CHS MANUSCRIPT PROPOSAL FORM

Template date April 16, 2008
C H S M A N U S C R I P T P R O P O S A L F O R M
Please review CHS P&P Committee protocol at www.chs-nhlbi.org
before completing this form. Send completed form to: Erika Enright, P&P Coordinator ( eenright@u.washington.edu
).
Part I: Basic Information and Checklist of Key Components
1. Date of submission: 11-1-2008
2. Proposal Title: Multi-state life tables, Markov models, equilibrium and selection bias in CHS
3. Writing Chair Name and Contact information: Paula Diehr, pdiehr@u.washington.edu
4. CHS Sponsor Name (NB: if this is your first CHS proposal, please include a brief letter of introduction from your Sponsor): Paula Diehr
5. Co-author names and email addresses (the Steering Committee may nominate additional authors if special expertise for interpreting CHS data is needed): David Yanez
6. Have all co-authors reviewed and approved this document? (required): Yes
7. Does this proposal derive from a CHS Working Group? (if yes, please name group): No
8. Please confirm that you have reviewed the internal CHS website for potential areas of overlap. If you see a paper(s) that may overlap, please list along with any plans for addressing this: Yes
9. Type of study (Main, Ancillary, Meta-analysis/Pooled): Main
(If not a Main CHS data analysis, please list Ancillary Study or Collaborative Group title and name of
PI. A list of all CHS Ancillary Studies can be found on the internal CHS website):
10. Type of data (Events, Longitudinal or Cross-sectional): Longidutinal including events
11. Who/what group will do the analysis (if local)? Diehr and Yanez
12. Funding: Do you plan to request any Coordinating Center services in conjunction with this paper?
(Note that a “yes” answer to this question will result in an invoice for services unless other arrangements are made.) No. a. If no, how do you plan to obtain CHS Data? Diehr and Yanez are CHS investigators, will extract necessary data themselves. b. If yes, please check all services that apply:
_____ Sample Selection
_____ Dataset preparation
_____ Central analysis by a CC statistician
_____ Verification of analyses
_____ Arranged consultation c. If yes to above, please check one:
_____ I have funding (please indicate source):
_____ I am applying for funding (requires completion of CHS Ancillary Study Proposal Form).
Template date April 16, 2008
13. Keywords: (Please see suggested keyword list on CHS website. If you answer yes to question #13a, below, please include “genetic factors” as one of the keywords): multi-state life table, markov, equilibrium, steady state, selection bias
14. Genetic Information: a. Do you propose use of data from a participant’s DNA? No b. If yes, for a primary aim of CHS? (includes heart, vascular disease or dementia): c. If yes, please confirm that you will use our variable “gencons” to exclude participants who did not give consent for use of their DNA, whether for primary or for secondary aims:
15. Conflict of Interest: a. Do you or any member of your Writing Group intend to patent any process, aspect or outcome of these analyses? (requires author-funded verification; author-funded central analysis may also apply): No b. Are these analyses to involve a for-profit corporation? (if yes, requires same as above). No c. If yes to above, said involvement will include: (please check one): i. ii.
____ An unrestricted educational or research grant
____ Assistance with hypotheses and/or analyses (requires verification by the
Coordinating Center)
16. Distributed manuscript review: All Writing Chairs are encouraged to participate in the distributed P&P review of penultimate draft manuscripts (1-3 times per year.) Please describe your area of expertise
(eg, genetics, diabetes, statistical methods, etc): biostat and health services, quality of life
PART II: Description (This section must be limited to 3 pages).
1. Introduction [Rationale and background]:
CHS is notable for its extensive longitudinal data, with a few variables measured as many as 19 times, and many more variables measured annually. CHS data are believed to be positively biased at baseline, but perhaps to become more representative of the general population over time. Multi-state life tables
(MSLTs) are a good way to display longitudinal data,
1
but some of the assumptions and potential biases are unclear. CHS longitudinal data will be used to examine and illustrate some of these issues. We will use self-rated health, coded excellent, very good, good, fair, or poor (EVGGFP) which is sometimes recoded as Healthy (E,VG,G) versus Sick (F,P).
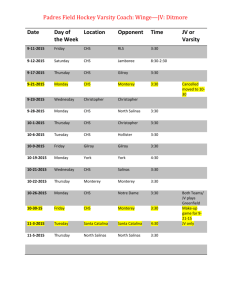
The basis of a CHS multi-state life table is a table of transition probabilities from one state to another in one year. These probabilities can be estimated from the CHS longitudinal data. Probabilities for a 3state system are in Table 1. For a population with a specific initial number of healthy and sick persons, it is easy to calculate the expected number who will be healthy, sick, or dead one year later. For example, about .863*(#healthy)+.272*(#sick) will be healthy one year later.
The assumptions for these calculations are not well understood. It is common to assume that every person in the healthy state has identical transition probabilities, and that every person in the sick state has identical transition probabilities. This is another way of saying that the only relevant information is the state that the person is in, and that prior trajectories have no influence. If this
Template date April 16, 2008 assumption, known as the Markov assumption, holds, knowledge of a person’s state at a particular age would completely determine his transition probabilities; that is, all persons in a given state would have the same transition probabilities. That is unfortunately not the case. For example, healthy 70-year-olds who were also healthy at age 69 have probability 0.91 of being healthy at age 71, compared to a probability of
0.61 for those who were sick at age 69 and healthy at age 70 (data not shown).
Table 1 - Transition Matrix for all years, ages and both sexes combined
% within hsd1_evgr
H
Health After
S Dead
Total
Health
Before
Total
Healthy
Sick
86.3% 11.9%
27.2% 63.7%
71.4% 25.0%
1.7% 100.0%
9.1% 100.0%
3.6% 100.0%
In fact, MSLT calculations can be performed if only the average probability is known, which permits variability of probabilities within a state, and is more reasonable. The average transition probability for each age-specific state is sometimes known as the cohort (rather than the individual) transition probability.
2
For example, suppose the Healthy state at age 70 comprised two sub-states of the same size, one with probability 0.9 of being healthy the following year and one with probability 0.6 of being healthy (similar to the example above). The average transition probability is 0.75, and indeed, 75% are expected to remain healthy at age 71 (90% of group 1 and 60% of group 2), even though not a single person in the population had a transition probability of 0.75. The average transition probability is thus sufficient for this calculation. At age 71, there will no longer be two equal subgroups within the Health state, but the correct average transition probabilities may be estimated from a random sample of 71-yearolds. The average transition probability can be estimated from population data without knowledge of the individual probabilities.
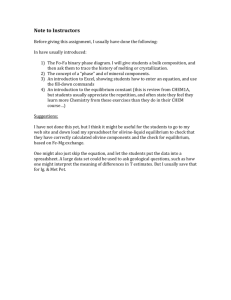
An unspoken assumption is that the average probabilities must be estimated from a population similar to the population at risk; that is, that they are the right probabilities for the state at this time. This assumption can be made more specific by considering the equilibrium or steady-state distribution of the states. (These words are misnomers because at the true equilibrium everyone is dead, but we will use them in this proposal – they are more properly pseudo equilibrium or pseudo-steady-state). Figure 1, calculated from a multi-state life table, demonstrates that no matter where the population starts (all healthy, 80% healthy, all sick in the example), after a while the prevalence of the healthy state is eventually the same. Diehr and Yanez
3
showed that, at equilibrium, the ratio of the number healthy to the number sick was
K
H
S t t
P ( H | H )
P ( S | S )
2 P ( S | H )
[ P ( H
[ 2
| H )
P ( S |
P ( S
H )]
2
| S )]
2
P ( H
P ( S
| S
| H )
)
. {1}
That is, no matter what the initial conditions, H t
/ S t will converge to K. From the probabilities in Table 1,
K= 2.67; that is, after a few years to overcome any initial imbalance, there will always be approximately
2.67 times as many Healthy as Sick persons, until eventually all are dead. The prevalence of the healthy state is K/(1+K) = 2.67/(1+2.67) = 0.73. (Figure 1 was actually based on age-specific probabilities rather than the grouped probabilities seen in Table 1).
Figure 1
Template date April 16, 2008
Template date April 16, 2008
If the population is at equilibrium, and the average probabilities were estimated from an equilibrium population, the average probabilities are sufficient for calculating the MSLT. In CHS, however, persons not expected to be able to participate for three years, or who were institutionalized, using a wheelchair at home, or under treatment for cancer at baseline were ineligible. Only about 59% of those eligible agreed to enroll. A recent CHS paper showed that survival in CHS was considerably better than in comparable persons in Medicare. [ref?] There is thus a strong likelihood of program and selfselection bias at baseline. 4
The baseline data are undoubtedly positively biased, but it seems likely that some of this bias will
“wear off” over time, and that data collected later on may be less biased. Most of the data used to estimate the transition probabilities were collected long after baseline, when the sample should have been at equilibrium. These transition probabilities should be appropriate to create a MSLT for a population that is initially at equilibrium. We propose an approach to estimate the equilibrium distribution in CHS and to compare this to the observed distribution at various survey waves, to determine the extent of bias.
It is the goal of this paper to address some of these issues.
2.
Research Hypothesis:
We hypothesize that CHS baseline data will be out of equilibrium, in the direction of being too healthy. The bias will be worse for older persons than for younger persons, and for sicker persons than for healthy persons. This bias will decrease over time, and that in a few years (perhaps 3 years) after baseline the population will be seen to be in equilibrium. We will try to identify that time, to strengthen the generalizability of some of the analyses that are made using the longitudinal CHS data. Biases in the distribution by age (instead of by calendar time) will be smaller except for ages 65-68, which were estimated based only on early, more biased data.
3.
Data [Variables to be used, sample inclusions/exclusions]:
We will use all of the longitudinal data on EVGGFP and the mortality data. We will use self-rated health, coded excellent, very good, good, fair, or poor (EVGGFP) sometimes recoded into Healthy
(E,VG,G) versus Sick (F,P) and, over time, Dead. Data collected both at clinic and in the later telephone calls will be included.
4.
Brief analysis plan and methods:
Extend formula {1} to calculate the equilibrium prevalences of systems with more than 3 states. This will turn out to be an eigenvector of the transition probability matrix for the living (that is, with the row and the column for death removed).
Estimate the equilibrium distribution for the 6-state EVGGFPD system (the 6 th
state is death), initially for all combined, and later by age and sex. We will calculate the over-all eigenvector using Mathematica.
We will also estimate the over-all equilibrium distribution by repeated applications of equation {1}, which does not require eigenvector calculations, and compare the results to the correct eigenvector result. If the estimates are similar, the following calculations will be performed by this second method.
Compare the observed and equilibrium distributions of EVGGFP, by calendar year, and note at how long it takes for the CHS population to reach equilibrium. We expect baseline to be biased but for the CHS population to reach approximate equilibrium in about 3 years.
Template date April 16, 2008
Perform a similar operation over age (instead of calendar year), separately by sex (and by race if the numbers are sufficient). There should be less bias when age is the measure of time, because age-specific probability estimates will come from many survey waves, not just from the earliest most biased waves. (Estimates for ages 65-68 may be the most biased).
Calculate multi-state life tables (MSLTs), to illustrate the following: i.
If the population starts out in equilibrium, it will be in equilibrium throughout ii.
If the population starts out in disequilibrium (such as all sick, all healthy) equilibrium will not be reached for several years iii.
It will take longer to reach equilibrium if everyone is initially sick. iv.
If everyone is initially healthy, the estimated healthy life expectancy will be underestimated.
Illustrate these points with the 3- and 6-state model, sometimes assuming that the 6-state model is correct (everyone in a state has identical probabilities) but that only the 3-state model can be observed.
Some comparisons will first assume that probabilities do not change by age, and then allow them to change.
5.
Summary/conclusion:
This paper will illustrate that Markov assumptions are not necessary to calculate MSLTs, but rather that using the average state population is sufficient if the population is at equilibrium and the probabilities were calculated at equilibrium. It will also show how far CHS baseline data are out of equilibrium, and how many years of follow-up may be required before equilibrium may be assumed.
6.
References :
1 Diehr P, O’Meara ES, Fitzpatrick A, Newman AB, Kuller L, Burke G. Weight, mortality, years of healthy life and active life expectancy in older adults. J American Geriatric Soc. 2008; 56:76-83.
2 Vaupel JW, Manton KG, Stallard E. The impact of heterogeneity in individual frailty on the dynamics of mortality. Demography 1979; 16:439-454.
3 Diehr P, Yanez D, Derleth A, Newman Anne B. Age-specific prevalence and years of healthy life in a system with 3 health states. Statistics in Medicine 2008; 27:1371-1386
4 Tell GS, Fried LP, Hermanson B et al. Recruitmnet of adults 65 years and older as participants in the
Cardiovascular Health Study: Ann Epidemiol 1993; 3:358-366.