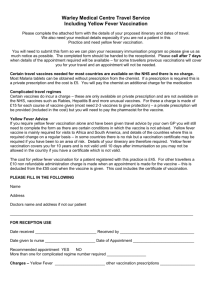
הודעה על החמרה ( מידע בטיחות) בעלון לצרכן
advertisement
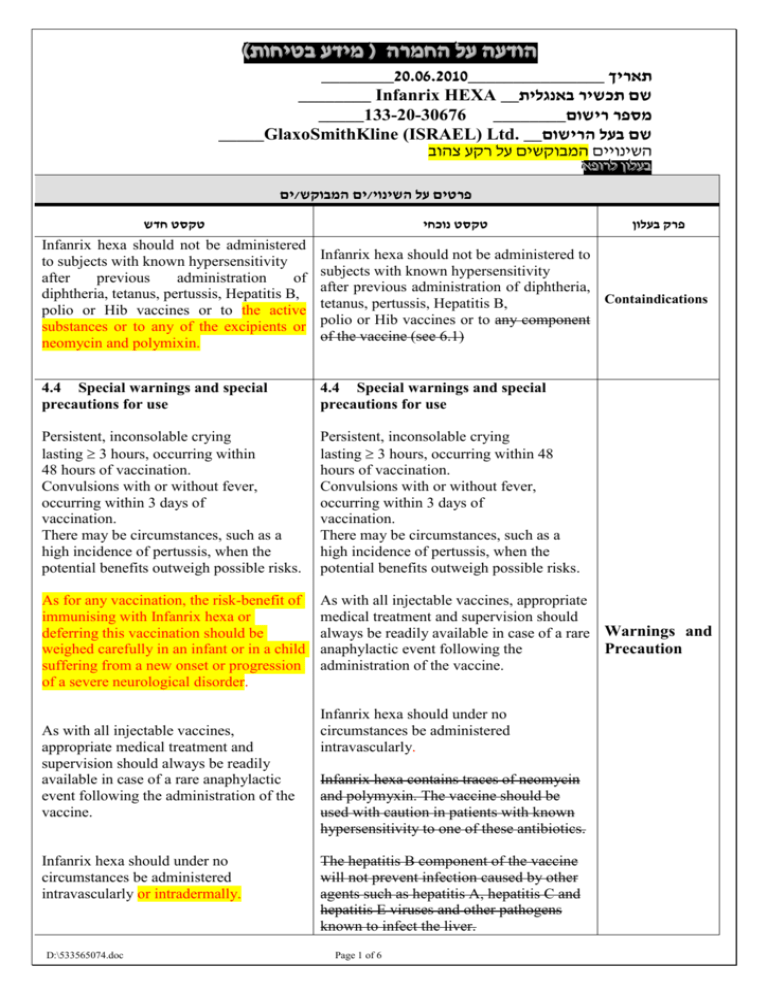
)בטיחות )מידע בטיחות החמרה (( מידע על החמרה הודעה על הודעה ________0262.60202_______________ תאריך ________ Infanrix HEXA __שם תכשיר באנגלית _____133-20-30676 ________מספר רישום _____GlaxoSmithKline (ISRAEL) Ltd. __שם בעל הרישום השינויים המבוקשים על רקע צהוב לרופא בעלון לרופא בעלון ים/ים המבוקש/פרטים על השינוי טקסט חדש טקסט נוכחי פרק בעלון Infanrix hexa should not be administered to subjects with known hypersensitivity after previous administration of diphtheria, tetanus, pertussis, Hepatitis B, polio or Hib vaccines or to the active substances or to any of the excipients or neomycin and polymixin. Infanrix hexa should not be administered to subjects with known hypersensitivity after previous administration of diphtheria, Containdications tetanus, pertussis, Hepatitis B, polio or Hib vaccines or to any component of the vaccine (see 6.1) 4.4 Special warnings and special precautions for use 4.4 Special warnings and special precautions for use Persistent, inconsolable crying lasting 3 hours, occurring within 48 hours of vaccination. Convulsions with or without fever, occurring within 3 days of vaccination. There may be circumstances, such as a high incidence of pertussis, when the potential benefits outweigh possible risks. Persistent, inconsolable crying lasting 3 hours, occurring within 48 hours of vaccination. Convulsions with or without fever, occurring within 3 days of vaccination. There may be circumstances, such as a high incidence of pertussis, when the potential benefits outweigh possible risks. As for any vaccination, the risk-benefit of immunising with Infanrix hexa or deferring this vaccination should be weighed carefully in an infant or in a child suffering from a new onset or progression of a severe neurological disorder. As with all injectable vaccines, appropriate medical treatment and supervision should always be readily available in case of a rare Warnings and Precaution anaphylactic event following the administration of the vaccine. As with all injectable vaccines, appropriate medical treatment and supervision should always be readily available in case of a rare anaphylactic event following the administration of the vaccine. Infanrix hexa should under no circumstances be administered intravascularly or intradermally. D:\533565074.doc Infanrix hexa should under no circumstances be administered intravascularly. Infanrix hexa contains traces of neomycin and polymyxin. The vaccine should be used with caution in patients with known hypersensitivity to one of these antibiotics. The hepatitis B component of the vaccine will not prevent infection caused by other agents such as hepatitis A, hepatitis C and hepatitis E viruses and other pathogens known to infect the liver. Page 1 of 6 Infanrix hexa will not prevent disease caused by pathogens other than Corynebacterium diphtheriae, Clostridium tetani, Bordetella pertussis, hepatitis B virus, poliovirus or Haemophilus influenzae type b. However, it can be expected that hepatitis D will be prevented by immunisation as hepatitis D (caused by the delta agent) does not occur in the absence of hepatitis B infection. As with any vaccine, a protective immune response may not be elicited in all vaccinees (see section 5.1). A history of febrile convulsions requires special attention. A family history of convulsions or a family history of Sudden Infant Death Syndrome (SIDS) does not constitute a contra-indication. Vaccines with a history of febrile convulsions should be closely followed up as such adverse events may occur within 2 to 3 days post vaccination. The Hib component of the vaccine does not protect against diseases due to other capsular serotypes than type b of Haemophilus influenzae or against meningitis caused by other organisms. A history of febrile convulsions requires special attention. A family history of convulsions or a family history of Sudden Infant Death Syndrome (SIDS) does not constitute a contra-indication. HIV infection is not considered as a contraindication. The expected immunological response may not be obtained after vaccination of immunosuppressed patients. Excretion of capsular polysaccharide antigen in the urine has been described following receipt of Hib vaccines, and therefore antigen detection may not have a diagnostic value in suspected Hib disease within 1-2 weeks of vaccination. HIV infection is not considered as a contra-indication. The expected immunological response may not be obtained after vaccination of immunosuppressed patients. Since the Hib capsular polysaccharide antigen is excreted in the urine, a positive urine test can be observed within 1-2 weeks following vaccination. Other tests should be performed in order to confirm Hib infection during this period. Antipyretic treatment should be initiated according to local treatment guidelines. Limited data in 169 premature infants indicate that Infanrix hexa can be given to premature children. However, a lower immune response may be observed and the level of clinical protection remains unknown. The potential risk of apnoea and the need for respiratory monitoring for 48-72h should be considered when administering the primary immunisation series to very D:\533565074.doc Page 2 of 6 premature infants (born ≤ 28 weeks of gestation) and particularly for those with a previous history of respiratory immaturity. As the benefit of the vaccination is high in this group of infants, vaccination should not be withheld or delayed. Clinical trials on primary vaccination: Clinical trials: The safety profile presented below is based on data from more than 16,000 subjects. As has been observed for DTPa and DTPa-containing combinations, an increase in local reactogenicity and fever was reported after booster vaccination with Infanrix hexa with respect to the primary course. Tabulated summary of adverse reactions (clinical trials): Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness. Frequencies per dose are defined as follows: Very common: Common: Uncommon: Rare: Very rare: (≥1/10) (≥1/100 to <1/10) (≥1/1,000 to <1/100) (≥1/10,000 to <1/1,000) (<1/10,000) Nervous system disorders: Uncommon: somnolence Very rare: convulsions (with or without fever) Respiratory, thoracic and mediastinal disorders Uncommon: cough Gastrointestinal disorders: Common: diarrhoea, vomiting Skin and subcutaneous tissue disorders Rare: rash D:\533565074.doc Clinical trials involved the administration of over 13,500 doses of Infanrix hexa to 4,590 healthy infants from 6 weeks of age as primary vaccination. In two large randomised controlled studies, infants were enrolled to receive a three dose primary series of Infanrix hexa (N=2121) or separate injections of commercially-available DTPa-IPV/Hib and hepatitis B (HBV) vaccines given simultaneously at separate sites (N=708). In these trials, Infanrix hexa was shown to be as safe as the licensed vaccines. For both groups, solicited local reactions were reported in 54 to 70% of subjects. In the study where measurement of temperature was specifically requested, fever of >39.5°C was reported for 1.4% of infants administered Infanrix hexa; fever of >40°C was reported for 0.2% (values for infants Undesirable administered licensed vaccines were effects respectively 1.6% and 0%). No increase in the incidence or severity of these undesirable events was seen with subsequent doses of the primary vaccination series. In a smaller randomised comparative trial, severe undesirable events after Infanrix hexa were reported with a lower frequency as compared to a commercial diphtheria, tetanus, pertussis (DTP) whole cell vaccine. Clinical trials on booster vaccination: A total of 2,358 infants 12 to 24 months of age received a booster dose of Infanrix hexa; 1,220 of these subjects received Infanrix hexa for both the primary and booster doses (for a total of 4 doses of vaccine). Page 3 of 6 Very rare: dermatitis As has been observed for DTPa and DTPacontaining combinations, an increase in reactogenicity was reported after booster vaccination with Infanrix hexa with respect General disorders and administration site to the primary course; however, the incidence of symptoms graded as severe conditions: was low. Very common: fever 38°C, local Oedematous swelling, occasionally leading swelling at the injection site (≤ 50 mm), to an increased circumference of the fatigue, pain, redness injected limb, has been observed in clinical Common: fever >39.5°C, injection site trials evaluating booster doses of Infanrix reactions, including induration, local swelling at the injection site (> 50 mm)*, hexa at an incidence of 2.3% when solicited. injection site reaction All these reactions resolved without Uncommon: diffuse swelling of the sequelae. injected limb, sometimes involving the adjacent joint* Irrespective of the vaccine used for the primary course, fever >39.5°C was Psychiatric disorders: reported for overall 3.3% of infants Very common: crying abnormal, administered Infanrix hexa as a booster irritability, restlessness dose. The incidence of fever >39.5°C in a Common: nervousness control group of infants boosted with commercially-available DTPa-IPV/Hib + Post marketing surveillance: HBV vaccines was 2.9%. The incidences of fever > 40°C were respectively 0.9% for Blood and lymphatic system disorders Infanrix hexa and 0.8% for the licensed Lymphadenopathy vaccines. Nervous system disorders: Collapse or shock-like state (hypotonic- In a randomised comparative trial, infants primed with Infanrix hexa were boosted hyporesponsiveness episode) with the same vaccine (N = 543) or received a booster dose with commercially Respiratory, thoracic and mediastinal available DTPa-IPV/Hib (with or without disorders: HBV administered separately at a different Apnoea [see section 4.4 for apnoea in site) (N = 331). The incidences of the very premature infants (≤ 28 weeks of solicited general and local symptoms gestation)] following the booster dose were similar in both groups. Fever of >39.5°C was Skin and subcutaneous tissue disorders reported for 3.5% of infants administered Angioedema Infanrix hexa; fever of >40°C was reported General disorders and administration site for 0.7% (values for infants administered licensed vaccines were respectively 3.6% conditions: and 0.9%). Swelling of the entire injected limb*, extensive swelling reactions, injection site Post marketing surveillance: mass, injection site vesicles Metabolism and nutrition disorders Very common: appetite lost Immune system disorders Anaphylactic reactions, anaphylactoid reactions (including urticaria), allergic reactions (including pruritus) During post marketing surveillance, other reactions have been reported in temporal association with Infanrix hexa. None of the reactions were reported with a frequency higher than 0.01%. * Children primed with acellular pertussis vaccines are more likely to experience swelling reactions after booster D:\533565074.doc Tabulated summary of undesirable effects: Page 4 of 6 administration in comparison with children primed with whole cell vaccines. Undesirable effects reported in clinical These reactions resolve over an average of trials (following primary immunisation or booster dose) or reported during post 4 days. marketing surveillance are listed here Experience with hepatitis B vaccine: below per system organ class. For those symptoms reported both during clinical trials and during PMS, invariably the In extremely rare cases, paralysis, highest frequencies were under controlled neuropathy, Guillain-Barré syndrome, clinical trial conditions. encephalopathy, encephalitis and meningitis have been reported. The causal Frequencies are defined as follows: relationship to the vaccine has not been established. 10% Thrombocytopenia has been reported with Very common: Common: 1% and < 10% hepatitis B vaccines. Uncommon: 0.1% and < 1% Rare: 0.01% and < 0.1% Very rare: < 0.01% Application site very common: pain, redness, swelling, peripheral oedema common: injection site reaction very rare: injection site mass*, extensive swelling reaction* Body as a whole very common: fever 38C common: abnormal crying, restlessness uncommon: fatigue very rare: allergic reactions (including rash* and angiooedema), anaphylactoid reactions (including urticaria)* Gastro-intestinal system very common: loss of appetite common: diarrhoea, enteritis, gastroenteritis uncommon: abdominal pain, vomiting, constipation Neurological disorders very rare: convulsions (with or without fever)*, collapse or shock-like state (hypotonic-hyporesponsiveness episode)* Psychiatric very common: drowsiness, irritability uncommon: somnolence Resistance mechanism common: viral infection, moniliasis, otitis D:\533565074.doc Page 5 of 6 media uncommon: infection Respiratory system common: upper respiratory tract infection, bronchitis, coughing, rhinitis, pharynigitis uncommon: bronchospasm, laryngitis, stridor Skin and appendages common: rash erythematous, dermatitis uncommon: eczema very rare: pruritus* Vision common: conjunctivitis * Reported only during post-marketing surveillance Experience with hepatitis B vaccine: Nearly 100 million doses of Engerix B 10 µg, GlaxoSmithKline Biologicals’ hepatitis B vaccine, have been distributed for infants < 2 years old. In extremely rare cases, paralysis, neuropathy, Guillain-Barré syndrome, encephalopathy, encephalitis and meningitis have been reported. The causal relationship to the vaccine has not been established. Thrombocytopenia has been reported very rarely with hepatitis B vaccines. D:\533565074.doc Page 6 of 6