37- Synthetic organic antimicrobials
advertisement
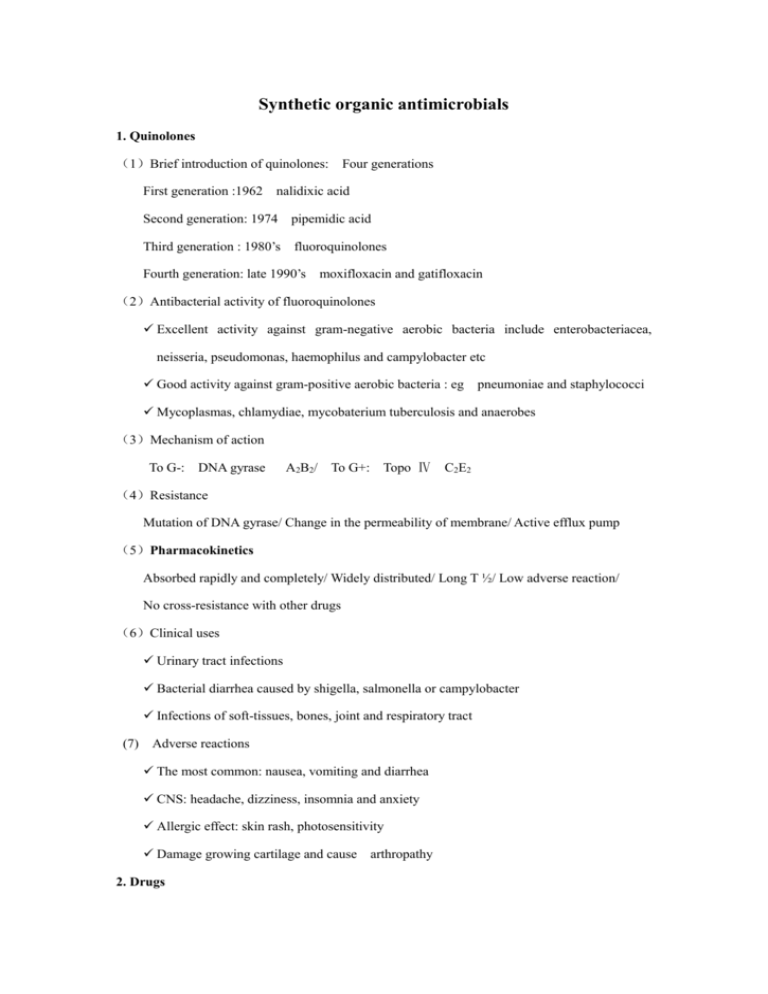
Synthetic organic antimicrobials 1. Quinolones (1)Brief introduction of quinolones: Four generations First generation :1962 nalidixic acid Second generation: 1974 pipemidic acid Third generation : 1980’s fluoroquinolones Fourth generation: late 1990’s moxifloxacin and gatifloxacin (2)Antibacterial activity of fluoroquinolones Excellent activity against gram-negative aerobic bacteria include enterobacteriacea, neisseria, pseudomonas, haemophilus and campylobacter etc Good activity against gram-positive aerobic bacteria : eg pneumoniae and staphylococci Mycoplasmas, chlamydiae, mycobaterium tuberculosis and anaerobes (3)Mechanism of action To G-: DNA gyrase A2B2/ To G+: Topo Ⅳ C2E2 (4)Resistance Mutation of DNA gyrase/ Change in the permeability of membrane/ Active efflux pump (5)Pharmacokinetics Absorbed rapidly and completely/ Widely distributed/ Long T ½/ Low adverse reaction/ No cross-resistance with other drugs (6)Clinical uses Urinary tract infections Bacterial diarrhea caused by shigella, salmonella or campylobacter Infections of soft-tissues, bones, joint and respiratory tract (7) Adverse reactions The most common: nausea, vomiting and diarrhea CNS: headache, dizziness, insomnia and anxiety Allergic effect: skin rash, photosensitivity Damage growing cartilage and cause arthropathy 2. Drugs (1)Nalidixic acid and pipemidic acid: Used only in urinary tract infection (2)Norfloxin: The least active in fluoroquinolones, F low No effects on mycoplasma, chlamydiae, mycobacterium tuberculosis, legionella Urinary tract and intestinal tract infections ( 3 ) Ciprofloxacin: The most active agent in fluoroquinolones against gram-negatives, particularly P. aeruginosa (4)Ofloxacin Improved quality in pharmacokinetics F 89% Effective on mycobateria, chlamydiae and some anaerobes Effective on resistant bacteria Second line agent for tuberculosis (5)levo-ofloxacin: F 100% Superior activity against gram-positive organisms Effective on mycoplasma, legionella, chlamydia and anaerobes Lowest toxicity among fluoroquinolones (6)Lomefloxacin: (7)Sparfloxacin: Photosensitivity Long-acting C8-F t ½>16h/ Improved activity against G+ bacteria, anaerobes, mycobateria, mycoplasma, chlamydiae / Second line agent for tuberculosis (8) Moxifloxacin : fourth generation F 90%,t ½ 12~15h / High activity on most G+ ,G-, anaerobes, mycobateria, mycoplasma, chlamydiae / Low toxicity 3. Sulfonamides (1)Classification ①Used in systemic infections Short-acting: SIZ/ Medium-acting: SD, SMZ/ Long-acting: SMD ②Used in intestinal infections: sulfasalazine ③Topical sulfonamides: SD-Ag, SA-Na, SML (2)Antimicrobial activity: Broad-spectrum bacteriostatic agents Both G+ and G- , nocardia, chlamydia, trachomatis and some protozoa (3)Mechanism of action Inhibit dihydropteroate synthesis and block bacteria folic acid synthesis (4)Clinical uses Urinary tract infection: SIZ, SMZ Meningococcal meningitis: SD first choice Ulcerative colitis: sulfasalazine Topical use for trachoma and conjunctivitis Prevent infections of burn wounds (5)Adverse effects Urinary tract disturbance: crystalluria, hematuria, obstruction Allergic reactions: fever, skin rashes, exfoliative dermatitis, photosensitivity Hematopoietic disturbances Granulocytopenia, thrombocytopenia Hemolytic reactions: lack of glucose-6-phosphate dehydrogenase 4. Trimethoprim (TMP) (1)Inhibit bacterial dihydrofolic acid reductase (2)Used in combination with sulfonamides: synergism 5. Metronidazole (1)Clinical uses Extraluminal amebiasis: drug of choice / Infections caused by anaerobes Giardiasis/ Trichomoniasis (2)Adverse reactions Gastrointestinal irritation: metallic taste in mouth, nausea, dry mouth and headache disulfiram-like effect CNS: vertigo, paranesthesia, ataxia and seizures Mutagenic and carcinogenic 6.Tinidazole