Guidance - Christchurch Infant School
advertisement

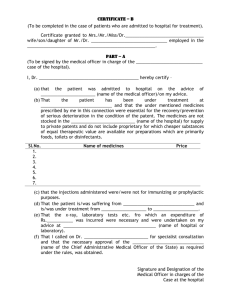
Appendix 5A CHRISTCHURCH INFANT SCHOOL Policy for Supporting Pupils with Medical Needs and Administering Medicines This policy has been structured based upon the guidance provided by information from the Guidance and Code of Practice - First Aid at Work (Issue 2 April 2011) provided by Dorset County Council, guidance from local Health Services, professional teaching associations, Dorset County Council Health and Safety information and the most recent government advice to Schools and Early Years settings. Children with medical needs have the same rights of admission to a school or setting as other children and our school takes all reasonable steps to enable pupils with short and long term medical needs to attend school. Aims 1. To provide clear procedural guidance on the Administering of Medicines and record keeping at Christchurch Infant School 2. To ensure that the children and young people in our school are safe and are able to attend school regularly. 3. To enable children and young people with medical conditions to be included in the school curriculum and other activities. 4. To support children and young people with complex medical conditions and or long term medical needs. Christchurch Infant School will adhere to the advice contained in Managing Medicines in Schools and Early Years Settings – DfES 2005, Multi-Agency Guidance for the Management of Long Term Health Conditions for Children and Young People - DSCB 2011, and Supporting Pupils with Medical Needs – DfEE 1996. The school is mindful of the Dorset For You web document, Medical Advice for Schools and Early Years Settings (found on Schoolsnet). This policy should be read in conjunction with the school’s safeguarding policy and child protection procedures. Short-term medical needs - Most children will, at some time have, short term medical needs perhaps entailing finishing a course of medicine such as antibiotics. To allow children to do this will minimise the time that they need to be absent from school. However such medicines should only be taken where it would be detrimental to a child’s health if it were not administered. Longer term medical needs – these may require medicines on a long-term basis to keep them well, for example children with well-controlled epilepsy or cystic fibrosis. Others may require medicines in particular circumstances, such as children with severe allergies or asthma. Most children with medical needs can attend school or a setting regularly and take part in normal activities, sometimes with some support. However for some pupils with significant needs, staff may need to take extra care in supervising some activities to make sure that these children, and others, are not put at risk. An individual health care plan can help staff identify the necessary safety measures to support children with significant medical needs and ensure that they and others are not put at risk. Such plans are drawn up with parents and relevant health care professionals and more details can be found in DCFS Guidance and from the Inclusion Leader. Arrangements have been made for the following: managing prescription medicines that may need to be taken during the day; managing prescription medicines on trips and outings, including school transport; the safe storage of medicines and accurate record keeping; procedures for access to medicines during emergency situations; adhering to risk management procedures involving medicines. More information can be obtained from the school office. Safeguarding of children is paramount. The Governing Body has a duty under Section 175 (or Section 157, for Academies) of the Education Act 2002 to safeguard and promote the welfare of children in this school. Christchurch Infant School is responsible for adhering to Health Care Plans, maintaining and monitoring records and demonstrating that children are provided with appropriate medical support for which training has been given by qualified personnel. It should be noted that failure to adhere to Health Care Plans could affect insurance cover and increase liability. The school will follow First Aid principles and seek to act in the interest of preserving life when in the event of an emergency. The school will accept written notice from parents / carers that relate to particular medical or religious issues that might affect the manner in which emergency cases are managed. Appropriate / standard forms will be used to support the management and administering of medicines (see ‘Managing Medicines in Schools and Early Years Settings’ DfES 2005 and Multi-Agency Guidance for the Management of Long Term Health Conditions for Children and Young People - DSCB 2011). We understand that the key information requested must not be changed as it would affect any potential insurance claims for medical malpractice. Responsibilities The Governing Body adheres to the health and safety policies and procedures produced by the Local Authority and ensures that staff follow the agreed procedures detailed in this policy. They also ensure adequate training is provided as and when appropriate. Parents have prime responsibility for their child’s health. They are required to: Only keep children off school if absolutely necessary Only send children back to school when they are fit to attend. Allow 48 hours before returning children to school after a bout of sickness. Keep the school informed. (For pupils with longer term medical needs) provide schools and settings with clear information about their child’s medical condition, (including details from doctors or consultants if appropriate). It only requires one parent to request that medicines are administered and it is likely that this will be the parent with whom the school has day-to-day contact. Where possible, prescribed or non-prescribed medicines should be administered by parents outside of the school day. If this is not possible, parents should talk to school staff and also make requests to administer medicines in writing to the Headteacher on the appropriate form Parents are asked to deliver medicines to school in the original container(s) and ensuring that the medicine is not out of date and that it has been stored correctly. All medicines must be marked with the following information clearly indicated: the child’s name on the medicine; when the medicine should be given; the prescribed dose and pharmacist’s instruction, e.g., after meals. Parents must notify the school immediately (in writing) of any changes or alteration to a prescription requiring adjustment to be made to any previous arrangement about medicines for their child / young person. Headteacher The Headteacher will make appropriate arrangements for medicines to be stored safely in a locked cabinet. Medicines must be kept in the container supplied which must be clearly labelled with the name of the child and instruction for usage. The school will ensure that all medicines held are not out of date and that they are returned to parents routinely after use. Some medicines (insulin, liquid antibiotics) may need to be kept in a fridge but must not be frozen. These medicines are placed in the resources room fridge on the shelf marked ‘medicines’. Medicine cabinets will be supervised closely and emptied at least once each term. The Headteacher will make suitable arrangements in partnership with parents that enable children / young people to maintain a prescribed course of treatment. They will liaise with staff / parents / nominated support so that recommended medical treatment can be sustained, and that those people are appropriately trained to administer medication. Should the child require ‘invasive or intimate medical care then the school should consult the relevant health agencies and get the consent of staff willing to administer such care. Together with school Governors, the Headteacher will review this policy at appropriate intervals, in line with local advice, so that the well-being of children and young people and their health is safeguarded. The Headteacher will ensure that all staff and parents/carers are aware of this policy and the procedures for dealing with medical needs at Christchurch Infant School. The Inclusion Leader, (in consultation with the Headteacher if necessary), will need to agree with the parents exactly what support can be provided for a child with significant medical needs. Then a ‘health care plan’ is formulated. Where parents’ expectations appear unreasonable, further advice will be sought from the school nurse or doctor, the child’s GP or other medical advisers. The Inclusion Leader is responsible for Extended Services and will ensure that this policy is compatible and consistent with the registered day care operated by the external provider at the school. Teachers and Other Staff have a ‘duty of care’ and are required to act like any reasonably prudent parent. They are required to: Make sure that children are healthy and safe. Ensure that they are aware of the medical needs in their class or group. Such information should be given to staff by admissions officer, teacher colleagues or the Inclusion Leader (such as nature of the condition, and when and where the children may need extra attention). Ensure temporary staff are also made aware of such needs. If a child has a serious or ‘life threatening’ condition then all staff (including lunchtime supervisors) are informed as and when appropriate. All staff are made aware of the likelihood of an emergency arising and what action to take if one occurs. Teaching Assistants are responsible for administering medicines if and when required. Those who administer medicines receive appropriate and relevant training and support from health professionals. The members of staff overseeing medical arrangements are Doreen Darch, Inclusion Leader and Jane Ashenden, Headteacher. Primary Care and NHS Trusts may be involved in providing extra guidance training and advice to the school. Specialist voluntary bodies may also be able to provide additional background information and training for staff. The school nurse or doctor should help schools draw up individual health care plans for pupils with medical needs, and may be able to supplement information already provided by parents and the child’s GP. Every child should be registered with a GP. A GP owes a duty of confidentiality to patients, and so any exchange of information between a GP and a school or setting should normally be with the consent of the parent. Some children with medical needs receive dedicated support from specialist nurses or community children’s nurses, for instance a children’s oncology nurse. The Inclusion Leader is responsible for liaising with other agencies. Christchurch Infant School will ensure the following: staff work in partnership with parents/carers to ensure the well-being of child and young people; that interruption to school attendance for medical reasons will be kept to a minimum; staff who have agreed to administer medicines will receive the appropriate training; adherence to Health Care Plans; that records are maintained detailing an accurate history of the administration of medicines for the school; that information recorded when administering medicines includes: name of child / young person, the name of the medicine to be administered, confirmation that the medicine is being given and that it is not out of date, that it is being administered to the correct person, the dosage given, and the name and signature of the person administering or supervising, the date, place and time that the medicine was administered; that suitable back-up systems are in place to cover the administration of medicines staff duties in the event of staff absence; if there are any doubts or confusion about arrangements for administering medication, staff must consult with the parents and Headteacher; that no child or young person under 16 will be given medicines without their parents’ written consent; all cultural and religious views, made known to the school in writing, will be respected; the principles and advice provided in Guidance for Administering Medicines in Schools and Early Years Settings (DCC Nov 2011) will be used. The school is committed to assisting children with long-term or complex medical needs and working in partnership with their parents /carers to enable full access to schooling. Staff Training Most medicines to be administered will not require professional training; however the school will ensure that staff supervising the administering of medicines will understand that accurate records are to be kept and are completed at the time of being administered. Staff who maintain these records should be clear about what action to take, (such as referring to the Designated Senior Person for Child Protection) if they become concerned about the welfare of an individual pupil. If a Health Care Plan is applied to particular children / young people additional training must be given by a nominated Health professional, e.g., use of a nebuliser, injecting insulin, using Epipens. Training received or cascaded from parents will not be accepted unless otherwise instructed by a health professional. Record of Training Forms are completed by the Health Professional and/or Inclusion Leader and copies held both with the child/young persons records and at the school office. (See Multi-Agency Guidance for the Management of Long Term Health Conditions for Children and Young People – DSCB 2011; section 3.3 and 3.4 including Chart E.) Reasonable adjustments The school understands it’s duties under the Equality Act 2010 to make reasonable adjustments and enable children and young people to have equitable access to education. Children and young people with complex or significant medical needs will be included in activities for as much as their health permits. -3Child or young person refuses, or not well enough to take medicines If a child refuses to take medicine as prescribed, the records must state this clearly and the parents/carer must be informed immediately. Children / young people will not be forced to receive medicine if they do not wish to do so. ( E.g., see ‘Managing Medicines in Schools and Early Years Settings’, Form 6 – enter REFUSED in the ‘dose given’ column.) If a child or young person is ill / injured and therefore unable to receive the agreed prescribed medication, the person designated to supervise the taking of medicine will consult with parents / carers immediately and advise the Headteacher of their actions. If the child vomits or has diarrhoea soon after receiving medication, parents must be contacted so that they can seek further medical advice. Self medication In our school we do not permit pupils to carry ‘over the counter medicines’ (non-prescribed medicines) for their own use or self administer prescribed medicines. Those with long term health needs may ‘play a part’ in the administration of medication – however they are always supervised. Storage of Medicines The school will adhere to the advice contained in Guidance and Code of Practice - First Aid at Work (Issue 2 April 2011), and Guidance for Administering Medicines in Schools and Early Years Settings (DCC Nov 2011). The school has 1 medicine cabinet located at the school office. All medicines are stored in a locked cabinet unless: they need to be stored in the kitchen fridge to which pupils’ do not have access it is an emergency medicine, such as asthma inhaler and adrenaline pens and needs to be readily available (still out of reach of children) Prescribed controlled drugs are always kept in safe custody Disposal of Medicines Staff do not dispose of medicines. Parents are responsible for ensuring that date-expired medicines are returned to a pharmacy for safe disposal. They should also collect medicines held at the end of each term/ school year (whichever is appropriate). If parents do not collect all medicines, they are taken to a local pharmacy for safe disposal. Sharps boxes are always used for the disposal of needles. Administering Medicines No child is given medicines without their parent’s written consent. Any member of staff giving medicines to a child checks: the child’s name prescribed dose expiry date written instructions provided by the prescriber on the label or container If in doubt about any procedure, staff do not administer the medicines but check with the parents or a health professional before taking further action. If staff have any other concerns related to administering medicine to a particular child, the issue is raised with parents. Record Keeping The school must keep written records each time medicines are given. Staff complete and sign a record each time they give medicine to a child. Written details include name of child, name of medicine, dose, method of administration, time/frequency of administration, any side effects & expiry date A designated member of staff also records when first aid station and first aid trip bags have been checked. Emergency arrangements Care is taken to ensure that all children and young people are safe. The school has 7 ‘First Aid at Work’ qualified first aiders, 8 ‘Paediatric First Aid’ qualified first aiders and 9 Emergency First-Aid trained staff. [See DCC Guidance and Code of Practice – First Aid at Work (Issue 2 April 2011) for further information.] There are robust systems in place to ensure that medicines are managed safely. A risk assessment sets out an assessment of the risks to the health and safety of staff and others and measures put in place to manage any identified risks. This duty is set out in the Control of Substances Hazardous to Health Regulations 2002 (COSHH). All staff should be familiar with normal precautions for avoiding infection and follow basic hygiene procedures. Staff have access to protective disposable gloves and take care when dealing with spillages of blood or other body fluids and disposing of dressings or equipment. Our school has arrangements in place for dealing with emergency situations. This is part of the school’s first aid policy and provision. Children also should know what to do in the event of an emergency, such as telling a member of staff and taking a ‘red hand’ to the office. All staff should know how to call the emergency services and are aware of the emergency procedures in the event of need. A member of staff will always accompany a child taken to hospital by ambulance, and will stay until the parent arrives. Health professionals are responsible for any decisions on medical treatment when parents are not available. Children and young people with life threatening medical conditions or that require close monitoring / supervision may have Health Care Plans issued by Health professionals that provide contact details for emergency situations, e.g., anaphylaxis, diabetes, or epilepsy. Asthma can also be life threatening. All cases deemed ‘complex’ or ‘serious’ medical conditions have emergency contact details held in the school office, and, where necessary, key medical needs are displayed in the school. Children and young people who are at risk due to their medical condition hold a Grab Pack (collated information to pass to a doctor or ambulance crew in an emergency) that is situated in the medicine cupboard and accompanies the child/ren on school trips. The purpose of the pack is to provide emergency services with up to date information such as: diagnosis of principle conditions, key personnel and medical contacts, medication taken, up to date records of medicines that have been administered together with other relevant medical information and an agreement with parents/carers about what to do in an emergency. Off-site activities / school trips All arrangements for medicines, including the storage of medicines, Health Care Plans, and Risk Management programmes will apply for any off-site activities or school trips. A member of staff will be appointed to ensure there are suitable arrangements for storage, and recording of the medicines when assessing any risks associated for the trip, particularly for those children and young people with long term or complex health conditions. All off-site activities will be evaluated in terms of proximity and accessibility to emergency services and any implications for those with short or long term medical conditions before receiving approval to go ahead from the Headteacher / Governors. Equality Statement Christchurch Infant School is mindful of its Equality Duties; respecting religious belief and ensuring that support is provided for those with disability needs that might be affected by this policy. Where there are language or communication issues, and to avoid any misunderstanding, the parents / carers and Headteacher will agree an appropriate course of action. The Headteacher will engage interpreters or signers when required to ensure that full understanding of a child’s / young person’s medicine needs are determined accurately. Confidentiality All staff always treat medical information confidentially. The Inclusion Leader and class teachers aim to seek parental consent before passing on information about their child’s health to other staff. Sharing information is important if staff and parents are to ensure the best care for a child. The school is committed to safeguarding & promoting the welfare of children & expects all staff to share this commitment. This policy has been reviewed in line with the 9 principles set out in the Single Equality Policy and an initial screening Equality Impact Assessment has been carried out. Further Information on Health Plans and Common Medical Conditions is found in: Medical Advice for Staff in Schools – DCC Managing Medicines in Schools & Early Years Settings EYFS Requirements This policy should be read in conjunction with: Health and Safety Policy, First Aid Policy, Intimate Care Policy, Safeguarding Policy, DSCB Multi-Agency guidance for the Management of Long Term Health Conditions. This policy is reviewed as and when appropriate Last review Jan 2014