Introduction
advertisement

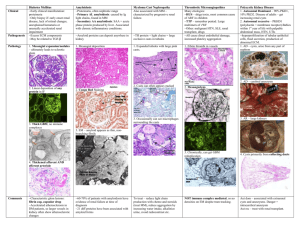
Glomerulopathies Associated with Multisystem Diseases Jinn-Yuh Guh, M.D. Case A 38 y/o female p’t with DM for 15 years has blurred vision, both limbs numbness, intermittent claudication, foot ulcer, edema, residual urine, nephritic syndrome, hypertension, Blood: glucose 350 mg/dl, HbA1C 8.0, creatinine 1.8 mg/dl. What is your Dx? What would you do? Introduction Secondary GN Dx: Clinical syndromePathologic featuresSpecific diseases Diabetic Nephropathy (DN) Introduction The leading cause of ESRD in USA and 2nd most common cause of ESRD in Taiwan (2nd only to chronic GN) Occurs in 30% of IDDM and 20% of NIDDM p'ts, but most diabetic ESRD p'ts have NIDDM Clinical & morphologic features of DN are similar in IDDM & NIDDM Clinical staging Hyperfiltration Glomerular hypertension Renal hypertrophy Silent 2-3rd year Thick GBM Mesangial expansion Incipient (microalbumiuria) 7-15th year Urinary albumin excretion=30-300 mg/day=30-300 mg/g creatinine=20-200 g/min (Avoid exercise, UTI, other diseases) >2/3 within 3 months "Point of no return" beyond this stage! Overt (clinical proteinuria) 10-20th year Dipstick + proteinuria With or without nephrotic syndrome Hypertension Progressive GFR Normal sized kidneys D.D. of CRF with normal sized kidneys DM, polycystic kidneys, amyloidosis, obstructive uropathy, multiple myeloma Retinopathy (90% in IDDM, 60% in NIDDM) Bland urinary sediment 1 Renal failure (end-stage renal disease) Dialysis is indicated at an earlier stage (serum creatinine 6 mg/dl) than the other uremic p'ts Pathology Nodular glomerulosclerosis (Kimmelstiel-Wilson lesion) Classic lesion for DN Thick GBM IgG linear deposition along GBM Wide mesangium Hypertensive nephrosclerosis Treatment 1. Glycemic control Less effective beyond stage 3 2. Blood pressure control Goal is BP<125/75 mmHg 3. Angiotensin-converting enzyme inhibitor Inhibiting angiotensin II Proteinuria Retard progression of GFR Efferent arteriole resistance Intraglomerular hypertension Glomerular cell growth Mesangial matrix Glomerulosclerosis Indicated for DM p'ts normotensive or hypertensive with greater than microalbuminuria stage 4. Low protein diet 0.6-0.8 g/kg/day 5. Renal replacement therapy Introduction Diabetic ESRD p'ts has higher mortality than the other uremic p'ts HD and CAPD has similar survival rates Hemodialysis (HD) Continuous ambulatory peritoneal dialysis (CAPD) Renal transplantation The preferred treatment Case A 30 y/o female p’t has malar rash, polyarthritis, edema, oliguria, ANA+, anti-DsDNA+, hypertension, Blood: creatinine 1.6 mg/dl (1 month ago)6 mg/dl (now); Urine: protein 6 g/day, RBC casts+, WBC 10-15/HPF What is your Dx? What would you do? Immunologically Mediated Multisystem Diseases Vasculitis Large vessel Takayasu's disease & giant cell arteritis Glomerular injury is exceedingly rare Classic polyarteritis nodosa Proteinuria, hypertension, CRF 2 Bland urinary sediment Normal serum complement ANCA (antineutrophil cytoplasmic antibody) negative Rx If untreated, 5-year survival 10% Glucocorticoids & cyclophosphamide5-year survival 80% ANCA-associated small-vessel vasculitis ANCA May also be positive (in low titers) in other diseases Anti-GBM disease, inflammatory bowel disease, primary biliary cirrhosis, some autoimmune disorders Pathogenic role is not clear The correlation between titer and disease activity is not good Classification 1. Wegener's granulomatosis Renal injury in 80% p'ts Rarely recurs in renal transplants 2. Microscopic polyarteritis Plasmapheresis may be effective for severe RPGN and lung hemorrhage 3. Churg-Strauss syndrome Renal injury is rare and mild Granulomatous vasculitis Necrotizing GN is rare 4. Pauci-immune renal-limited GN Clinical features Elderly Viral-like prodrome Nonspecific constitutional symptoms BW loss, fatigue, fever, arthralgia, myalgia Nonspecific laboratory findings ESR & CRP, leukocytosis, thrmbocytosis, normocytic anemia Normal serum complement Nephritic syndrome or RPGN Pathology "Pauci-immune GN" Focal, segmental necrotizing crescentic GN Treatment Corticosteroids and cyclophosphamide If adequately treated, 5-year survival>75% Henoch-Schönlein purpura GN occurs in 80% p'ts May be the different manifestation of IgA nephropathy Treatment Supportive Prognosis Exacerbations and remissions within 1st yearLong-term remission CRF & hypertension <10% p'ts 3 Essential mixed cryoglobulinemia (EMC) Mixed cryoglobulinemia Type II Polyclonal IgG + monoclonal IgM Type III Polyclonal IgG + polyclonal IgM Clinical features More common in females, mean age of onset 60 years Clinical features Triad (purpura, arthralgia, fatigue), Raynaud's phenomenon RA factor + Renal disease occurs in 50% p'ts Nephrotic syndrome, hematuria, hypertension Rarely (20-30%) nephritic syndrome 5% RPGN Hypocomplementemia (esp.C4) Chronic liver disease (15-50% p'ts) Anti-HCV +, HCV-RNA + Pathology Mesangial proliferative GN or MPGN Pseudothrombi in glomerular capillaries Granular depositions EM: Subendothelial deposits with "thumbprints" Treatment Glucocorticoids & cyclophosphamide Plasmapheresis -interferon Systemic lupus erythematosus (SLE) Introduction Clinical renal disease (Lupus nephritis) in 40-85% p'ts, but pathologic abnormalities may occur without clinical manifestations All syndromes in nephrology can be found! Immune complex-mediated lupus nephritis Clinical features Urinalysis: “telescoped urine” (simultaneous presence of nephritic, nephrotic, acute renal failure and chronic renal failure sediments) Hypocomplementemia ANA (95-99%), anti-DsDNA (highly specific), anti-Sm Ab (17-30%, highly specific) WHO classification Introduction Interstitial changes are mainly seen in Class III & IV Weak correlation between pathologic classifications and clinical features Class I (Normal) Normal in LM (light microscope) Occasional deposits in IF (immunofluorescence) Clinically silent 4 Class II (Mesangial) Classification Class IIA Normal mesangial cellularity Class IIB Mesangial hypercellularity Mesangial deposits in IF Hematuria, mild to moderate proteinuria Class III (Focal segmental proliferative) Necrosis and sclerosis <50% of glomeruli Rarely nephrotic syndrome (1/3 p'ts) or renal failure (15-25% p'ts) Class IV (Diffuse proliferative) Clinical features The most aggressive lupus nephritis! "Telescoped urine" Nephritic + nephrotic + chronic GN >50% p'ts have nephrotic syndrome and renal failure 30% p'ts progress to ESRD Pathology LM Often with crescents, fibrinoid necrosis, wire-loops (GBM thickening, mesangial interposition) IF Widely positive EM (electron microscope) Mesangial, sub-endothelial and subepithelial deposits Tubuloreticular structures in endothelial cells Also seen in HIV nephropathy "Thumbprinting" similar to EMC Class V (Membranous) 90% p'ts have nephrotic syndrome Rarely (10%) has renal failure Class VI (Diffuse glomerulosclerosis) Plus advanced tubulointerstitial disease Clinical features The end stage of lupus nephritis Renal failure Hypertension Nephrotic syndrome Transformation between classes is common Additional pathologic features useful for deciding Rx Activity index Endocapillary proliferation, glomerular leukocyte infiltration, wire loops, cellular crescents, interstitial inflammation Chronicity index Glomerulosclerosis, fibrous crescents, tubular atrophy, interstitial fibrosis Treatment Introduction 5 Treat the p't, NOT ONLY the kidneys Depends on clinical activity and pathologic features! Class I & II Rx is not indicated, but may be used for extrarenal manifestations Classs III & IV Glucocorticoids Pulse therapy is indicated in severe cases Cyclophosphamide Pulse therapy is indicated in severe cases Monthly pulses x 6 monthsPulses every 3-6 monthsTotal treatment period 18-24 months Corticosteroids are used concomitantly & tapered Plasmapheresis is NOT indicated Renal replacement therapy P'ts may become clinically silent durine ESRD Renal transplantation Lupus GN rarely recurs in allografts Graft survival is comparable to other p'ts Prognosis Introduction Follow-up with urine sediment, proteinuria, GFR, serum complement, anti-DsDNA lelvels Class III & IV If adequately treated, 5-year suvival=60-90% Class V 1/2 spontaneous remission 5-year survival=70-90 % Antiphospholipid syndrome and thrombotic microangiopathy Intravascular microthrombi and endothelial swelling (interlobular arteries, arterioles, glomerular capillaries) Tissue plasminogen activator 2--antiplasmin Treatment Plasmapheresis (?) Rheumatoid arthritis (RA) Classification 1. Direct renal involvement Rare 2. AA amyloidosis Esp. duration>10 years, RA factor +, destructive arthropathy 10-20% RA p'ts, 其中只有 3-10%有 GN Nephrotic syndrome Renal failure 3. Drug-induced Gold & penicillamine Nephrotic syndrome (membranous GN) NSAID Minimal change disease Acute interstitial nephritis 6 Sjögren's syndrome Tubulointerstitial diseases Fanconi's syndrome Distal renal tubular acidosis Impaired urinary concentrating ability GN is rare Polymyositis and dermatomyositis Occasionally mesangial proliferative GN Mixed connective tissue disease (MCTD) SLE+scleroderma+polymyositis Antiribonucleoprotein + GN is rare (<15%) Hematuria & proteinuria Membranous GN or MPGN Treatment Glucocorticoids for rare p'ts with progressive disease Prognosis Excellent Glomerular Deposition Diseases Amyloidosis Classification Primary Elderly Secondary Chronic inflammation (RA, paraplegia, osteomyelitis), multiple myeloma, cancers, hereditary (FMF) 1. AL (Primary, immunoglobulin light chain) 2. AA (Secondary, serum amyloid A) 3. Dialysis-associated (2-microglobulin) 4. Alzheimer's disease & Down's syndrome (amyloid protein) Diagnosis Rectal biopsy or abdominal fat pad biopsy Congo red + Apple-green birefringence under polarized light Renal involvement AA & AL amyloidosis (75-90%) Nephrotic syndrome 50% p'ts have renal failure Tubulointerstitial disease is rare 20-25% p'ts have hypertension Normal-sized kidneys even in CRF! Pathology LM: Mesangial amorphous (nodular) deposits, tubulointerstitial or vascular deposits IF: Weakly positive for immunoglobulin light chains (variable region) EM: Amyloid fibrils (7.5-10 nm) Treatment Melphalan & prednisolone Eradicate underlying disease for AA amyloidosis 7 Colchicine for familial Mediterranean fever (FMF) Dialysis Lower survival than the other uremic p'ts Renal transplantation Recurrence in allograft is common but rarely leads to graft loss Prognosis Poor ESRD within 2-5 years Died of cardiovascular diseases Light chain deposition disease (with or without multiple myeloma) Clinical features Renal involvement in 90% p'ts Nephrotic syndrome & renal failure Tubular abnormalities may be seen Pathology Tubular basement membrane thickening Mesangial expansion & nodular glomerulosclerosis (33%) Similar to diabetic nephropathy & MPGN Strongly positive for immunoglobulin light chains (constant region) EM: Granular rather than fibrillar deposits Treatment Melphalan & prednisolone (?) Prognosis Poor if with multiple myeloma (ERSD rapidly) Waldenström's macroglobulinemia Monoclonal proliferation of IgM-plasma cells Hyperviscosity syndrome Renal failure Direct renal involvement is rare (deposits in glomerular capillaries) Renal amyloidosis Drug-Induced Glomerular Disease NSAID 1. Acute renal failure a. Hemodynamic b. Acute interstitial nephritis Nephrotic syndrome Most common with propionic acid NSAIDs, but also occurs in ampicillin, rifampicin, interferon Stopping drugs leads to remission 2. Papillary necrosis 3. Fluid & electrolyte disturbances Salt & water retention Edema Hypertension Hyponatremia Hyperkalemia Gold (for RA Rx.) Proteinuria after 4-6 months of therapy (5-25%) 8 Nephrotic syndrome (33%) Membranous nephropathy Rarely progressive renal failure Withdrawal of the drug leads to remission Penicillamine Proteinuria (5-30%) Membranous nephropathy Withdrawal of the drug leads to remission I.V. heroin abuse More common in blacks Focal & segmental glomerulosclerosis Nephrotic syndrome, renal failure, hypertension, ESRD within 3-5 years Hereditary Diseases with Glomerular Involvement Alport's syndrome X-linked dominant trait Rarely autosomal recessive inheritance Genetic defect in5 chain of type IV collagen on long arm of X chromosome which is a major component of GBM Clinical features Hematuria, proteinuria, nephrotic syndrome (30%), progressive renal failure Sensorineural hearing loss (60%) Bilateral anterior lenticonus (15-30%) Mild in female carriers Pathology LM: mesangial hypercellularity, FGS, foam cells, tubulointerstitial fibrosis EM: Thickening, fragmentation and lamellation of GBM (lamella densa), patchy thinning of GBM Prognosis Males progress to ESRD Anti-GBM disease occurs in 5% p'ts after renal transplantation Sickle cell disease Exceedingly rare in Taiwan Fabry's disease Clinical features X-linked recessive trait Hematuria, proteinuria, nephrotic syndrome, progressive renal failure Angiokeratoma of skin, corneal and lens opacities, etc. Diagnosis Urinary glycoshingolipids Leukocyte-galactosidase Pathology Accumulation of neutral glycosphingolipids EM "Myeloid bodies" Nail-patella syndrome 9 Rare AD inheritance 50% nephropathy (hematuria & proteinuria) Rarely (10%) progress to ESRD Lipodystrophy Females (5-15 years old) MPGN type II (80%), type I (20%) Low C3 levels Lecithin-cholesterol acyltransferase (LCAT) deficiency TG Proteinuria, hematuria, progressive renal failure FGS Infectious Diseases Viral infections HBV Chronic persistent or chronic active hepatitis 1. Membranous nephropathy Good prognosis in children 2/3 spontaneous remission within 3 years Poor prognosis in adults 30% progressive renal failure, 10% to ESRD 2. MPGN 3. IgA nephropathy 4. Essential mixed cryoglobulinemia 5. Polyarteritis nodosa HCV It should be considered in all p'ts with cryoglobulinemic proliferative GN, MPGN & membranopus nephropathy Treatment Glucocorticoids, cytotoxics, plasmapheresis (?) -interferon Usually relapse after drug withdrawal HIV FGS (HIV-associated nephropathy) Clinical features More common in blacks Nephrotic syndrome Rapidly progress to ESRD within weeks to months EM Tubuloreticular structures (glomerular endothelial and tubular cells), leukocyte infiltration, degeneration of tubular nuclei Bacterial infections Infective endocarditis Clinical features Hematuria, proteinuria, nephrotic syndrome (25%), pyuria, mild renal failure RA factor (10-70%) Hypocomplementemia Pathology Immmune-complex GN (Focal proliferative GN) 10 Embolic renal infarction Septic abscesses ATN (acute tubular necrosis) DIC (diffuse intravascular coagulation) Acute interstitial nephritis (drug-induced) Rarely crescents Prognosis Good, resolve with eradication of underlying disease Infected ventriculoatrial shunt 1-4% p'ts have immune-complex GN Hematuria, proteinuria, nephrotic syndrome (50%) MPGN or diffuse proliferative GN Prognosis 1/3 has residual renal failure despite eradication of underlying disease Suppurative infections Abscesses (thoracic, abdominal, dental), osteomyelitis Hematuria, proteinuria, acute renal failure Syphilis 0.3% p'ts have nephrotic syndrome Membranous nephropathy with mild cellular proliferation Leprosy AA amyloidosis aGN (like PSGN) Protozoan and parasitic infections Plasmodium (malaria) Eradication of infection does NOT consistently induce remission of nephrotic syndrome Schistosoma mansoni 5-10% p'ts have nephrotic syndrome Filariasis Loa loa & Oncocerca volvulus Congenital Toxoplasmosis Hydatid disease Trichinosis Neoplasia Solid organs Membranous nephropathy Hodgkin's lymphoma Minimal change disease Non-Hodgkin's lymphoma Leukemias GN is rare Paraproteinemia Classification 1. Primary amyloidosis 2. Light chain deposition disease 3. Multiple myeloma Secondary amyloidosis (10-15%) Light chain nephropathy 11 Myeloma kidney Fracturing tubular casts (Bence-Jones proteinuria) Fanconi’s syndrome Acute renal failure & CRF 4. Cryoglobulinemia 5. Fibrillary/immunotactoid GN Prognosis Usually remits after treating underlying disease Summary Hypocomplementemia MPGN, SLE, EMC, infectious endocarditis, lipodystrophy 12