Abnormal Sexual differentiation
advertisement
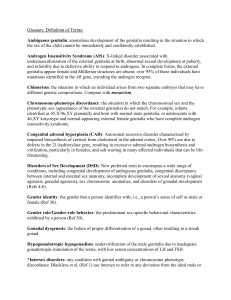
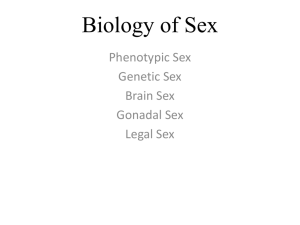
Normal and abnormal sexual development Definition and elements of sex Normal Sexual Differentiation: Genetic factors: Gonadal Factors: Hormonal Factors: Central nervous system differentiation. Abnormal Sexual differentiation: Sex: Is the gender assigned to an individual based on appropriate and compatible morphologic features, function and behaviour. Determinants of normal sexual differentiation: include the following elements: Genetic sex, Gonadal sex, internal genital sex, external genital sex and behavioural sex. Intersexuality: Is said to occur whenever there is a conflict between one or more of the elements of sexual differentiation. Normal Sexual differentiation: Genetic Sex: Is assigned the moment fertilisation takes place. Based on a normal genetic make up the gonadal sex will be determined as ovaries or testis. For example normal differentiation of the gonads to testis depends on the presence of functioning testicular determining factor gene Also loss of one of the X chromosome or deletion of important part of it will result in the gonads being fibrous streaks. Gonadal sex: The gonads appears at 5 weeks as protuberance overlying the mesonephric ducts. migration of the germ cells into the genital ridge to induce gonadal differentiation. Development of the gonads goes into two stages: Stage of Indifferent gonads (up to 6 weeks): The gonads are bipotential i.e. can differentiate into ovaries or testis. It is formed of : Cortical area, medullary area, germ cells, epithelial cells ( granulosa cells or Sertoli cells) and mesenchyme (Theca or lyeding cells). Failure of migration of the germ cells results in gonadal agenesis. Differentiation into testis occur between 6-8 weeks in case of XY germ cells. If the genetic make up is XX ovarian differentiation begins from around 8 weeks. Development of the Internal genital system (Duct system differentiation) At one stage the embryo will harbour both elements for male and female duct system i.e. the Wollfian (mesonephric) duct and the Mullerian (paramesonephric) duct. Differentiation begin at around 8-10 weeks into male depending on: AniMullerian hormone (AMH), synthesised by Sertoli cells soon after testicular differentiation. It results into regression of the ipsilateral Mullerian duct which takes place by about 8 weeks before the production of testosterone begins and subsequent development of the Wollfian duct. The gene for AMH is located on the short arm of chromosome 19. While the receptor for AMH is located on chromosome 12. Genetic defects in production of AMH or its receptors results in persistence of the Mullerian duct system (later to be the uterus and tubes) in otherwise normal male. AMH is also important for descent of the testis in the scrotal region. Testosterone Is secreted by the Leyding cells from about 8th week. It results in Wollfian duct differentiation into epidedymes, vas difference and seminal vesicles. It has a paracrine effect (the ipsilateral duct). Therefore the Wollfian duct can not be stimulated in females exposed to adrenal or exogenous androgen. The testosterone hormone reaches peak by 15-18 weeks. Secretion of testosterone depends on normal Leyding cell function, HCG and latter fetal pituitary LH. In the absence Y chromosome, the duct system differentiation into the default female. The Wollfian duct regress and the Mullerian duct differentiate into tubes, uterus and upper vagina. However oestrogen hormone seems to play a role in the regression of the Wollfian system. External Genital differentiation: Stage of indifferent genitalia: At 6 weeks the external genitalia is bipotential state i.e. can differentiate into male or female. Its main elements include: The genital tubercle: in male give the penis and in female the clitoris. The labioscrotal swelling to become the scrotum or the labia minora. The urogenital sinus to make the penile urethra or the labia minora. With the sinus to give the urethra and vaginal in female. The target tissue of the external genitalia must convert testosterone into dihyrotestesterone using the 5 alpha reductase enzyme. Deficiency in this enzyme with leads to variable degrees of ambiguous genitalia. Other effects of DHT are temporal hair line recession, growth of facial and body hair, development of acne, development of external genitalia and prostate. Abnormal Sexual differentiation Disorders of Fetal endocrinology (hormonal factors) Masculinized females (Female pseudohermaphroditism) Congenital Adrenal hyperplasia: Elevated androgen in the maternal circulation: Aromatase (P450arom) deficiency Incompletely Masculinized males (male psuedohermaphroditism) Androgen insensitivity syndromes 5 Alpha reductase deficiency Testosterone biosynthesis defects Gonadotropin resistant testes Anti-mullerian hormone deficiently. Disorders of Gonadal Development: Male pseudohermaphroditism Primary gonadal defect True hermaphroditism Gonadal dysgenesis: Turner syndrome Mosaicism Normal karyotype (Noonan syndrome) Congenital Adrenal Hyperplasia (Adrenogenital Syndrome): In female the syndrome is characterised by masculinization of external genitalia. It is diagnosed by the demonstration of excessive androgen production by the adrenal cortex, caused by either tumour or hyperplasia. It may appear in utero or develop postnatally. The features and severity depends on the time of onset, quantity available and duration of exposure. Signs of virilisation of the external genitalia are varying degrees of: fusion of the labioscrotal folds, clitoral hypertrophy, and anatomical changes of the urethra and vagina (deformity of the urogenital sinus). The internal genitalia differentiated is not affected because it is completely formed by the 10th week whereas adrenal cortex does not reach a level of significant function until 10-12 weeks. Because the female external genitalia is not completed until 20 weeks of fetal age early androgen excess (10-12 weeks) may fully musculinize, whereas late (18-20 weeks) androgen may create limited ambiguity of the basically female appearance of the external genitalia. Postnatally if untreated the female infant will develop progressive signs of virilization (pubic hair at age 2-4 years, followed by axillary hair, body hair and beard) bone age is advanced by age. In addition to sexual changes patients can present with metabolic disorders such as salt-wasting, hypertension, rarely hypoglycaemia. The condition is an inherited monogenic autosomal recessive trait. Masculinization due to elevated androgen in the maternal circulation: Abnormal (P450arom) Deficiency: Placental aromatase deficiency result in accumulation of fetal androgen precursors normally utilised in placental synthesis. The result is virilisation of the mother during the second half of pregnancy, low oestrogen levels in the mother and masculinization of a female fetus. Incompletely musculinized Males: Those are male by genetic sex ( XY) and possess testicles but the external genitalia are not normally male (pseudohermaphrodits): 1234- Androgen Insensitivity Syndrome.( X linked recessive trait) Abnormal androgen synthesis. Gonadotropin resistant testes. Absent or defective anti-mullerian hormone. Androgen Insensitivity Syndromes: 1Complete. (Testicular femenisation syndrome) 2Incomplete Androgen Insensitivity. Abnormal Androgen Synthesis: This may result in defective male development if it occurs at a critical time of sexual differentiation. Gonadotrophin resistant Testes: Due to agenesis or abnormal differentiation of the Leyding cells thus reduced response to LH/HCG. Absent or defective anti-mullerian hormone: Individuals in this syndrome are normal males with uterus and tubes. Disorder of Gonadal Development: Bilateral dysgensis of the testes: normal female external and internal genitalia but the gonads are streaked fibrous tissue. The karyotype is XY. True hermaphroditism: Individual who possess both ovarian and testicular tissue. Either on the same side (ovotestis) or one on each side. About 60% are genetic females’ (XX) few are XY the rest are mosaic. Gonadal Dysgenesis (Turner syndrome): The typical complete case is due to absence of the X chromosome in all cell lines result in bilateral streaked gonads. This occurs in 60 % of cases. The rest has either structural abnormality in one of the X-chromosomes or mosaicism with an abnormal X. Mixed Gonadal Dysgenesis: The most common example is the mosaic individuals with 45X/46XY. The can exhibit a wide variety of phenotypes range from new-borns with ambiguous genitalia to normal fertile males or normal phenotype female with bilateral streaked gonads.