44 Oxygen enhanced imaging outside the lung
advertisement
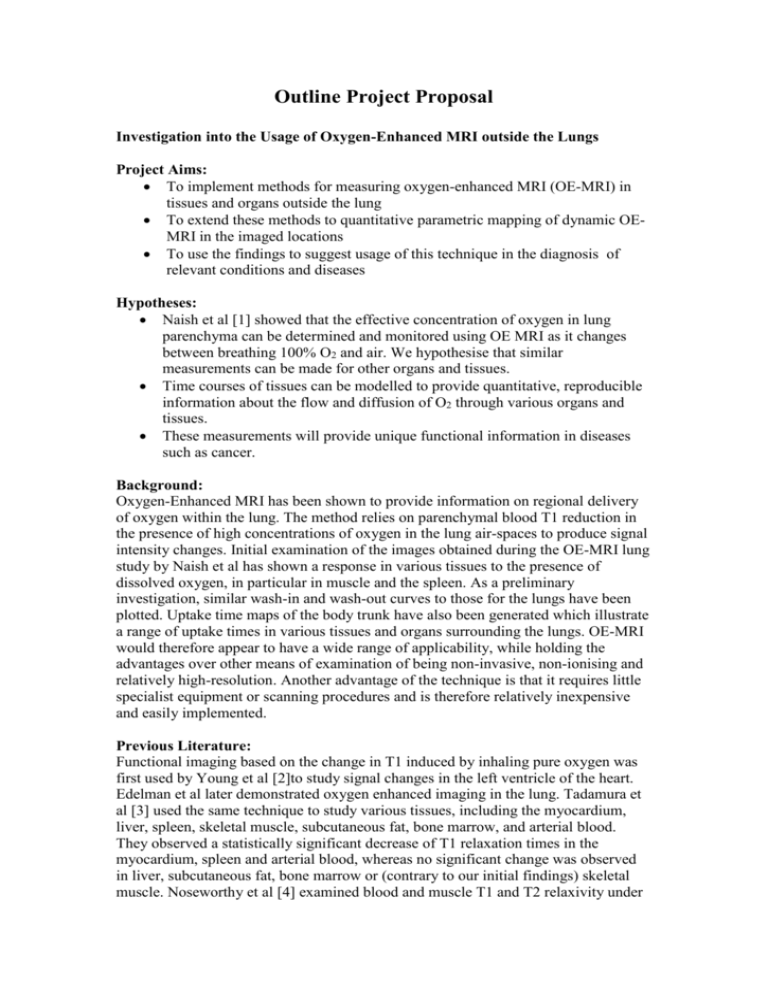
Outline Project Proposal Investigation into the Usage of Oxygen-Enhanced MRI outside the Lungs Project Aims: To implement methods for measuring oxygen-enhanced MRI (OE-MRI) in tissues and organs outside the lung To extend these methods to quantitative parametric mapping of dynamic OEMRI in the imaged locations To use the findings to suggest usage of this technique in the diagnosis of relevant conditions and diseases Hypotheses: Naish et al [1] showed that the effective concentration of oxygen in lung parenchyma can be determined and monitored using OE MRI as it changes between breathing 100% O2 and air. We hypothesise that similar measurements can be made for other organs and tissues. Time courses of tissues can be modelled to provide quantitative, reproducible information about the flow and diffusion of O2 through various organs and tissues. These measurements will provide unique functional information in diseases such as cancer. Background: Oxygen-Enhanced MRI has been shown to provide information on regional delivery of oxygen within the lung. The method relies on parenchymal blood T1 reduction in the presence of high concentrations of oxygen in the lung air-spaces to produce signal intensity changes. Initial examination of the images obtained during the OE-MRI lung study by Naish et al has shown a response in various tissues to the presence of dissolved oxygen, in particular in muscle and the spleen. As a preliminary investigation, similar wash-in and wash-out curves to those for the lungs have been plotted. Uptake time maps of the body trunk have also been generated which illustrate a range of uptake times in various tissues and organs surrounding the lungs. OE-MRI would therefore appear to have a wide range of applicability, while holding the advantages over other means of examination of being non-invasive, non-ionising and relatively high-resolution. Another advantage of the technique is that it requires little specialist equipment or scanning procedures and is therefore relatively inexpensive and easily implemented. Previous Literature: Functional imaging based on the change in T1 induced by inhaling pure oxygen was first used by Young et al [2]to study signal changes in the left ventricle of the heart. Edelman et al later demonstrated oxygen enhanced imaging in the lung. Tadamura et al [3] used the same technique to study various tissues, including the myocardium, liver, spleen, skeletal muscle, subcutaneous fat, bone marrow, and arterial blood. They observed a statistically significant decrease of T1 relaxation times in the myocardium, spleen and arterial blood, whereas no significant change was observed in liver, subcutaneous fat, bone marrow or (contrary to our initial findings) skeletal muscle. Noseworthy et al [4] examined blood and muscle T1 and T2 relaxivity under normoxic and hyperoxic conditions. They found a decrease in T1 for arterial blood and an increase in T2 for venous blood, but again no change in T1 for muscle. However using a bi-exponential model for T2 they noted an increase in a component of the T2 model for muscle. As regards T1 measurements in muscle it is worthwhile noting that Tadamura et al used the dorsal skeletal muscles and Noseworthy et al the calf muscles for their measurements. These muscles receive blood flow at a later time than the shoulder muscles we have examined (?), and are likely to benefit less from increased oxygenation. More recently Jones et al [5]have demonstrated T1 shortening in the kidneys and spleen. Much work has been carried out on measuring the effects of breathing carbogen on tumour oxygenation, e.g. Griffiths et al [6]. Measurements of the characteristics of response of various tissues and organs to pure O2 could be used in turn for similar examinations of pathologies. Draft Work Plan: Acquisition protocols for T1-weighted and T2*-weighted O2 imaging will be implemented. Oxygen breathing equipment will be constructed (same equipment as planned for O2 lung project) and tested. Acquisition protocols will be optimised for dynamic OE-MRI and volunteer scans acquired. O2 time courses on wash-in and wash-out will be modelled in a range of target organs to define normal tissue uptake characteristics. 10 volunteers will be scanned in total. No patients will be studied in this work. However, depending on which organs exhibit useful functional information, it is possible that follow-on disease studies would be possible (in, for example, tumours, pancreas, spleen, liver, muscle). Number of PDF months required 6 Non-Staff Costs Scanning costs (including breathing equipment) ~ £7000. Proposed Start and End Dates start: Feb 2005, end: July/August 2005 Milestones Construction of breathing equipment (in parallel with O2 lung project) Replication of published static enhancement studies Development of dynamic OE-MRI protocol Characterisation of normal tissue O2 uptake/washout Identification of possible disease areas for further study Outputs 1: Information sought by AZ Are these techniques likely to be sensitive to pathology? Are these techniques able to characterise normal tissue function consistently across a group? Can a clinical application be of possible use to provide markers in therapeutic trials of experimental agents? 2: Publication Opportunities Methods publication Clinical publication if applied in patients Strategic Fit AZ Novel non-invasive biomarkers that provide information related to tissue function are of potential application in trials of a range of compounds. For example, an index of oxygen diffusion within tumours would provide a surrogate for growth potential. This project is relatively ‘blue sky’ as it involves the implementation and evaluation of techniques that are currently unfamiliar to us, but which could provide unique in vivo information. Strategic Fit University Interest in dynamic contrast enhanced MRI in general and also methods to measure tumour oxygenation (GP). Complementary work to on-going lung oxygenation project. 1. 2. 3. 4. 5. 6. Naish JH, P.G., Beatty PC, Jackson A, Waterton JC, Young SS and Taylor CJ, "Improved regional analysis of oxygen-enhanced lung MR imaging using image registration". Lect Notes Comp Sci, 2004. 3216: p. p 862-869. Young IR, C.G., Bailes DR, Pennock JM, Doyle FH and Bydder GM, Enhancement of Relaxation Rate with Paramagnetic Contrast Agents in NMR Imaging. Jounal of Computer Assisted Tomography, 1981. 5: p. 543-547. Tadamura E, H.H., Li W, Prasad P, Edelman R, Effect of Oxygen Inhalation on Relaxation Times in Various Tissues. Journal of Magnetic Resonance Imaging, 1997. 7(1). Noseworthy MD, K.J., Stainsby JA, Stanisz GJ and Wright GA, Tracking Oxygen Effects on MR Signal in Blood and Skeletal Muscle During Hyperoxia Exposure. Journal of Magnetic Resonance Imaging, 1999. 9: p. 814-820. Jones RA, R.M., Moonen CTW and Grenier N, Imaging the Changes in Renal T1 Induced by the Inhalation of Pure Oxygen: A Feasibility Study. Magnetic Resonance in Medicine, 2002. 47: p. 728-735. Griffiths JR, T.N., Howe FA, Saunders MI,Robinson S,Hoskin PJ, Powell MEB,Thoumine M, Caine LA, and Baddeley H, The Response of Human Tumours to Carbogen Breathing, Monitored by Gradient-Recalled Echo Magnetic Resonance Imaging. International Journal of Radiation Oncology Biology Physics, 1997. 39(3): p. 697-701.