33 ml. Iohexol injection of the popliteal lymph node has been described in the dog as a method of lymphangiography. En bloc ligation of the tissues dorsal to the aorta can be done without any pre-operative feeding of fatty meals and mesenteric or lymph node injection or dye or contrast. Unfortunately, it is not perfect either. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 13 One study reported successful TDL in 13/14 dogs in which contrast lymphangiography was done. The single failure was due to a branch of the thoracic duct located on the right side of the aorta. This further emphasizes the need to start the dissection ventral and lateral on the aorta. The author strongly recommends that the same dissection occur on the left side of the aorta, as many branches were noted on the left in the study evaluating popliteal lymph node injection for coloration of the thoracic duct and because failures of thoracoscopic TDL were due to left-sided branches in another study. Cisterna chyli ablation was developed to increase the success rate of TDL. It was hypothesized that continued chylous effusion or modified transudative effusion was due to collateral lymphatic channel opening in response to increased pressure following TDL. It was also hypothesized that new lymphaticovenous anastomoses may form in the abdomen, rather than chest at the site of the ablation. TDL alone resulted in new anastomoses adjacent to the ligation site, whereas TDL + CCA resulted in intra-abdominal anastomoses. Clinical application of TDL + CCA resulted in long-term resolution of clinical signs in 7/8 cases reported, with 1 having no improvement and one case died acutely 2 months after the procedure, no necropsy was performed in that case. CCA may be useful in treating TDL failures; however, its sole use in the treatment of chylothorax is under investigation. Omentalization is somewhat out of favor currently. Two case reports (1 canine, 1 feline) elucidated successful treatment via omentalization alone when the thoracic duct could not be identified due to severe mediastinal fibrosis. The abdomen was approached paracostally, and the omentum advanced through the diaphragm was sutured in place. The omentum provides “milk spots” with lymphatic bulbs and holes in the mesothelium that provide lymphatic drainage. The lymphatics, however, enter the thoracic duct system. Other possible roles of the omentum are provision of a large venous surface area for fluid absorption or sealing of the leaking thoracic lymphatic system. The surgical treatment of chylothorax may likely change over time. Currently, TDL should obstruct every duct branch, and branches may be located on the left and right lateral walls of the aorta, so careful dissection should be done along those surfaces. En bloc or individual ligation may be done, but neither is successful alone in every case, thus the addition of pericardectomy and cistern chyli ablation to improve outcome. Open or minimally invasive approaches may be used to achieve TDL and pericardectomy, and clinician preference usually dictates whether lymphangiography and coloration are done. Either can be achieved peripherally via the popliteal lymph nodes, decreasing the need for laparotomy. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 14 RECONSTRUCTION OF THE THORACIC WALL D.J. Krahwinkel, Jr., DVM, MS, Diplomate, ACVS, ACVA, ACVECC The University of Tennessee, Knoxville, Tennessee The indications for surgical correction of the thorax include flail chest (rib fractures), pectus excavatum, cancerous lesions, and diaphragmatic hernia. We will discuss all these except the latter. All of these surgeries will require the patient to have controlled ventilation during the procedure and a chest tube postoperatively. Pectus Excavatum (Funnel Chest) Pectus excavatum is a congenital depression of the caudal 1/3-1/2 of the sternum in puppies and kittens. The depressed segment displaces the heart, compresses the lungs, and interferes with swallowing. Clinical signs are related to cardiopulmonary dysfunction and dysphagia. External repair can be performed before the thoracic wall loses its elasticity. An external vshaped splint is formed from either plaster or fiberglass that conforms to the sternum. The splint is padded with cast material. Five to six holes are placed in the splint such that 2-3 of the holes correspond to the normal sternabrae and the other 2-3 to the inverted segment. Large polypropylene sutures are placed around 2-3 normal sternabrae and around 2-3 of the inverted sternabrae that correspond with the holes in the splint. The sutures are placed through the corresponding holes in the splint. The cranial sutures are pulled tight and secured with split fishing sinkers. The inverted sternal segment is then pulled into position and secured with the split sinkers. All sutures are pulled snugly but not so tight as to cut through the soft cartilage. The sutures in the inverted segment can be tightened on a weekly basis to keep tension on the inverted sternum. The splint is kept in place for 2-4 weeks. In severe cases or in older patients, external splints may not correct the problem. Internal repair may be necessary. The entire ventral thorax is prepared for surgery. A midline incision is made the length of the sternum. The skin is reflected to expose the point where the ribs are deformed. The entire inverted sternum is mobilized by cutting between the normal and inverted sternum and the ribs attached to the sternal segment. Large polypropylene sutures (1-0) are placed around 2-3 normal and 2-3 abnormal sternabrae. A u-shaped intramedullary pin is laid along the sternum and the sutures secured around the pin to pull the sternum into a normal configuration. If the diaphragm is contracted, it may be necessary to cut it free from the sternal midline and close the defect. The subcutaneous tissues and skin are closed over the pins and sutures. Young, rapidly-growing animals will outgrow the system in 2-4 weeks. The pin can be removed by making a small incision over the u-shaped end. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 15 Thoracic Wall Tumors The most common tumors affecting the thoracic wall are osteosarcoma, chondrosarcoma, fibrosarcoma, hemangiosarcoma, and myxosarcoma. The 4 th, 5th, and 6th ribs are most commonly involved and usually in the distal rib or the costochondral junction. One report states that the median survival is 26 weeks postoperatively. Surgery is reported to be successful for excision of up to 5 adjacent ribs, although we have removed up to ribs 6-13. Reconstruction can be by direct closure for 1-2 ribs resected. Mesh (usually polypropylene) is used for most larger resections. Omentum can be advanced out of the abdomen to reinforce mesh closures (the question is whether the omentum is placed on the inside or outside of the mesh). A latissimus dorsi muscle flap can be rotated from the dorsal thorax to close ventral resection. When the caudal ribs are resected, it is preferred to advance the diaphragm to the last remaining rib. It is uncertain whether the caudal lung lobe should be removed when the advancement is cranial to the 8 th rib. An excision is performed to remove the tumor plus 1-2 ribs cranial and caudal to the tumor. At least 2 cm of normal tissue is excised dorsal and ventral to the tumor. A sheet of autoclaved polypropylene mesh is tailored to a size slightly larger than the defect so that when turned over at the edge, it results in a double-thickness margin of approximately 1 cm around the entire periphery of the prosthesis. The mesh is folded such that the cut edge is external to the body cavity. The mesh then is sutured into place under slight tension using a monofilament suture such as polypropylene or polyethylene. Soft-tissue coverage is achieved by undermining and transposing the local musculature, subcutaneous tissue, and skin. Latissimus dorsi muscle or myocutaneous flaps have been used for reconstruction. The origin of the muscle on the lumbar fascia and caudal ribs is incised and the muscle rotated ventrally to cover the defect. When the caudal ribs are excised, it is advisable to detach the diaphragm from the rib cage and advance it to the last remaining rib. The diaphragm is reattached by suturing around the rib or to a stump of intercostal muscle. The defect, now in the abdominal wall, is closed with mesh with omentum placed on the lung side to prevent adhesions of lung to the mesh. Antibiotics are administered perioperatively to help prevent infection of implants. The most common complication is seroma due to surgical trauma and foreign body effect from implants. Flail Chest (Multiple Rib Fractures) Rib fractures often occur as a result of blunt trauma or by penetrating trauma such as bite injuries or gunshot wounds. Underlying injury to the heart, lungs, and liver often presents a more important clinical disease than the rib fractures themselves. These injuries must be promptly diagnosed and treated. Simple fractures occur when there are one or more ribs injured and seldom require any care. Flail chest occurs when there are multiple adjacent ribs fractured in multiple locations. With multiple rib fractures, surgery may be indicated if the fractures are severely displaced and have resulted in injury to the internal organs. Flail chest may need to be repaired if there is resulting severe respiratory compromise and the flail segment is contributing to ongoing injury. Internal repair can be used for multiple fractures such as flail chest or when there is penetrating injury of the underlying organs. The surgical repair usually consists of orthopedic wire placed through AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 16 holes drilled into each end of the fractured rib to reappose the fracture and prevent any further injury. Most rib fractures, including flail segments, can be repaired by external fixation. Large sutures (1-0 polyethylene) are placed around the non-fractured ribs cranial and caudal to the fractured segment. The same sutures are then placed around the ribs in the flail segment. All the sutures are tied to an external stabilization device such as a padded aluminum rod or around a covered intramedullary pin. The fixation is left in place for 2-3 weeks until the ribs develop a fibrous callus. REFERENCES 1. Fossum TW, Boudrieau RJ, Hobson HP, Rudy RL: Surgical correction of pectus excavatum, using external splintage in two dogs and a cat. J Am Vet Med Assoc 195:91-7, 1989. 2. Bowman KLT, Birchard SJ, Bright RM: Complications associated with the implantation of polypropylene mesh in dogs and cats: a retrospective study of 21 cases (1984-1996). J Am Anim Hosp Assoc 34: 225-233, 1998. 3. Baines SJ, Lewis, S, White RA: Primary thoracic wall tumours of mesenchymal origin in dogs: a retrospective study of 46 cases. Vet Rec 150:335-9, 2002. 4. Halfacree ZJ, Baines SJ, Lipscomb VJ, Grierson J, Summers BA, Brockman DJ: Use of a latissimus dorsi myocutaneous flap for one-stage reconstruction of the thoracic wall after en bloc resection of primary rib chondrosarcoma in five dogs. Vet Surg 36:587-592, 2007. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 17 TRACHEAL COLLAPSE: IS SURGERY AN OPTION? D.J. Krahwinkel, Jr., DVM, MS, Diplomate, ACVS, ACVA, ACVECC The University of Tennessee, Knoxville, Tennessee YES! Tracheal collapse is a surgical disease! NO! Tracheal collapse is not curable with either medicine or surgery! Some patients are best managed medically, while others are or will soon become surgical candidates. Diagnosis of the extent and location of the collapse is central to formulating a plan for treatment. Palpation of the cervical region often reveals a flaccid, flattened trachea and stimulates a cough. The degree and severity of the collapse is best determined by radiography and tracheoscopy. Flexible endoscopy provides the opportunity to evaluate the entire airway including laryngeal function and the extent of collapse of both trachea and bronchi. Collapse is graded as I thru IV, with a grade I showing a 25% reduction in tracheal diameter, grade II a 50% reduction, grade III a 75% reduction, and grade IV a total collapse with the dorsal membrane lying on the flattened ring. Medical management includes weight loss, cough suppressants, bronchial dilators, and sedation as needed to control anxiety and excitement. Medical management is usually the first option and can result in long-term resolution of clinical signs in many cases of grade I and II collapse, as long as other medical problems are appropriately addressed. It has been reported that over 70% of cases of tracheal collapse can be managed medically long-term. Other cases are refractory to medical care and will require surgical intervention. Surgical Options The decision to intervene surgically on a patient with tracheal collapse is made when medical management can no longer provide an acceptable quality of life. These patients are “respiratory cripples” and require extensive and repeated medical care, including frequent periods of oxygen therapy. These are usually patients with grade III or IV collapse. It is essential to remind the client that surgery is not an absolute cure for tracheal collapse, but rather a treatment to improve pulmonary function. Most patients will show dramatic improvement with surgery but maintain some clinical signs such as chronic cough. Tracheal rings: Placing rings on the outside of the collapsed trachea is one option. This technique has been used successfully for many years. These are normally placed only on the collapsed cervical trachea. A ventral approach is used, and rings are used to span the collapsed portion of the trachea. If necessary, the entire cervical trachea can be repaired along with the most cranial portion of the intrathoracic trachea. This will require 4 to 7 rings with one placed approximately every centimeter (every 3rd to 4th ring). The most cranial rings are placed first, and the intrathoracic trachea retracted cranially to allow 1 to 2 rings to be placed on the intrathoracic trachea. The peritracheal tissue is gently dissected to create a tunnel around the trachea, being careful not to damage the segmental tracheal blood supply or the recurrent laryngeal nerves. Custom-made rings of the appropriate size (New Generation Devices, Franklin Lakes, NJ) are used. The slit in the ring is positioned ventrally on the trachea, and the ring sutured to the trachea with four to five 4-0 polypropylene sutures. The ventral AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 18 sutures are placed first and then used to rotate the trachea to aid in placing the dorsal sutures. Surgical magnification (2.5X) helps to see the recurrent nerve and avoid accidental damage. Postoperative medications include antibiotics (cephazolin, 20 mg/kg bid for 7 days), corticosteroids (prednisolone, 0.5 mg/kg bid for 5 days), and antitussives (hydrocodone, 2-5 mg tid). Acetylpromazine, 2-5 mg prn, is used to relieve excitement and barking. The surgical complications of tracheal ring surgery are worse in dogs over six years old with the complications including persistent cough, dyspnea, and laryngeal paralysis. Intraluminal Stents Permanently implanted internal stents have been used to support human tracheas collapsed from malacia or cancer. These have been recently successfully employed in cases of canine collapsed trachea. A stainless steel stent was placed in twenty-four dogs with 95.8% immediate improvement. Ninety-one percent were asymptomatic or markedly improved on followup. We began to use the Ultraflex® stent (Boston Scientific, Boston, MA) several years ago. We limited the use to dogs with either grade III or IV collapse who did not respond to medical management and were severely compromised by their disease. Due to the problems with this stent, we switched and are now using VetStent® (Infiniti Medical, www.infinitimedical.com.) The outcomes with this stent have been much better. Definitive diagnosis of collapsed trachea and the diameter and length of the collapse are determined by radiography and endoscopy. The diameter of the collapsed trachea and the size of the stent to be placed are determined by placing a cuffed endotracheal tube in the larynx and applying positive pressure to the airway. The maximum tracheal diameter is then measured from a lateral radiograph with the trachea under positive pressure of 20 mmHg. A 4 to 8 cm long stent is chosen with the diameter 2 mm larger than the maximum trachea size under positive pressure. The dog is anesthetized with injectable anesthetic (propofol) with oxygen provided through the endoscopy. The proximal and distal extents of the collapsed segment are determined with endoscopy. The stent catheter is positioned, and the self-expanding stent is deployed. The positioning of the stent and dilation of the trachea are confirmed with endoscopy. Anesthesia is discontinued, and the dogs are observed in the ICU overnight and then discharged the following day. Postoperative care is the same as described for tracheal rings except the prednisolone is continued for fourteen days. Stents can be placed in both cervical and thoracic trachea. The stents are available in various lengths and diameters. Most dogs will require only one stent, but some may require two placed end-toend. Most stented patients do very well long-term with only a slight cough. However, others have developed granulation tissue in the tracheal lumen over the stent; a few have fractured the stent resulting in partial re-collapse, and others have a chronic mucoid tracheitis. The granulation tissue can be treated with a two to four week course of corticosteroids. We have restented one of the broken stents, and the patient is doing okay. The mucoid tracheitis is treated with nebulization of mucolytics. Stents are very attractive for several reasons including no chance of damage to the segmental trachea blood supply or to the recurrent laryngeal nerve, can be placed quickly avoiding lengthy surgery, provide continuous support along the entire stented trachea, and subsequent stents can be placed if additional collapse occurs. We should continue to consider tracheal collapse that is nonresponsive to medical care as surgical patients for rings or stents. Studies at the University of Tennessee AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 19 We at the University of Tennessee have completed two studies on stents for tracheal collapse. The first was with the Ultraflex stent. Twelve client-owned dogs with endoscopically diagnosed tracheal collapse refractory to medical management were studied. Medical records were reviewed for 12 dogs in which 1 or more self-expanding nitinol stents were placed for the treatment of endoscopically diagnosed tracheal collapse. A total of 17 stents were placed. Survival times after stent placement ranged from 1 to 48 months. Three of 12 dogs died within 6 months after stent placement. Nine dogs survived > 1 year after stent placement, and 7 dogs survived > 2 years. Of the deceased dogs, 5 of 9 succumbed to tracheal disease. Other causes of death included congestive heart failure, cerebral neoplasia, cerebrovascular accident, and renal failure. Material failure (stent fracture) was a common complication (5/12 dogs). Other complications reported included excessive granulation tissue within the stent lumen, tracheitis, and pneumonia. Placement of an intraluminal stent with self-expanding nitinol stents was a successful palliative treatment for tracheal collapse in dogs that did not respond to medical management. Disease progression is inevitable, but substantial improvement in respiratory function may be achieved for a period of months to years. A second study was with the VetStent – Trachea®. That paper is awaiting publication. The most common breed represented in this study was the Yorkshire terrier (11/18 cases; 61.1%). Other breeds include Pomeranian (4/18; 22.2%), Pug (2/18; 11.1%), and Miniature Poodle (1/18; 5.6%). Mean age at the time of onset of clinical signs was 7.6 years (range 3.0 – 12.0 years) with a length of clinical signs before presentation ranging from 0.5 – 7.0 years. Radiographic and tracheobronchoscopic followup was available in 14/18 cases. Most common tracheoscopic findings at followup included epithelial hyperplasia, tracheitis, and bacterial tracheitis. Owner outcome assessment was available in 15/18 patients, two of which were deceased 42 and 60 days after stent placement (13% morbidity within 60 days). Of the other 13 cases, subjective classification of outcome included 13% Excellent (2/15), 27% Good (4/15), and 47% Fair (7/15). In cases where residual clinical signs were present and medication was still administered, 14/15 owners stated that they were pleased with the current clinical outcome and would have the procedure performed again in additional pets if needed. There was no statistical significance found between outcome and grade of collapse within the cervical trachea, thoracic inlet, or thoracic trachea. Survival times ranged from 42 days to 2 years and 5 months. REFERENCES 1. White RAS, Williams JM: Tracheal collapse in the dog- Is there really a role for surgery? A survey of 100 cases. J Small Anim Pract 35:191-196, 1994 2. Buback JL, Boothe HW, Hobson HP: Surgical treatment of tracheal collapse in dogs: 90 cases (19831993). J Am Vet Med Assoc 208:380-384, 1996 3. White RN: Unilateral arytenoid lateralization and extraluminal polypropylene ring prostheses for correction of tracheal collapse in the dog. J Small Anim Pract 36:151-158, 1995 4. Moritz A, Schneider M, Bauer N: Management of advanced tracheal collapse in dogs using intraluminal self-expanding biliary wallstents. J Vet Intern Med 18:31-42, 2004 5. Sura PA, Krahwinkel DJ: Self-expanding nitinol stents for the treatment of tracheal collapse in dogs: 12 cases (2001-2004). J Am Vet Med Assoc 232:228-236, 2008 AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 20 THORACOSCOPY MaryAnn Radlinsky, DVM, MS, DACVS University of Georgia, Athens, GA, USA Thoracoscopy is a rapidly emerging technique in veterinary practice. It allows for exploration, diagnosis, and therapy for many intrathoracic conditions. The procedures are usually done through 5 mm portals in most patients, larger instruments require larger ports, and small patients require smaller, specialized equipment. Traditional of endoscopic instruments can also be used in an “assisted” fashion, in which they are introduced through small thoracotomy incisions without rib retraction, which may be the cause of significant pain with thoracotomy. The rigid endoscope allows for significant illumination and magnification of intrathoracic structures; the detail is far greater than you are used to and is quite pleasing to the eye! The indications for thoracoscopy are the same as those for open surgery of the chest. The technique initially gained popularity for pericardectomy and the diagnosis of chronic pleural effusion, primarily modified transudates. All areas of the thorax can be viewed, and the patient is approached similar to either a lateral thoracotomy or median sternotomy. The same limitations are present with each approach: one entire hemothorax is accessible with the lateral approach, and both hemithoraces are accessed via a paraxiphoid approach but dorsal access is limited as for median sternotomy. Thoracoscopic skill can be built upon starting with exploration and diagnostic techniques. The instrumentation required consists of grasping and dissecting forceps, cup biopsy forceps, and retractors. Samples of pleura, mediastinum, pericardium, and lymph node are simple to obtain. The pleura may be biopsied easily with cup biopsy forceps; avoidance of the neurovascular bundles along the caudal aspects of the ribs are simple, even with thickened pleura, as the ribs are palpable. Dissection of mediastinal or hilar lymph nodes requires more skill, and dissection of the pleura followed by cup biopsy sampling can be built up into complete lymph node excision with time and practice. Mediastinal mass excision represents a great improvement in skill, dexterity, and understanding of the endoscope and view gained with the different angles of endoscope. A 0° endoscope provides an easily understood straight on view of the structures within the chest; however, the rigid chest wall makes the use of a 30° endoscope beneficial for viewing all extremes of the chest while minimizing levering against the ribs and damaging the adjacent tissues or endoscope. Pulmonary biopsy can be done along the periphery of the lung with a guillotine method using a pretied loop ligature. The lung can be evaluated for leakage following specimen collection. As experience and skill are gained, more interventional techniques can be done. Mediastinal biopsy or lymph node excision can progress to mediastinal debridement in cases of pyothorax and mediastinal mass excision for thymoma. Pericardial biopsy can be expanded to subtotal pericardectomy. Precise dissection is required for ligation and division of the ligamentum arteriosum and esophageal debridement for treatment of PRAA, and dissection and ligation of the thoracic duct may be done thoracoscopically as well. The most difficult procedure done thoracoscopically requiring the most skill is pneumolobectomy. Clearly, as skill is gained and the techniques done are expanded into therapeutic procedures, more specialized equipment is required and the ability to treat complications is also required. Minor hemorrhage during thoracoscopy obscures visualization and should be minimized. Endoscopic clip appliers, bipolar cautery, monopolar cautery, and loop ligatures may be used endoscopically to control hemorrhage. Vessel sealing devices are a great adjuvant for attempting significant debridement or mass removal. These specialized bipolar cautery type devices “read” the tissue impedance and seal the elastin and collagen of the vessel wall together and do not require a coagulum to stop blood flow. They also AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 21 have the ability to transect the tissue after it is sealed and can be used through fatty tissue without the need to specifically isolate the vessels for sealing. There are certainly limitations to the size of vessel that can be sealed with each device. The harmonic scalpel can seal vessels up to 5 mm in diameter, while the Enseal and LigaSure can seal larger vessels (up to 7 mm in diameter). The harmonic scalpel is not a cautery device but uses tissue vibration to heat and seal tissues. Position the patient as you would for a standard open approach and be ready to convert to the open approach on an emergent basis. With time and practice, endoscopic treatment of complications will become possible, but every client should be made aware that open surgery may be required in every case and time is not available for contacting them prior to doing so. Draping will need to be wider than normal, as ports will be placed in a triangulating fashion around the intended surgical target. Lateral thoracoscopy uses ports placed in a direction that targets the organ to be operated, as does the paraxiphoid approach. Place each port via a minithoracotomy to avoid pulmonary trauma. Make an incision in the intercostal space and bluntly dissect until the chest is open. Be sure that the thoracotomy is at least as large as the port, and use a port that approximates the thoracic wall thickness. The author prefers flexible ports that can be cut to size and sutured to the patient. Once a number have been cut, various sizes become available for future patients, and the flexible ports minimize the compression of the neurovascular bundles. The lack of rib retraction and nerve compression may be associated with diminished morbidity following thoracoscopic procedures. The paraxiphoid approach utilizes a screw in port adjacent to the base of the xiphoid and directed into the ipsilateral hemothorax. A 0° endoscope placed inside the port during insertion allows the endoscopist to visualize when the thorax has been entered and allows for the shortest insertion possible, minimizing the interference with visualization and instrument opening. The mediastinum must be divided early in the paraxiphoid procedure to allow evaluation of the contralateral hemothorax. With lateral or paraxiphoid thoracoscopy, another port can simply be added to gain visualization or for instrumentation introduction before conversion to an open approach. Remember that gravity is a great retractor during endoscopy, and that works within the chest as well. Atelectasis will allow the lungs to drop out of the way during the procedure, but anesthesia will become a bit more challenging. The ventilatory volume should be approximately halved, and ventilation guided by carbon dioxide and oxygen monitoring (either invasively or via capnography and pulse oximetry). Mild hypoxemia is expected but was clinically insignificant in normal animals. Beware of pleural effusion – it is your enemy for visualization. Remove as much effusion as possible early in the procedure to decrease “floating lung” and its interference with visualization. Likewise, very obese animals can be quite challenging for endoscopic surgery. Fat itself obscures structures and can put organs in the visual field during surgery. Pericardectomy via a thoracoscopic approach is the standard of care in many veterinary practices and was early evidence for the decreased morbidity of endoscopically performed techniques. A lateral or ventral approach can be used. The author prefers a ventral approach, as it allows complete exploration and access to more of the pericardium during the procedure. The pericardectomy should be started at the apex and extends cranially toward the heart base. Care should be taken to firmly grasp the pericardium with significantly long-toothed grasping forceps for pericardial elevation and stabilization during the procedure. The right atrium should be avoided, and the pericardium should be visualized on either side of the sealer or scissors prior to sealing and/or cutting to avoid cardiac, pulmonary, and nerve trauma. A window can be made, taking care to make it small or large enough to avoid cardiac herniation and entrapment. Forming a window can be followed by pericardial fenestration from apex to the phrenic AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 22 nerves in 3 places, which obviates the need for complete excision ventral to the phrenic nerves and reduces the risk of adhesion of the pericardium back to the heart. Partial pneumolobectomy requires an assisted approach and standard stapling or suturing once the chest has been exposed, lymph nodes have been evaluated, and the affected peripheral portion of lung has been exteriorized through a limited thoracotomy. The procedure can be done completely endoscopically if endoscopic GIA stapling equipment is available. With either approach, test the lung and treat leakage if necessary. Complete pneumolobectomy has been described using the endoscopic GIA in dogs. Dissection of the pulmonary attachments should be done as necessary, and apply the stapler to the hilus, ensuring complete coverage of the involved structures. Be sure to purchase the longest stapler available, as repeated stapling with multiple cartridges is more expensive than a few extra staples in the patient. Dissection and ligation of the individual structures of the pulmonary hilus is possible, but requires significant skill and intra- or extra-corporeal knot tying. The ligamentum arteriosum can be divided for treating PRAA in young animals. The site is approached laterally, from a ventral or caudal approach. Once the site is identified, dissection is done, clips are applied, and the ligament is transected. Adhesions along the esophagus are easy to see with the endoscope and can be debrided rapidly. Be ready to deal with hemorrhage if flow through a PDA and PRAA are both present. A PDA with PRAA is usually thicker and less pliable (less like a rubber band) than a ligamentum. PDAs can also be treated endoscopically or with endoscopic assistance, but the procedure has not gained popularity due to the limited sizes of clips available for treatment of many different sized PDAs. Dissection is done cranially and caudally only, avoiding medial and cranial dissection that is often associated with ductal rupture and hemorrhage. If the clips are not long enough to span the entire PDA, residual flow will be present. Thoracic duct ligation is possible with endoscopy and has been done in laterally recumbent or sternally recumbent dogs and cats. The duct may or may not be readily visible due to the thickness of the mediastinal pleura and lack of opacification with high fat food. Coloration of the duct can be achieved with a minimal approach to the popliteal lymph node for injection of dye or contrast or both. A paracostal approach to the abdomen can be done concurrently for mesenteric lymph node injection or lymphatic catheterization. The endoscope is usually inserted in the mid-thorax and the instrument ports are placed to allow dissection transversely across the aorta between intercostal vessels. The dissection should be started on the ventrolateral surface of the aorta and should be extended into the contralateral hemothorax with significant ventral retraction of the aorta to encompass contralateral ventral branches of the duct. Thoracoscopy allows for very caudal dissection and can be done bilaterally to increase effectiveness of the dissection and for placement of suture rather than hemostatic clips. Complications of thoracoscopy are the same as those with an open approach, and thoracostomy tubes are usually placed for monitoring for hemorrhage and air leakage. Nasal oxygen is usually provided for a few hours after surgery, but may not be necessary beyond that time, depending on the patient, condition, and procedure done. The minithoracotomies can be blocked with bupivacaine prior to recovery, and intrapleural bupivacaine can also be applied periodically as needed. The technique can do almost everything that open surgery can, but is limited in the presence of significant fat or adhesions. Give it a try, you just may like it! AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 23 THORACOSCOPIC MANAGEMENT OF BULLOUS EMPHYSEMA IN THE DOG Dr Hervé BRISSOT DMV, DECVS, MRCVS. DAVIES Veterinary Specialists Spontaneous pneumothorax is a non-traumatic closed pneumothorax in which the lung is the source of air accumulation. Previous retrospective studies assume that most spontaneous pneumothorax result from emphysematous disease and blebs, or bullae ruptures. In human surgery, bullous disease is treated by lobectomy with or without pleurodesis. This is currently made under thoracoscopy. In dog, the efficacy of pleurodesis to control emphysematous pneumothorax remains so far questionable and thoracic exploration associated with partial lobectomy remain the treatment of choice. The diagnosis of emphysematous disease is classically described to be achieved after imaging studies. The typical radiographic pattern of bullous disease has been described as a cystic hyperlucent zone at the margins of lung lobes. Radiographic identification of bullous disease has been reported in 5 - 50% of cases. In human medicine, tomodensitometric examination is used to detect and to localize bullae. Recent publication in a small population of dogs showed better sensitivity and sensibility of CT compared with radios in the identification of bullae. Most of the time, however, the final diagnosis is reach after definitive visualization of the lesion during the surgery. Clinical management of spontaneous pneumothorax by repeated thoracocentesis followed by chest tube aspiration has a poor prognosis (25 -100% recurrence), so surgical treatment is recommended. This requires exploratory thoracotomy, recognition of the affected tissue, and partial lobectomy. As preoperative lesion lateralization is very difficult, a median sternotomy is preferred. After surgery 3 to 25 % of recurrence is usually described in veterinary literature. In 2004, we were the first to report the use of thoracoscopy as a diagnostic and surgical tool for bullous emphysema management in dogs (cf Brissot, Dupré and coll). Three dogs were presented for treatment of persistent spontaneous pneumothorax after the failure of the conservative treatment. They were treated by mini-invasive procedure. Thoracoscopic exploration of the pleural space was performed under general anesthesia, with pulmonary ventilation but without pulmonary exclusion. A 1-cm skin incision was made 3 cm lateral to the last sternebra at the junction between the costal arch and the xyphoid process. Then a large trocar (11.5 mm) was inserted into the thoracic cavity. Under thoracoscopic control (10 mm scope), instrumental portals and endoscopic atraumatic forceps were introduced through 2 separate portals (for 5 mm and 10 mm instruments) located on the latero-ventral side of the thorax. In all dogs, the thoracoscope was pushed through the ventral mediastinum to view the controlateral lung lobes. If observation of the dorsal part of lungs was poor, the dog was rolled slightly to the side until a complete inspection could be achieved. If needed, a limited insufflation of carbon dioxide was used to create partial lung collapse and facilitate thorascopic lung manipulation. When a bulla or a pulmonary leak was identified, partial lobectomy was performed with endo-staplers If a bulla was not identified or when it was necessary to check the staples line, the thoracic cavity was filled with saline and checked for bubbles. After surgery, excised lung samples were submitted for histological examination. Partial lobectomies were performed with endoTA stapler. Parenchyma stapling was effective and no air leakage was detected from the staple lines. Surgical time ranged from 60 - 90 minutes. Lung inflation AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 24 didn’t interfere with the procedure. Drains were maintained for 2 days in each dog; but air was never aspirated after the initial 6 hours. Microscopy of resected lung tissue confirmed bullous emphysema; no neoplastic lesions were observed. Among the 3 first dogs, recurrence was not observed 18, 24, 29 months after the surgery. Our study showed that thoracoscopy was helpful for an accurate diagnosis of emphysematous bulla in dogs. With a single video portal we were able to scan all the surfaces of both lungs by pushing the thoracoscope through the mediastinum. Therefore, preoperative lateralization was not necessary. We performed thoracoscopy without pulmonary exclusion. Because exploration of both sides of the thoracic cavity was necessary, selective intubation should have been otherwise repeated. With the dog in dorsal recumbency, pulmonary exclusion was not necessary. Moreover, ventilation of both lungs was very helpful for an accurate visualization of bullae or of the parenchyma leakage. We used thoracoscopy for the definitive treatment of bullous emphysema in dogs. We didn’t make any attempt to perform pleurodesis. Under thoracoscopy we were able to perform the same procedures than in open surgery. Surgical time ranged from 60 - 90 minutes, which compares favorably with our surgical time for median sternotomy and partial lobectomy. It has been reported that thoracoscopic pericardectomy caused less post-operative pain and morbidity than “open” pericardectomy in dogs. We did not perform pain scores, but these three dogs were able to rest and walk comfortably 24 hours after the procedure. We conclude that thoracoscopy was a safe and valuable approach for the management of idiopathic pneumothorax, although pre-operative imaging is necessary to evaluate the feasibility of this approach (size of the chest cavity, potentially size of the lesion). Five years after this first study, the author will still advise minimal thoracic approach at least for diagnosis purpose to manage spontaneous pneumothorax. REFERENCES Brissot HN, Dupré GP, Bouvy BM, Paquet L. Thoracoscopic treatment of bullous emphysema in 3 dogs. Vet Surg. 2003 Nov-Dec; 32(6):524-9. Au JJ, Weisman DL, Stefanacci JD, Palmisano MP. Use of computed tomography for evaluation of lung lesions associated with spontaneous pneumothorax in dogs: 12 cases (1999-2002). J Am Vet Med Assoc. Mar 1; 228(5):733-7, 2006 Holtsinger RH, Beale BS, et al: Spontaneous pneumothorax in the dog: a retrospective analysis of 21 cases. J Am Anim Hosp Assoc 29: 195-210, 1993. Puerto DA, Brockman DJ, Lindquist C, et al: Surgical and nonsurgical management of selected risk factors for spontaneous pneumothorax in dogs: 64 cases (1986-1999). J Am Vet Med Assoc 220:16701674, 2002. Dupré GP, Corlouer JP, Bouvy B: Thoracoscopic pericardectomy performed without pulmonary exclusion in 9 dogs. Vet Surg 30:21-27,2001. De Rycke LM, Gielen IM, Van Ryssen B, et al: Thoracoscopic anatomy of dogs positioned in lateral recumbency. J Am Anim Hosp Assoc 37: 543-548, 2001. Jerram RM, Fossum TW, Berridge BR, et al: The efficacy of mechanical abrasion and talc slurry as methods of pleurodesis in normal dogs. Vet Surg 28: 322-332, 1999. OPEN VERSUS CLOSED PERICARDECTOMY IN THE DOG AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 25 Dr Hervé BRISSOT DMV, DECVS, MRCVS. DAVIES Veterinary Specialists Pericardial effusion is associated with cardiac tamponade and right sided heart failure. The origin of the effusion can be traumatic, inflammatory (more often septic) or neoplastic. Pericardectomy has been demonstrated to be very useful as a diagnostic procedure (histology of the pericardium) or as a definitive (idiopathic, traumatic or infectious diseases) or palliative (neoplasia) treatment. Although feasible after midline sternotomy, pericardectomy is usually performed via a right sided thoracotomy at the level of the 4th intercostal space. After rib retraction, the heart is isolated from the lungs, the phrenic nerve identified and a subphrenic pericardectomy is performed. As visualisation of the left part of the pericardium is impossible with this approach, the procedure aims to create a large lateral pericardial window with mild extension toward the left part rather than a full subphrenic pericardial excision. The theory associated with pericardectomy is to create a large pericardial defect to allow free drainage within the pleural space without the risks of secondary healing that might close the defect or that could create a fibrotic ring around the heart. For this purpose the usual aim of the surgeon is to create a large pericardial window: a defect of roughly 5x5cm for a median size dog. For the last 10 years with increased availability of rigid endoscopy, minimally invasive approaches have been described to perform therapeutic pericardectomy. Two main techniques are described for thoracoscopic pericardectomy: 1/Under general anesthesia, with pulmonary ventilation but without pulmonary exclusion as described by Dupré and coll in 2001. The patient is prepared as for a sternotomy, lying in dorsal recumbency with a large chest clip. A 1-cm skin incision is made 3 cm lateral to the last sternebra at the junction between the costal arch and the xyphoïd process; then an optical port is inserted into the thoracic cavity, under thoracoscopic control instrumental ports are introduced on the latero-ventral sides of the thorax, usually at the level of the 5th intercostal space. In all dogs, the thoracoscope is pushed through the ventral mediastinum to view both sides of the heart and to allow introduction of instruments in both sides of the chest. If observation of the lateral aspect of the heart is poor, the dog is rolled slightly to the side until a complete inspection can be achieved. If needed, a limited insufflation of carbon dioxide is used to create partial lung collapse and facilitate thorascopic lung manipulation. Using surgical instruments such as grasping forceps and scissors, a pericardectomy is performed ventral to the phrenic nerve. This procedure might be associated with local bleeding that may obstruct visualisation and therefore bipolar electric coagulation or advanced sealing devices are indicated to perform the procedure. 2/ Lateral thoracoscopy described byJackson and coll, and Walsh and coll, (published in 1999). The patient is prepared as for an exploratory thoracotomy and lung exclusion is performed (initially left or right sided pericardectomy were performed). This allows further exploration of the pleural space without the inconvenience of a ventilating lung. Of course, an intact mediastinum makes this exploration easier. The optical port is positioned dorsally at the level of 3rd to 6th intercostals space, dorsally to allow correct visualisation of the lateral aspect of the heart. The triangulation and the placement of 2 instrumental ports is performed to achieve, if necessary, additional retraction, before identifying the phrenic nerve. A 5 cm pericardial window is created. In each procedure, excised tissues are submitted for histological examination, attention is made to prevent contact of the pericardium with the thoracic wound at the time of removal to prevent any risk of tumor seeding and a chest drain is placed. Both described techniques are well recognised as suitable for idiopathic effusions, although they appear more useful for creating a pericardial window rather than extensive subtotal pericardectomy: the first AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 26 technique causes the ventilating lung to obstruct the dorsal aspect of the pericardium and the phrenic nerve. The second technique has the same limitations as the classic open approach with absence of visualization of the left side. They do however allow pericardioscopy to be performed on the right side of the heart which is the most common location of heart base tumor (but visualization remains very difficult). In the case of severe effusion, it can be challenging for the surgeon to safely opening the pericardial sac thoracoscopically. Direct incision of the tensed pericardium with a scalpel blade is sometimes required in these more complicated cases. This could be challenging for trainee thoracoscopists. It appears otherwise that closed pericardectomy is a safe procedure, although large surveys reporting surgical findings, outcomes and complications are required. In the early report of Jackson and coll in 1999, 13 dogs had lateral thoracoscopy, one had lung laceration, one had phrenic nerve laceration and one had moderate bleeding, all showed complete relief of the clinical signs of tamponade although 10 presented with neoplastic effusion. In a survey of 9 dogs, Dupré and coll reported subphrenic pericardectomy with 1 cm margin ventrally to the phrenic nerve without postoperative morbidity. Since these initial reports, both procedures appear to be widely performed as a standard treatment for pericardial effusion, and both authors claim to achieve good results with large pericardial windows (4 to 5 cm diameter) rather than strict subphrenic pericardectomy. Walsh and coll were the first to investigate the benefits of closed pericardectomy versus the classic open procedures in normal dogs. The study showed that the procedures (the amount of pericardium removed, in this case 5x5cm pericardial window) were successfully performed within 45 minutes, with a quicker and less painful recovery and with less wound complications. This was later confirmed by Dupré although the technique was different. Ten years after the first descriptions of closed pericardectomy, the techniques are widely used with good results in every size of dog and even in cats. However at that time there is no report comparing clinical populations with long term results. It is possible that creating only pericardial windows may be associated with poorer long term results, as the underlying pericardial disease may be missed, or too much pericardial tissue may remain in very exudative idiopathic effusions. Few authors have reported cases of patients that needed a 2nd open surgical intervention after an initial thoracoscopic surgery, although anecdotally further investigations would be necessary to clearly indentify the limits of the thoracoscopic procedure or the exact amount of tissue to be resected. REFERENCES Jackson J, Richter KP, Launer DP. Thoracoscopic pericardietcomy in 13 dogs. J Vet Intern Med 1999, 13: 529-533. Dupré GP, Corlouer JP, Bouvy B: Thoracoscopic pericardectomy performed without pulmonary exclusion in 9 dogs. Vet Surg 30:21-27, 2001. De Rycke LM, Gielen IM, Van Ryssen B, et al: Thoracoscopic anatomy of dogs positioned in lateral recumbency. J Am Anim Hosp Assoc 37: 543-548, 2001. Walsh PJ, Remedios AM, Ferguson JF, et al: Thoracoscopic versus open pericardectomy in dogs: comparison of postoperative pain and morbidity. Vet Surg 28: 472-479, 1999. Landreneau RJ, Hazelridge SR, Mack MJ, et al: Postoperative pain-related morbidity: video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg 56: 1285-1289, 1993. Cantwell SL, Duke T, Walsh PJ, et al: One-lung versus two-lung ventilation in the closed-chest anesthetized dog: a comparison of cardiopulmonary parameters. Vet Surg 29: 365-373, 2000. Monnet E. Interventional thoracoscopy in small animals. Vet Clin North Am. 39, 965-975, 2009 AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 27 SURGICAL MANAGEMENT OF THYMOMAS D. J. Brockman BVSc CertVR CertSAO DipACVS DipECVS The Royal Veterinary College Arthur K House and Daniel J Brockman ANATOMY OF THE MEDIASTINUM The mediastinum is the potential space between the right and left pulmonary pleural sacs that, in the normal dog or cat, contains the heart, great vessels, trachea, oesophagus, lymph nodes, and thymus. Occasionally, ectopic thyroid and parathyroid tissue resides within the mediastinum. The thoracic spine forms the dorsal mediastinal border and the sternum forms the ventral border. The cranial and caudal borders are formed by the thoracic inlet and diaphragm, respectively. The lateral borders are formed by the mediastinal or parietal pleura, which separates one hemithorax from the other. Although the mediastinal pleura is not truly “fenestrated”, its delicate nature frequently allows extension of disease from one side of the chest to the other. In the cranial thorax, the mediastinum is just to the left of midline; the mediastinal pleura joins the costal pleura to form the cupula pleura, which extends cranially beyond the first rib on each side. The cranial mediastinum communicates with fascial planes of the neck. In the caudal thorax, the mediastinum is continuous with the pericardium but deviates to the left of the midline to accommodate the accessory lung lobe. It attaches to the left side of the diaphragm, contacting the left thoracic wall near the ninth sternochondral junction to form the sternopericardial ligament. Caudally, the mediastinum communicates with the retroperitoneal space through the aortic hiatus. The caudal vena cava resides in a reflection of the parietal pleura, the plica vena cava, on the right side of the mediastinum. To assist radiographic interpretation the mediastinum is divided into five regions: craniodorsal, cranioventral, middle, caudodorsal, and caudoventral. CLINICAL FEATURES OF MEDIASTINAL DISEASE. Neoplastic or inflammatory conditions of the mediastinum are associated with vague clinical signs such as pyrexia, weight loss, reduced appetite, and malaise. Such disease processes may also affect the recurrent laryngeal nerves, causing laryngeal paralysis, the vagosympathetic trunk, causing Horner’s syndrome. In addition, mass lesions may compress the oesophagus, trachea, and major vessels resulting in regurgitation, coughing and dyspnoea, and either cranial or caudal venous hypertension and oedema (cranial or caudal caval compression syndrome). Because of the anatomy, diseases affecting the mediastinum may extend into the neck or abdomen (and vice-versa), along the continuous fascial planes. Cervical oesophageal perforation can, therefore, lead to septic mediastinitis; conversely, intrathoracic tracheal injury can lead to cervical +/- subcutaneous emphysema. In cats, a large mass occupying the cranial mediastinum will often reduce the compressibility of the cranial rib cage. In addition, some mediastinal neoplasms are associated with paraneoplastic syndromes such as the hypercalcaemia occasionally associated with lymphoma causing polyuria and polydipsia, and focal or generalized myasthenia gravis associated with mediastinal thymoma. A wide variety of non-specific clinical signs can, therefore, be associated with mediastinal disease. EVALUATION OF THE MEDIASTINUM Physical examination of the mediastinum is limited to establishing the compressibility of the cranial thorax and to thoracic auscultation. Abnormalities of these physical examination techniques are not specific to mediastinal disease. Diagnostic imaging techniques including survey and contrast radiography, ultrasound examination, and endoscopy are non-invasive steps that may be necessary to characterise mediastinal disease. Advanced imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) are being used increasingly to provide more specific information about the relationship of mediastinal neoplasia, in particular, to other structures contained within the mediastinum (Fujimoto and others 1992, Pirronti and others 2002). For tissue diagnosis or collection of samples for AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 28 culture or biochemistry, more invasive techniques such as ultrasound guided fine needle aspiration or core tissue biopsy, and surgical exploration are required. RADIOGRAPHIC EVALUATION OF THE MEDIASTINUM In the absence of disease, the mediastinum is an unclear radiographic anatomical region that lacks contrasting tissue densities except for the air filled trachea. The cranioventral region is more radio-opaque as it is thicker. The craniodorsal and caudodorsal regions are best viewed on either a ventrodorsal or dorsoventral radiographic projection. In the normal patient, the mediastinum is no wider than twice the width of the thoracic spine, although in obese animals the craniodorsal region may become wider due to the accumulation of fat. The middle region of the mediastinum is best viewed on a lateral projection. In young dogs, the thymus is viewed as a triangular structure in the cranioventral region of the mediastinum, often referred to as the thymic sail. Four general radiographic observations are made in the presence of disease; these are: mediastinal shift, pneumomediastinum, mediastinal fluid, and mediastinal masses. Mediastinal shift occurs secondary to a unilateral increase or decrease in lung volume or secondary to the presence of an intrathoracic mass. Mediastinal shift generally does not indicate disease of the mediastinum, rather disease in the lungs, bronchi, thoracic wall or pleura. Pneumomediastinum is the accumulation of free gas within the mediastinum; this provides contrast and enhances the outer walls of mediastinal structures such as the trachea, oesophagus and great vessels. Pneumomediastinum is best observed on a lateral radiograph, as the width of the mediastinum is not significantly increased. The source of air may be the trachea, main stem bronchi, marginal alveoli or oesophagus. Extension of gas from the cervical region caudally or from the retroperitoneum cranially into the mediastinum can also occur. Pneumomediastinum occasionally progresses to a pneumothorax, especially in cases of trauma or when large defects in the trachea or main stem bronchi are present. As previously mentioned, concurrent subcutaneous emphysema may develop in such animals. Mediastinal widening viewed in ventrodorsal or dorsoventral radiographic projections can be secondary to diffuse mediastinal disease such as mediastinitis or mediastinal fluid accumulation, or focal mediastinal disease such as mediastinal neoplasia (Figures 4 and 5). In the latter, distortion of adjacent structures, especially the trachea, is frequently seen. Mediastinal fluid accumulation causes diffuse soft tissue opacity and may occur in conjunction with a mediastinal mass or secondary to inflammatory disease. Diffuse widening of the mediastinum is more typical of mediastinal fluid and inflammatory disease whereas focal widening is more consistent with a neoplasm. ULTRASONOGRAPHY OF THE MEDIASTINUM Ultrasonographic examination of the normal mediastinum is limited by the lack of a reliable acoustic window. In the presence of a pleural effusion or a cranial mediastinal mass, significant information can be acquired using thoracic ultrasound. The transducer may be placed in a parasternal position or alternatively at the cardiac notch, using the heart as an acoustic window. Transoesophageal transducers can be used to acquire images of the heart base and major vessels within the mediastinum. In the investigation of cranial mediastinal masses, ultrasonography can provide useful information regarding the architecture of the mass and its relationship with adjacent structures. Ultrasound guided fine needle aspiration or core biopsy techniques can be performed. ADVANCED IMAGING Computed tomography (CT) and magnetic resonance imaging (MRI) are the most powerful imaging modalities for estimating the location, volume and invasiveness of mediastinal neoplasms. Difficulties in distinguishing mass from collapsed lung may be experienced with both modalities. Radionucleotide studies using either Iodine 131 or Technetium 99m have been used to identify ectopic or metastatic thyroid tissue in the mediastinum. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 29 MEDIASTINAL NEOPLASIA Soft tissue masses within the mediastinum are rare, but when present, they can usually be seen readily on plain thoracic radiographs. The most common primary mediastinal neoplasms are thymic lymphosarcoma and thymoma. Other mass lesions include mediastinal lipoma, pleural or bronchial neoplasia, enlarged mediastinal lymph nodes, abscesses and granulomata, oesophageal foreign bodies, congenital diaphragmatic hernias, gastro-oesophageal intussusception, adenomatous ectopic thyroid tissue, vascular lesions (such as chemodectoma), and benign cysts arising from embryonic branchial pouch. Opacities that are occasionally confused with mediastinal masses include fat in obese dogs, the thymus of young dogs, and tumours of the pulmonary parenchyma, especially those affecting the accessory lung lobe. The clinical features of any mediastinal neoplasm depend on either invasion or compression of local structures. Compression of the oesophagus and trachea in the cranial mediastinum may result in coughing dyspnoea, dysphagia, and regurgitation. Occasionally, oedema of the head, neck, and forelimbs is observed secondary to compression of the cranial vena cava (cranial vena cava syndrome). If the vagus nerves are infiltrated or compressed, changes such as altered phonation, inspiratory stridor and chronic cough associated with laryngeal paralysis may be present. Consequently, the diagnostic investigation of suspected laryngeal paralysis should include thoracic radiographs to rule out the presence of a mediastinal mass. Similarly, the sympathetic trunk may be damaged, leading to the development of Horner’s’ syndrome. In conjunction with these potential clinical signs, pleural effusion, pneumothorax, chylothorax, chylopericardium, and haemothorax have been observed, particularly in mediastinal lymphoma and invasive thymoma in dogs. As previously mentioned, paraneoplastic syndromes have been associated with thymic neoplasia in humans, dogs, and cats; most notably, acquired myasthenia gravis and megaoesophagus, and less commonly, hypercalcaemia and other immune-mediated diseases (Bellah and others 1983, Atwater and others 1994). A large percentage of human patients with myasthenia gravis have thymic abnormalities, either neoplastic or non-neoplastic (Robertson and others 1998, Mantegazza and others 2003). The incidence of acquired myasthenia gravis with thymoma in dogs is approximately 30% (Bellah and others 1983, Atwater and others 1994). Malignant mediastinal lymphadenopathy Mediastinal lymphadenopathy affecting the sternal, cranial mediastinal or tracheobronchial lymphocentrum is most commonly due to either multicentric neoplasia such as lymphoma, mastocytosis, malignant histiocytosis, or metastatic bronchopulmonary disease. All of the neoplastic causes are considered multi-centric and as such, surgical excision is of no therapeutic value once a diagnosis is confirmed. With the exception of lymphoma, they are poorly responsive to anti-cancer drug protocols. Thymic neoplasia Thymoma and thymic carcinoma are the most commonly reported primary thymic tumours in dogs and cats. Of these, thymoma is the most common. The clinical features of thymoma are vague and often mild until compression of the lungs and/or airways causes breathing difficulty. As previously mentioned, occasionally, animals with this disease will present with signs referable to a paraneoplastic syndrome such as myaesthenia or hypercalcaemia. The diagnosis is often suspected on the basis of plain thoracic radiographs and may be confirmed by cytological examination of fine needle aspirates. Occasionally, core biopsies or excisional biopsies are required to achieve definitive diagnosis. The biological behaviour of thymoma does not correlate well with the histological appearance of the neoplasm. Thymomas are, therefore, described as “invasive” or “non-invasive”, on the basis of gross local tissue invasion. Local metastases are uncommon but can be seen in the lungs, lymph nodes, diaphragm, and pericardium. Distant metastasis is rare but has been reported to the kidneys, liver, and spleen. Local invasion of the vascular system is also seen occasionally. The prognosis for animals with non-invasive non-metastatic thymoma following complete excision is good (provided that paraneoplastic syndromes are either not present or controllable), whereas the prognosis for animals with invasive or metastatic thymoma is poor. Theoretically, pre-operative assessment of local disease should be critical to clinical decision-making. The degree of local tissue invasion is difficult to determine on the basis of plain thoracic radiography, therefore, advanced imaging such as MRI and CT is often recommended to provide AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 30 additional information about the local disease. Unfortunately, many animals are presented with extremely large mediastinal masses, which complicates differentiation between invasion and ‘mass effect’ (Fujimoto and others 1992, Pirronti and others 2002). Surgical excision is indicated in the management of thymoma and exploration of the thorax is generally required to confirm or refute the suspicion of local invasion based on imaging. Although exploration can be performed via lateral thoracotomy, sternotomy is often preferable because of the size of the tumour. Non-invasive thymomas can be readily removed with blunt dissection. Preservation of structures such as the phrenic nerves and accurate haemostasis of larger vessels is essential. Attempted excision of invasive thymomas can be unrewarding due to the invasion of vital structures. Cranial caval replacement with a jugular autograft has been described in dogs to achieve en bloc tumour excision when the cranial vena cava has been invaded. Cytoreductive surgery such as this may be palliative for a prolonged period of time. Postoperative monitoring by physical examination and thoracic radiography every three to six months is recommended to detect tumour recurrence or development of myasthenia gravis and secondary megaoesophagus. Recurrence rates are not well documented but based on the limited literature available recurrence appears to occur in approximately 30% of dogs (Aronsohn 1985, Gores and others 1994). Cats appear to respond extremely well to surgical excision with long-term remission. In a retrospective study of 10 cats, no recurrence was observed in a six to thirty-six month follow-up period (Gores and others 1994). A staging system exists in humans that is of prognostic value. In non-invasive forms, recurrent disease is approximately 2% compared to 20% in invasive forms that are successfully excised at surgery (Monden and others 1984, Monden and others 1985). In dogs, the presence of myasthenia gravis and megaoesophagus are the most important prognostic indicators. Dogs with non-invasive thymoma and no paraneoplastic megaoesophagus appear to have a good prognosis for survival. Invasive thymoma in the presence of megaoesophagus carries a grave prognosis with high postoperative morbidity and mortality (Bellah and others 1983, Atwater and others 1994). Resolution of myasthenia gravis following thymectomy occurs in approximately 30% of human patients with significant improvement in approximately 60% - 70% (Drachman 1994). The response of acquired myasthenia gravis to thymectomy in dogs and cats is poorly described with single reports of either persistent or resolved disease following surgery (Gores and others 1994, Lainesse and others 1996). The development of myasthenia gravis following excision of thymoma has been observed in both humans and dogs. The pathogenesis of acquired myasthenia gravis in thymoma patients is not understood but appears to result from immune dysfunction and the development of autoantibodies against acetylcholine receptors (Garlepp and others 1984, Paciello and others 2003). Other immune-mediated diseases that have been associated with thymoma in dogs and cats include polymyositis and immune-mediated skin disease in the dog, and myositis, acute moist dermatitis, phemphigus foliaceous, superficial necrolytic dermatitis and hypogammaglobulinaemia in the cat (Willard and others 1980, Carpenter and Holzworth 1982, ForsterVan Hijfte and others 1997, Day 1997). How these diseases respond to excision of the thymoma is unknown. Non-thymic tumours are occasionally seen in association with thymoma in dogs, cats and humans. Up to ten percent of human patients with thymoma may have additional non-thymic neoplasia. Seven of twentytwo and five of twenty-three dogs with thymoma in two separate retrospective studies had additional neoplasms (Bellah and others 1983, Atwater and others 1994). Lymphoma and primary lung tumours are the most commonly reported concomitant tumours reported in dogs and cats. A failure of the thymusdependent immune surveillance is thought to be responsible for the development of these concomitant tumours. This fact means that great care should be taken when evaluating animals with thymoma both before and during surgery. Radiation therapy has been used as an adjunctive therapy prior or post-surgery or as a solitary protocol in both dogs and cats. In one study of 17 dogs and 7 cats, complete resolution of tumour was rare although partial responses was observed in 75% with greater than 50% reduction in tumour size and improvement in clinical signs (Smith and others 2001). Median survival times reported were 248 days in dogs and 720 days in cats. Fatal pneumonitis occurred in one animal with minimal side effects reported in the other cases. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 31 The value of chemotherapy has not been demonstrated in canine and feline patients. Following surgical excision, chemotherapy is not required as metastasis is rare. Response to chemotherapy, typically protocols using cisplatin, has been observed in human patients with invasive thymoma. References 1. Aronsohn, M. (1985) Canine thymoma. Vet.Clin.North Am.Small Anim Pract. 15;4:755-767. 2. Atwater, S. W., Powers, B. E., Park, R. D., Straw, R. C., Ogilvie, G. K., and Withrow, S. J. (1994) Thymoma in dogs: 23 cases (1980-1991). J.Am.Vet.Med.Assoc. 205;7:1007-1013. 3. Bellah, J. R., Stiff, M. E., and Russell, R. G. (1983) Thymoma in the dog: two case reports and review of 20 additional cases. J.Am.Vet.Med.Assoc. 183;3:306-311. 4. Carpenter, J. L. and Holzworth, J. (1982) Thymoma in 11 cats. J.Am.Vet.Med.Assoc. 181;3:248251. 5. Day, M. J. (1997) Review of thymic pathology in 30 cats and 36 dogs. J.Small Anim Pract. 38;9:393-403. 6. Drachman, D. B. (1994) Myasthenia gravis. N.Engl.J.Med. 330;25:1797-1810. 7. Forster-Van Hijfte, M. A., Curtis, C. F., and White, R. N. (1997) Resolution of exfoliative dermatitis and Malassezia pachydermatis overgrowth in a cat after surgical thymoma resection. J.Small Anim Pract. 38;10:451-454. 8. Fujimoto, K., Nishimura, H., Abe, T., Edamitsu, O., Uchida, M., Kumabe, T., Ueda, H., Sakoda, J., Kojima, K., Uozumi, J.(1992) [MR imaging of thymoma--comparison with CT, operative, and pathological findings] Nippon Igaku Hoshasen Gakkai Zasshi 52;8:1128-1138. 9. Garlepp, M. J., Kay, P. H., Farrow, B. R., and Dawkins, R. L. (1984) Autoimmunity in spontaneous myasthenia gravis in dogs. Clin.Immunol.Immunopathol. 31;2:301-306. 10. Gores, B. R., Berg, J., Carpenter, J. L., and Aronsohn, M. G. (1994) Surgical treatment of thymoma in cats: 12 cases (1987-1992). J.Am.Vet.Med.Assoc. 204;11:1782-1785. 11. Lainesse, M. F., Taylor, S. M., Myers, S. L., Haines, D., and Fowler, J. D. (1996) Focal myasthenia gravis as a paraneoplastic syndrome of canine thymoma: improvement following thymectomy. J.Am.Anim Hosp.Assoc. 32;2:111-117. 12. Mantegazza, R., Baggi, F., Antozzi, C., Confalonieri, P., Morandi, L., Bernasconi, P., Andreetta, F., Simoncini, O., Campanella, A., Beghi, E., and Cornelio, F. (2003) Myasthenia gravis (MG): epidemiological data and prognostic factors. Ann.N.Y.Acad.Sci. 998;413-423. 13. Meadows, R. L., MacWilliams, P. S., Dzata, G., and Meinen, J. (1993) Chylothorax associated with cryptococcal mediastinal granuloma in a cat. Vet.Clin.Pathol. 22;4:109-116. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 32 14. Monden, Y., Nakahara, K., Iioka, S., Nanjo, S., Ohno, K., Fujii, Y., Hashimoto, J., Kitagawa, Y., Masaoka, A., and Kawashima, Y. (1985) Recurrence of thymoma: clinicopathological features, therapy, and prognosis. Ann.Thorac.Surg. 39;2:165-169. 15. Monden, Y., Nakahara, K., Kagotani, K., Fujii, Y., Masaoka, A., and Kawashima, Y. (1984) Myasthenia gravis with thymoma: analysis of and postoperative prognosis for 65 patients with thymomatous myasthenia gravis. Ann.Thorac.Surg. 38;1:46-52. 16. Paciello, O., Maiolino, P., Navas, L., and Papparell, S. (2003) Acquired canine myasthenia gravis associated with thymoma: histological features and immunohistochemical localization of HLA type II and IgG. Vet.Res.Commun. 27 Suppl 1;715-718. 17. Pirronti, T., Rinaldi, P., Batocchi, A. P., Evoli, A., Di Schino, C., and Marano, P. (2002) Thymic lesions and myasthenia gravis. Diagnosis based on mediastinal imaging and pathological findings. Acta Radiol. 43;4:380-384. 18. Robertson, N. P., Deans, J., and Compston, D. A. (1998) Myasthenia gravis: a population based epidemiological study in Cambridgeshire, England. J.Neurol.Neurosurg.Psychiatry 65;4:492-496. 19. Smith, A. N., Wright, J. C., Brawner, W. R., Jr., LaRue, S. M., Fineman, L., Hogge, G. S., Kitchell, B. E., Hohenhaus, A. E., Burk, R. L., Dhaliwal, R. S., and Duda, L. E. (2001) Radiation therapy in the treatment of canine and feline thymomas: a retrospective study (1985-1999). J.Am.Anim Hosp.Assoc. 37;5:489-496. 20. Willard, M. D., Tvedten, H., Walshaw, R., and Aronson, E. (1980) Thymoma in a cat. J.Am.Vet.Med.Assoc. 176;5:451-453. Further Reading 1) Ettinger, Stephen J. and Feldman, Edward C. (2000) Textbook of Veterinary Internal Medicine, Diseases of the Dog and Cat, 5th Edition, WB Saunders, Philadelphia 2) Morrison, Wallace B. (1998) Cancer in Dogs and Cats, Medical and Surgical Management, Williams and Wilkins, Baltimore 3) Slatter, Douglas H. (2003) Textbook of Small Animal Surgery, 3rd Edition, WB Saunders Philadelphia 4) Thrall, Donald E. (1998) Textbook of Veterinary Diagnostic Radiology, 3 rd Edition, WB Saunders, Philadelphia 5) Withrow, Stephen J. and MacEwan, E. Gregory (2001) Small Animal Clinical Oncology, 3 rd Edition, WB Saunders, Philadelphia AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 33 POLYNEUROPATHY AS A CAUSE OF LARYNGEAL PARALYSIS D. J. Krahwinkel, Jr., DVM, MS, Diplomate, ACVS, ACVA, ACVECC The University of Tennessee, Knoxville, Tennessee Introduction Laryngeal paralysis results when there is a disruption of the abductor muscles of the larynx. The disease may be unilateral, but more commonly occurs bilaterally. Large breed, older dogs are more commonly affected, with the Labrador predominating. Saint Bernards, Irish Setters, and Afghans are frequently affected. The disease has been reported to occur congenitally in the Bouvier, Husky, Bulldog, and Rottweiler. Smaller animals such as poodles and cats may be affected. Etiology In many instances, the cause of laryngeal paralysis is unknown. Some animals may be affected secondary to trauma of the cervical region and injury to the recurrent laryngeal nerves. Other causes of injury to these nerves include lesions of the neck or mediastinum such as abscesses, tumors, or surgical intervention. Other dogs with laryngeal paralysis have also been shown to be hypothyroid which may contribute to the disease in some manner. Myasthenia gravis results in a generalized muscular weakness, including laryngeal paralysis. Most cases are truly idiopathic; however, one must rule out any and all other causes of laryngeal paralysis. Clinical Signs Individual animals with laryngeal paralysis most commonly exhibit noisy, stridorous breathing. There is a poor exercise tolerance for working animals. These dogs become progressively more dyspneic and noisy as they exercise. A change in the tone of the bark (dysphonia) is evident along with occasional episodes of severe dyspnea, cyanosis, and collapse. A soft, moist, chronic cough is frequently observed due to a dysfunction in proper closure of the glottis during swallowing. Dogs with a history of vomiting often present with aspiration pneumonia and have a poor prognosis. Physical Examination Physical examination of the patient usually provides little useful information. Auscultation of the upper airway will usually reveal stenotic and increased upper airway sounds. Under exercise and stress, these animals may become extremely dyspneic and cyanotic. Muscle weakness may be represented by rear limb weakness or swallowing difficulty. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 34 Diagnosis Radiographic evaluation of the airway is usually done to rule out other respiratory diseases. A megaesophagus may be observed in animals who have generalized neuromuscular disease. Diagnosis is generally made by observation of laryngeal function under light anesthesia. The animal must be light enough that the cough and gag reflex are present when the examination is performed. Failure to equally abduct the arytenoid cartilages bilaterally during inspiration or cough is diagnostic of laryngeal paralysis. Laryngeal paralysis patients commonly have an inflamed larynx with a large amount of mucous. Doxapram can be used to increase respiratory effort and aid diagnosis. Paradoxical motion of the larynx may be seen during examination. Transnasal tracheoscopy can be used but is probably no better than direct visualization. Ultrasound has also been used in diagnosis. Treatment Medical treatment includes weight loss, heat stroke prevention, oxygen as needed for hypoxia, sedation for excitement/anxiety, and thyroid supplements for hypothyroid patients. There is no medical cure. Surgical treatment of laryngeal paralysis has been done with partial laryngectomy (partial arytenoidectomy), vocal fold excision, laryngofissure, or laryngeal "tie-back" procedure. Laryngeal Tie-back The objective of this surgical procedure is to enlarge the laryngeal opening by surgically retracting the arytenoid cartilage on one side of the larynx. The procedure may be done on either the left or right side. The neck is extended over a small sandbag to elevate the larynx for increased surgical exposure. A skin incision is made from the level of the ramus of the mandible, ventral to the jugular vein to a level just caudal to the bifurcation of the jugular vein. The subcutaneous musculature and connective tissues are separated directly over the lateral wing of the thyroid cartilage. The thyropharyngeus muscle is incised at its attachment to the rim of the thyroid cartilage. The wing of the thyroid cartilage is reflected laterally by blunt dissection of the connective tissue on its medial border and separation of the cricothyroid articulation. The muscular process of the arytenoid cartilage can usually be palpated as a small protrusion on the lateral surface of the larynx. The cricoarytenoid muscle that attaches at this point is usually atrophied, making the process particularly prominent. Dissection is begun under the muscular process with small blunt scissors, and the arytenoid cartilage is disarticulated from the cricoid cartilage immediately beneath the muscular process. This articulation is identified by the presence of articular cartilage. Once totally separated from the cricoid cartilage, the muscular process of the arytenoid cartilages is freely movable. Some surgeons prefer to additionally sever the sesamoidian band that connects the left and right arytenoid cartilages across the dorsal aspect of the larynx. This small band of tissue is approximately 1 mm in diameter, and when excised permits the arytenoids to become mobilized. Preferably two sutures are placed from the muscular process of the arytenoid to the caudal rim of the cricoid lateral to the dorsal midline. After these sutures have been placed and before they are tied, an assistant should examine the laryngeal opening with a laryngoscope to ensure that the "tie-back" procedure has resulted in lateralization of the arytenoid cartilage. It is very easy to over-abduct the arytenoid cartilage resulting in severe dysfunction of the larynx after surgery due to inability of the epiglottis to totally close the abducted larynx. Absorbable sutures are used to reapproximate the severed thyropharyngeus muscle and the subcutaneous tissue. The skin is closed with monofilament nonabsorbable sutures. AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 35 Postoperative Care for Laryngeal Tie-back Postoperatively the animals with laryngeal "tie-back" surgery may have discomfort in swallowing and may exhibit coughing after eating or drinking. This is most likely due to a slight deformity of the laryngeal opening which is not properly occluded by the glottis. Exercise should be avoided for six weeks to permit sufficient time for healing to occur. The animal should be kept quiet and tranquilized if necessary to prevent barking. Postoperative Problems of Laryngeal Tie-back Aspiration and cough are inevitable problems regarding any type of laryngeal paralysis surgery. Fixing the arytenoid cartilage in an abducted position will almost always result in some laryngeal incompetence; therefore, the client should be advised that a slight and permanent cough is to be expected. Should the procedure fail due to breakage of the muscular process or breakage of a suture, it will be necessary to repeat the operation on the opposite side. Studies at the University of Tennessee We recently completed a study at the University of Tennessee on a series of laryngeal paralysis cases (will be published soon in the JAAHA). The purpose of this study was to investigate a group of mature dogs presented to our hospital with acquired laryngeal paralysis and histologically confirm the presence of generalized polyneuropathy. In this study, electrodiagnostic testing and histopathology were evaluated in laryngeal and pelvic limb muscles and nerves to test the hypothesis that dogs with acquired laryngeal paralysis have a generalized polyneuropathy complex. To the author’s knowledge, no previous study has described histopathologic findings from biopsies of the recurrent laryngeal nerve and cricoarytenoideous dorsalis muscle and the distant peroneal nerve and cranial tibial muscle in the same dogs. Additionally, no previous studies have reported histopathologic results from biopsies of the recurrent laryngeal nerve and peroneal nerve and cricoarytenoideous dorsalis muscle and cranial tibial muscle in combination with electrodiagnostic results for more than one dog. Eleven mature client-owned dogs that presented to the University of Tennessee Veterinary Teaching Hospital for treatment of laryngeal paralysis were enrolled in the study. Consent for procedures performed was obtained from each of the dog’s owners. Eight of the dogs were Labrador retrievers, two were mixed breed dogs, and one was a Brittany spaniel. Seven of the dogs were spayed females, three were neutered males and one was an intact male. Average age of the dogs was 12.5 years. The average weight was 30.1 kg. A thorough physical examination, neurologic examination, complete blood count (CBC), and serum biochemistry profile were performed on all eleven dogs. Measurement of tibial/sciatic and/or ulnar motor nerve conduction studies were performed in six of the eleven dogs. The amplitudes of proximal and distal-evoked compound muscle action potentials (CMAP) were measured. Nine of the eleven dogs had a unilateral cricoarytenoid cartilage lateralization procedure. Two of the eleven were not treated surgically and were euthanized. Cricoarytenoideous dorsalis and cranial tibial muscle biopsies and recurrent laryngeal and peroneal nerve biopsies were collected from each patient at the time of surgery or immediately after euthanasia by the same surgeon. The AVSTS meeting October 2009 Non-cardiac thoracic surgery P a g e | 36 cricoarytenoideous dorsalis muscle and muscular branch of recurrent laryngeal nerve biopsies were obtained through the incision used for cricoarytenoid cartilage lateralization procedure. The cranial tibial and peroneal nerve biopsies were harvested from the lateral surface of the rear limb distal to the stifle. All nine dogs undergoing surgery were followed until the time of death or for a minimum of sixteen months. Follow-up information on eight of the nine survivors was obtained by physical examination or by telephone interview; one dog was lost to follow-up. Non-respiratory abnormalities were identified on physical examination in four of the dogs and included generalized weakness (1), decreased conscious proprioception of the pelvic limbs (1), pelvic limb hyporeflexia (2), and difficulty rising (1). Difficulty rising was noted in the history of five other dogs but was not noted on physical examination. CBC and serum biochemistry profiles were performed on every dog; no consistent abnormalities were present. Tibial nerve conduction velocity (NCV) was determined in six dogs. Mean + standard deviation (S.D.) sciatic/tibial nerve motor NCV was 40.8 + 5.5 meters/second (reference range 59-69 meters/second). CMAP amplitudes were reduced, and CMAP durations were prolonged as a result of stimulating the sciatic/tibial and ulnar nerves at both proximal and distal sites. Muscle specimens were evaluated in paraffin-embedded sections. In all eleven cases, combinations of large and small grouped atrophy were observed in laryngeal and cranial tibial muscle specimens with varying degrees of severity. Concurrent with this pattern of muscle fiber atrophy, large nerve fiber loss, axonal degeneration, and endoneurial fibrosis were consistently identified. Mixed axonal degeneration and demyelination was found in two cases. Regenerative changes were not observed. A specific cause for axonal degeneration could not be identified from the muscle and nerve specimens. In the nine surviving dogs, clinical signs which developed between surgery and the time of followup or death included dysphagia (2), megaesophagus (1), lower motor neuron tetraparesis (1), pelvic limb hyporeflexia (1), decreased conscious proprioception of the thoracic limbs (1), and decreased conscious proprioception in the pelvic limbs (2). Six of the eleven patients were euthanized or died within fifteen months of diagnosis. REFERENCES 1. Jackson AM, Tobias K, Long C, et al: Effect of various anesthetic agents on laryngeal motion during laryngoscopy in normal dogs. Vet Surg 33:102-106, 2004. 2. Lahue TR: Treatment of laryngeal paralysis in dogs by unilateral cricoarytenoid laryngoplasty. J Am Anim Hosp Assoc 25:317-324, 1989. 3. MacPhail CM, Monnet E: Outcome of and postoperative complications in dogs undergoing surgical treatment of laryngeal paralysis: 140 cases (1985-1998). J Am Vet Med Assoc 218:1949-1955, 2001. 4. White RAS: Unilateral arytenoid lateralisation: An assessment of technique and long-term results in 62 dogs with laryngeal paralysis. J Small Anim Pract 30:543-549, 1989. AVSTS meeting October 2009 Non-cardiac thoracic surgery