18_Westermark\Westermark
advertisement

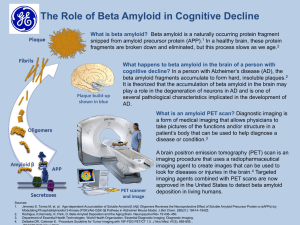
1 Physiological and pathophysiological role of islet amyloid polypeptide (IAPP, amylin) Gunilla T. Westermark Department of Medical Cell Biology, Uppsala University, Uppsala, Sweden 2 IAPP has a number of effects which may be of physiological relevance. Islet amyloid, which earlier was regarded as a non-important degenerative product, most likely plays a central role in the loss of beta cells in type 2 diabetes and probably in transplanted human islets. Taken together the results from human and animal studies show that amyloid develops before beta-cell deficiency and the occurrence of oligomers and amyloid intracellular induce beta cell death. Prevention of islet amyloid most likely will save beta-cells and extend hormone secretion. Key Words: Islet amyloid; Islet amyloid polypeptide; IAPP; ProIAPP, ER-Stress; Apoptosis; Posttranslational processing. 3 Islet amyloid polypeptide Islet amyloid polypeptide (IAPP) was originally isolated as the major peptide constituent of the amyloid from an insulinoma (1), and subsequently isolated from amyloid deposits present in the islet of Langerhans from patients with type 2 diabetes (2, 3). The 37 residue polypeptide proved to have an earlier unknown sequence, but showed an almost 50% identity to the known calcitonin gene related peptide (4). Other nomenclatures for IAPP are amylin (5), Diabetes Associated Peptide (6) and IAP Insulinoma Amyloid Peptide (1). IAPP is phylogenetically well preserved and found in all mammals where it has been looked for (7-10), and also in an avian (11) and fish (12). During embryogenesis in mice, IAPP was detected in the primordia at E12 and the immunoreactivity was restricted to the simultaneously occurring insulin expressing cells (13). In human, IAPP immune-reactive cells were demonstrated from week 13 of gestation and here its expression was preceded by insulin that was present already at 9 weeks of gestation. In fetal and neonatal pancreas there were a higher number of insulin positive cells than IAPP positive cells, but this difference did not remain in the adult pancreas where all beta cells co-express insulin and IAPP (13, 14). An additional expression pattern in developing mice was described by Wilson et al. (15) where IAPP and proglucagon/glucagon reactivity co-localized in the primordia at E.10.5 in cells also expressing PC1/3, a convertase not present in the alpha cells of the mature pancreas. Instead, PC1/3 is expressed in beta cells and together with proglucagon in intestinal L-cells. Cells positive for IAPP and glucagon did not express pdx-1, an activator of the IAPP gene (16) but they expressed brain-4 (Brn-4). Brn-4, 4 originally described in brain, is also a regulator of glucagon expression in alpha-cells (17). In human, IAPP is almost exclusively produced by the beta-cell where it is stored (18) and released together with insulin (19) and only minor synthesis occurs in enterochromaffine cells in the intestinal tract (20). IAPP is synthesized as an 89 residues long prepropeptide (21, 22) from which an 18 residue signal peptide is removed in the endoplasmatic reticulum. Posttranslational cleavages of proIAPP occur at dibasic residues and comprise the removal of N- and C-terminal flanking peptides. This proIAPP processing is initiated in the late transgolgi where cleavage by the proprotein convertase PC1/3 removes 16 residues at the carboxy terminus (23, 24) followed by PC2 cleavage in the secretory granules that leads to the removal of an 11 residue peptide at the amino terminus (25). The residues Lys-Arg that remain at the C-terminus after PC1/3 cleavage are removed by carboxy peptidase E (CPE) (26). To receive full biological activity, IAPP must be cyclized by a disulfide bond between the cystein residues at position 2 and 7 of the mature IAPP and be Cterminally amidated (27). An additional processing site is present at residues 79-80 (Lys-Arg) of the C-terminal flanking peptide, but no extended IAPP peptide has been described (Figure 1). Proinsulin is processed to insulin by the same convertases at the same location (28), and IAPP and insulin are stored in the same secretory granules (29-31) . In the mature granule IAPP and C-peptide occupy the halo region while Zn2+ insulin is present in the dense core region (32). The insulin to IAPP ratio varies but is often reported to be 10 to 1 (32-34). However, heterogeneity among beta-cells occurs (35). Reported non-stimulated plasma levels of IAPP in man range between 2-20 pM IAPP (36, 37). IAPP is cleared by the kidneys (38) and insulin is cleared by the liver and 5 kidneys (39, 40). The clearance of IAPP is almost 4 times slower than that determined for insulin but comparable to that for C-peptide (41).Taking this in account, a comparison of IAPP and C-peptide plasma levels might be more accurate and reflect the actual ratio. The IAPP to insulin ratio remains constant under normal circumstances and is not affected by type of stimuli (42). However, assays used for IAPP quantification will not discriminate between the active hormone and the partially or non-processed hormone. Regulation of the IAPP gene The human IAPP gene is a single copy gene situated on the short arm of chromosome 12 and consists of three exons separated by a 0.3 kb and 5 kb intron, respectively. Exon1 encodes most of the 5’ untranslated region of the transcribed RNA while exon 2 encodes the signal peptide and 5 residues of the N-terminal flanking peptide and exon 3 encodes the remaining residues 6-89 of the preproIAPP molecule (21, 43-46). Transcription of the IAPP gene is controlled by a promoter situated within the sequence spanning from -2798 to + 450, relative to the transcriptional start codon (47). IAPP and insulin genes contain similar promoter elements (48) and the transcription factor PDX1 regulates the effects of glucose on both genes (49-52). Glucose stimulated beta-cells respond with a parallel expression pattern of IAPP and insulin (53, 54). The islet hormones interplay in the regulation of glucose homeostasis (55), and insulin and glucagon stimulate IAPP gene expression (16), in contrast to somatostatin that has no effect (56) Receptor for IAPP 6 IAPP belongs to the calcitonin family of peptides also including calcitonin (57), calcitonin gene-related peptides (CGRP) (58), adrenomedullin (59) and intermedin (60). For long, there was a futile search for a specific IAPP receptor, and it was not until the discovery of the receptor activity modifying proteins (RAMPs) the problem was solved. RAMPs constitute a family of three different single transmembrane proteins (61) that by combining with the G protein coupled calcitonin receptor (CTR) or the calcitonin receptor-like receptor (CLR) (62) determine the ligand specificity and also increase the receptor repertoire (63). Paring of RAMP3 with a CT receptor forms an IAPP specific receptor (64). IAPP in other species A more disperse distribution of IAPP is seen in other species. In rat and mouse, IAPP immunoreactivity co-localises partly with gastrin, somatostatin and peptide YY in enteroendocrine cells in the gastrointestinal tract (65, 66) and in pancreas IAPP is present in beta and delta cells (67). IAPP is expressed in the rat brain, and sometimes with a different distribution of that shown for CGRP (68). In chicken the IAPP immunoreactivity was co-localised with insulin in the small islets, but mRNA expression analysis revealed higher signals from intestines and brain (11). In fish, IAPP immunoreactivity is present in the islet organ Brochmann body (12) and in the intestinal tract . Physiology of IAPP Glucose regulation 7 Taken together the results from a large group of researchers suggest that IAPP exert an autocrine or paracrine effect on beta cells and act as a modulator of insulin secretion (69-71). Glucose stimulated insulin secretion from perfused rat pancreas can be inhibited by IAPP at 75pmol/l, a concentration equal to that determined in the effluent from rat pancreas. The inhibitory effect on insulin secretion is limited to physiological changes of glucose and no effect remains when glucose levels are augmented from 5.5 mmol/l to 16.6 mmol/l (72) . Insulin secretion in response to other secretagogues such as sulfonylurea that block ATP dependent K channels or KCl that depolarized beta cells are also markedly reduced by IAPP (73). IAPP infusions in rats with hyperglycaemia clamped at 11 mmol/l showed a dose dependent reduction in insulin secretion, and 8.5 pmol/min and 85 pmol/min reduced plasma insulin by 31% and 53%, respectively (74). The inhibitory effect on insulin secretion ceased by time and IAPP is suggested to be a short-time regulator of insulin secretion (74). Immunoneutralisation of intra-islet IAPP by specific antibodies or by the IAPP inhibitor IAPP 8-37 potentiates both glucose and arginine stimulated insulin release (71). This is in accordance with the finding that IAPP null mice have a more rapid glucose clearance in response to both oral and intravenous administrated glucose (75). This phenotype was reversed by the introduction of human IAPP in the IAPP null mice. Peripheral effects of IAPP There are great differences in the reported in vitro and in vivo effects on IAPP and some of these differences could be ascribed to the use of pharmacological levels of IAPP, the solubility of IAPP or other not yet known circumstances. 8 An early reported effect for IAPP was the reduction of basal and insulin-stimulated glycogen synthesis in rat skeletal muscle (76). In the work by Furnsinn et al, shortterm IAPP infusion reduced glycogen content in the hindlimb rat muscle (74). Again, this effect was only seen after short-time IAPP exposure and did not remain after long-term exposure. IAPP can regulate glycogen synthesis by activation of glycogen phosphorylase and inactivation of glycogen synthase (77-79), effects antagonised by IAPP 8-37 (79). IAPP has also been shown to cause peripheral insulin resistance in vivo in cat (80), rat (81) and dogs (82). In contrary, Kassir et al. failed to measure any change in the insulin-stimulated glucose disposal rate in dog (83). A single injection of IAPP was shown to partly inhibit glucagon release in freely feed mice while IAPP had no effect after a glucose load. Glucagon secretion stimulated by L-arginine was reduced by IAPP while glucagon stimulated by hypoglycaemia was unaffected (84). In cat, rat-IAPP injection 5 minutes prior to intravenous administration of arginine or glucose lowered plasma glucagon levels and reduced also the insulin levels (85). Therefore, one effect for IAPP secreted together with insulin in response to a rise in blood glucose may be to modulate postprandial glucagon secretion. Gastric emptying Administration of IAPP has been shown to delay gastric emptying and thereby reduced the increase in postprandial glucose (86-88). Due to the absence of endogenous IAPP in type 1 diabetes gastric emptying is expected to be accelerated. When this was monitored in 21 patients with type 1 diabetes mellitus, no significant difference in mean or median time compared to the controls could be detected. However, it should be pointed out that a large variation occurred among the 9 individuals with type 1 diabetes and increased emptying occurred in a sub-group without secondary complication (89). However, in a recent study by Heptulla et al, it was hypothesised that accelerated gastric emptying should occur in children with complication-naive type 1diabetes. Instead they found delayed gastric emptying when compared to controls (90). Therefore, administration of IAPP in individuals lacking the hormone seems to have a different effect than expected on gastric mobility. Regulation of food intake The central high affinity binding sites for IAPP are concentrated to nucleus accumbens, area postrema and in the immediate adjacent nucleus of the solitary tract in rat (91) and monkey (92). Both centrally (93-96) and peripherally (97-99) administered IAPP reduces food intake and produces anorexia in mouse and rat. Chronic subcutaneous infusion of IAPP, at concentrations kept within the pathophysiological range, causes a dose-dependent reduction of food intake and body weight gain by lowering the adiposity (99).The anorectic effect from chronic peripheral infusion was abolished in rats after AP/NST lesion (100) and the effects of intraperitoneal injections of IAPP was reduced by direct injections of IAPP receptor antagonist AC187 into the area postrema (95). Chronic intraperitoneal infusions of AC187 increased the total food intake in genetically obese fa/fa rat but were ineffective on lean littermates. IAPP can enter the blood brain barrier (101) and the anorectic effects exerted by peripheral IAPP indicate that the molecule might be a satiety factor. One side-effect found during the clinical trials with the IAPP analogue pramlintide was a slight weight reduction in the study group. 10 The expression pattern of intracranial IAPP is somewhat unclear and local expression was reported to occur at multiple sites in the rat brain (68) (102). If IAPP produced at this site participates in the regulation of food intake has yet to be resolved. In a study on postpartum mRNA regulation a 25 fold increase of IAPP was detected in the preoptic area of the hypothalamus. The increase was verified at the peptide level and suggests that IAPP plays part in maternal regulation (103). Calcium metabolism IAPP participates in the regulation of total bone mass and stimulates osteoblast proliferation and bone formation, in both rodent and human (104, 105) cultured osteoblasts. Bone absorption is reduced because IAPP slower the mobility of osteoclasts (106-108) and prevents the fusion of the preosteoclasts into multinucleated osteoclasts shown in rodent cell culture (109). IAPP null mice have a 50 % reduction in bone mass when compared to wild type mice (110). It still needs to be elucidated if IAPP has any significance for the development of osteopenia, but IAPP fasting levels are reported to be significantly lower in patients with osteoporosis and in women with anorexia nervosa, a disease frequently associated with osteoporosis (111) . IAPP as a drug in obesity and diabetes treatment Pramlintide/symlin is a synthetic analogue of IAPP with three structure-breaking proline substitutions inserted at position 25, 28 and 29 to inhibit aggregation of the peptide (Figure 1). This exchange of residues makes pramlitide more like the rat IAPP. Symlin was approved by US food and drug administration (FDA) in 2005 (112), 11 but not elsewhere, to be given together with insulin to control post meal blood glucose in patients with type 1 and type 2 diabetes. Over the recent years, multiple clinical trials on the effects of Pramlintide have been undertaken. All in all the reported biological effects including an often mild weight decrease, significant reduction in HbA1c and a decrease in insulin dose. The drawback was the experience of a transient nausea. More interesting is the finding from ongoing clinical studies where a combination of pramlintide and the leptin analoge metreleptin were given and resulted in an approximately 13% weight loss after 24 weeks, a reduction significantly more than after treatment with pramlintide or metreleptin alone (113). Amyloid Amyloid in general Amyloidoses constitute the largest group among the protein misfolding diseases, and today, thirty different proteins have been characterized from amyloid deposits in human (114). The proteins are unrelated and each protein is linked to a specific amyloid disease. Based on the distribution pattern, the diseases are divided into two forms, systemic amyloidosis where deposits are present throughout the body and where the precursor proteins most often are plasma proteins, and localised amyloidosis where the deposits mainly are restricted to the site of production and where not all but many of the precursors are polypeptide hormones. Amyloid is often referred to as an amorphous material, but it consists of fibrilar structures with a diameter of 7-10 nm and of indefinite length. The protein molecules that make up the fibrils are aligned perpendicular to the fibrilar axis and this is 12 believed to cause the specific tinctorial characteristic of amyloid, affinity for Congo red and green birefringence in cross polarized light. Formation of amyloid can be separated into three separate phases, a lag phase, an elongation phase and a plateau phase. The lag phase is of undefined length and can last from minutes up to a life time. It is during this period the monomer unfolds and forms small amyloid aggregates. These aggregates can act as templates and amyloid fibrils extend from these during the elongation phase. The elongation of fibrils will continue until the plateau phase is reached, dependent on the equilibrium for the specific peptide (115, 116). In experimental in vivo and in vitro models for amyloid formation, the introduction of a minute amount of preformed amyloid fibrils can dramatically shorten the lag phase and cause rapid amyloid formation. It is evident that extracellular amyloid can be degraded and cleared, but often the formation of amyloid exceeds the resolution and therefore the amyloid mass will continue to grow as long as the precursor is supplied. Islet amyloid Islet amyloidosis is a localised form of amyloid disease and was described by Opie in 1901 (117). Islet amyloid is the main islet pathology present in individuals diagnosed with type 2 diabetes, but the reported frequency of amyloid varies from 40 -100% (118-122). This rather large discrepancy in amyloid frequency between reports and the presence of amyloid in islets of non-diabetic subjects has questioned the importance for islet amyloid as a cause of type 2 diabetes. In a study by Maloy et al., amyloid was present in 59% of the subjects with diabetes but when the group was subdivided dependent on treatment, it was shown that the patients that received 13 insulin treatment all had islet amyloid (119). This points to an association between the severity of the disease and the prevalence of islet amyloid . In addition to man, islet amyloid occurs in primates (123-125) and cats (126). In primates, there is an increased risk for spontaneous diabetes when kept in captivity and the disease development includes obesity and hyperinsulinaemia, a disease pattern that resembles the type 2 diabetes that develops in humans. There are three studies on different monkeys that connect islet amyloid with the development of diabetes. In Macaca nigra, the amyloid area was determined in pancreas biopsies and at autopsy in 18 monkeys, some followed for 10 years (127). The amyloid area was determined and compared to the result of an intravenous glucose tolerance test. In non-diabetic monkeys the amyloid area did not exceed 3% and no abnormalities in insulin secretion or glucose clearance was detected. When the amyloid load progressed and affected 20-40% of the islet area both insulin secretion and glucose clearance was decreased. Diabetes shown by hyperglycaemia developed when the amyloid area exceeded 50-60 %. In Macaca mulatta the progression of the metabolic deterioration was correlated to the islet morphology present in autopsy biopsies (125). Animals were divided into 4 different groups: 1;lean young monkeys, 2; monkeys > 10 years old, 3; monkeys with normoglycaemia and hyperinsulinaemia and 4; diabetic animals. In group 3 the beta cell volume was increased while group 4 animals had a reduced beta cell volume. Amyloid deposits were present to a varying degree in 4 of 6 group 3 animals replacing 0.03- 45 % of the islet mass. In the diabetic group amyloid was present in 8 of 8 animals and the affected area varied between 37-81 % of total islet area. In the third study, performed on 150 baboons the metabolic state was correlated to the islet amyloid mass and the result thereof showed that the levels of fasting plasma glucose was sensitive and specific enough 14 to determine the extent of amyloid (123). This latter is different from studies on human where islet amyloid was significantly associated with a higher mean HbA 1c but not with fasting blood glucose levels (128). Islet amyloid does not develop in mouse or rat. This depends on the amino acid composition and especially the three proline substitutions present at position 25, 28 and 29 in rodent IAPP are assumed to prevent amyloid aggregation (129). In the model for human IAPP fibril formation presented by Jaikaran et al. the regions made up by residues 1 to17, 18 to 27 and 30 to 37 form strands that fold and form intramolecular beta-sheet structures while the residues at position 17-19 and 28 and 29 form the beta-turns. The presence of proline residues, which are known beta-strand breakers, at position 28 and 29 will disrupt the structure and prevent fibril formation (Figure 1) (130). CD analysis of human IAPP in monomeric form revealed mainly random coil structure (131, 132), and NMR analysis on human IAPP and rat IAPP when bound to membrane, showed alpha-helical content in the N-terminus (133). The presence of amyloid in the islets of Langerhans in the South American rodent Octodon degus was surprising since the predicted IAPP sequence after cDNA analysis from degu revealed a non-amyloidogenic IAPP sequence with protective proline residues at position 28 and 29 (134). Interestingly, an insulin sequence was obtained when the degu islet amyloid was sequenced (135). Degu insulin sequence diverges from human and rat insulin at 32 out of 53 positions (134) and these differences could result in a potentiated amyloidogeneity. The degu develops diabetes when kept in captivity, and therefore, despite the different origin of the amyloid in the islets of Langerhans in degu it points clearly to the importance for amyloid in the islets. 15 Amyloid in transgenic animal models The original data on islet amyloid derive from studies performed on material recovered post-mortem and we are still waiting for new methodology that will allow in vivo studies on islet amyloid in humans. Meanwhile studies have been performed on transgenic animals which have been very useful and facilitated a large number of studies on IAPP cell toxicity and amyloid formation and allowed the exploration of different pathways role in amyloidogenesis. Several transgenic mouse strains that express the human IAPP gene linked to the rat insulin I or II promoter (136, 137), cDNA for human IAPP associate with the rat insulin II promoter, cDNA for human IAPP linked to human insulin promoter (138) and a transgenic rat strain expressing the cDNA encoding human IAPP driven by rat insulin II promoter (HIP rat) have been established (139). A strain that expresses human IAPP, but made deficient for endogenous IAPP expression was made by crossing a transgenic mouse with an IAPP deficient strain. Expression of the human IAPP gene in the IAPP null mice ameliorated the defect insulin secretion detected in this strain. Formation of amyloid caused solely by over-expression of human IAPP was only found in one mouse strain (140). In other strains, amyloid occurred in mice fed a diet high fat (141, 142) after treatment with dexamethasone or growth hormone (143) or when introduced into a diabetogenic trait (144). In human IAPP transgenic ob/ob mice the extensive IAPP production caused amyloid to form in parallel with the development of insulin deficiency and persisting hyperglycaemia (144). In the HIP rat, over-expression of human IAPP lead to spontaneous development of hyperglycemia in transgenic rats by the age of 4 months and overt diabetes was present in all rats by the age of 10 months. In these animals the amyloid amount did not correlate to 16 the fasting blood glucose. Instead a positive relationship between beta-cell apoptosis and fasting blood glucose was reported. An earlier prerequisite in the definition of amyloid was that it should be present extracellularly and this was also the main finding in the post-mortem material, often affected with massive amyloid load and autolysis. However, some amyloid present in insulinoma (145) and human islets transplanted to mice (146) appeared to be present intracellularly. In transgenic mice or in cultured islets isolated from such animals, it was shown that initial amyloid formation occurs intracellularly (140, 142, 147). The amount of amyloid deposited in cultured islets was clearly dependent on the glucose concentration. Oligomers and cell toxicity In some amyloid diseases it has been clear that the massive amyloid burden does not always correlate to the clinical picture. Instead, the attention was drawn to the fibril formation process and it was shown that aggregation to amyloid fibrils involves formation of intermediates, and these oligomeric assemblies are ascribed the cell toxic effect. The term oligomer is still a matter of debate. It does not define a homogenous population of aggregates and the number of monomers varies. Most of the results on oligomers arise from studies on A-beta, the amyloid protein deposited in the Alzheimer brain where soluble oligomers have been implicated as the toxic species, responsible for cell death (148) and (149). When Lorenzo et al. added mature IAPP fibrils to beta-cells in culture they detected apoptosis. With today’s knowledge, it is most likely that oligomers were present in the solution and the propagation of amyloid fibrils induced apoptosis (150). The general mechanism is supported by the existence of antibodies that recognize cell toxic oligomers 17 independent of the nature of amyloid protein (151). Different models for how oligomers exert their toxic activity exist. An early finding (150) was that A-beta can form ion leaking channels in lipid layers (152, 153). Human IAPP was also shown to form active channel structures while this was not seen by rat IAPP (154). Atomic force microscopy studies on channel structures suggest that the IAPP channel consists of five IAPP molecules (155). A second model for IAPP toxicity is membrane permeabilization during fibril elongation (156, 157). The N-terminal part of human and rat IAPP contains alpha-helical structures and can interact with the membrane, but only human IAPP can aggregate and form the amyloid fibrils that disrupt the membrane. The result of this model fits well with the electron microscopical picture on amyloid interaction with beta-cells (Figure 2). Being a secretory protein IAPP will after synthesis enter the secretory pathway starting with the endoplasmic reticulum where the SS-bond is form and eventual further folding is assisted by chaperons, transported to golgi and finally to the secretory granule where the main part of the posttranslational processing occurs. The mature proteins are stored in the secretory granules, waiting for secretion. If not used the granule content will be degraded by crinophagy. Type 2 diabetes is often preceded by peripheral insulin resistance that is compensated for by an increased insulin biosynthesis. This increase in the demand on the secretory machinery in the beta-cells can cause endoplasmic reticulum (ER)stress which can induce apoptosis if not compensated by activation of the unfolding protein response (UPR). The UPR response includes upregulation of ER-resided chaperones to assist folding of aggregated proteins, a selective inhibition of protein synthesis to reduce ER workload in favour for synthesis of proteins that augment UPR and transport of mis-folded proteins to the ubiqutine-proteosome system (UPS) 18 for degradation. It has been shown that over-expression of IAPP in cell lines and in the HIP rat activates apoptosis and reduces the beta-cell number (139, 158). A sixfold increase of positive islet cell nuclei was detected in human pancreatic sections from patients with type 2 diabetic subjects not present in non-obese or obese nondiabetic patients (159). The stress inducible transcription factor CHOP is present in the ER and if activated during ER-stress, it will translocate to the cell nucleus. An increased production of the ER-stress markers HSPA5, CHOP, DNAJC3 and BCL2associated X protein was detected in human pancreatic islets recovered from diabetic subjects (160). However, in this immunological study CHOP reactivity appeared to be restricted to the cytosole without translocation to the cell nucleus. The association between human IAPP expression and ER stress induction is still contradictory. Hull et al. failed to detect changes in the mRNA expression of the ERstress markers Bip, Atf4 and CHOP and splicing of Xbp1 mRNA in mouse islets expressing human IAPP after culture in 11.1, 16.7 and 33.3 mmol/l glucose (161). The islet amyloid that developed was associated with reduced beta-cell area in a glucose- and time-dependent manner. In a recent paper from Peter Butlers research team, where the commercially available oligomer antibody A11 was used, oligomers were found intracellularly in human islets from patients with type 2 diabetes (162). The oligomers disrupted the membranes of the secretory pathway and entered the cytosol. Oligomers were also found in close association to mitochondria. IAPP in the secretory granules IAPP is present in the halo region of the secretory granules and a fibrilar material, recognised by proIAPP specific antibodies are present in beta-cells affected by small amounts of amyloid (163, 164). When the intracellular amyloid mass expands, 19 granule-sized aggregates fuse and replace the cytosol. Cells stained for intracellular amyloid are also recognised by the apoptos-marker M-30 (164). During the hyperinsulinemic period that precedes diabetes there is an increase in secretion in proinsulin and partially processed proinsulin (32-33 split proinsulin) (165, 166). Because proIAPP is processed by the same convertases a similar change of processing of proIAPP is expected with an increase in secretion of IAPP bound to the N-terminal propeptide (N-IAPP). When human beta-cells were incubated in 20mmol/l glucose the cellular content of insulin was decreased without a concomitant decrease of IAPP resulting in a shift in IAPP to insulin ratio. Western blot analysis of cell content showed a raise in proIAPP and an intermediate that in size corresponded to N-IAPP (167). Expression of human proIAPP in B-TC 6 cells that express PC2 and PC1/3 and where proIAPP is expected to be processed into IAPP, failed to show amyloid formation. Expression of proIAPP in GH4C1 cells that lack PC2 and PC1/3 or AtT-20 cells that lack PC1/3 and where aberrant processing of proIAPP occurs, lead to amyloid formation (168). IAPP is known to be one of the most amyloidogenic peptides and is readily assembled into amyloid fibrils, and the absence of fibrillar aggregates in the granules during non-pathological condition raises the question if an endogenous inhibitor is present in the secretory granule. It was shown that IAPP aggregation was in a concentration dependent manner inhibited by insulin (32, 169). Therefore, a change in the intragranular milieu may be enough to facilitate aggregation of proIAPP/IAPP. When the composition of endocrine granules was determined it was shown that chaperones were present. This shows that assisted folding may be of importance also at this site (170). 20 It is possible that two different ways exist for IAPP to reduce the beta cell number in islets of Langerhans in patients with type 2 diabetes. One is through formation of oligomers that induce ER-stress ultimately leading to apoptosis. Amyloid formation has been suggested to primarily constitute a surviving pathway where formation of fibrils is a way to neutralize toxic oligomers. However, intracellular growth of amyloid which replaces the cytoplasm may also induce apoptosis. Mutations in the IAPP gene and amyloid Mutations in the IAPP gene occur both in the coding region and in the regulatory part of the gene. The most studied mutation is the S20G, present in the Asian population (171). In a search for mutations within the coding region of IAPP, 294 patients with type 2 diabetes were analysed and the S20G mutation was found in 4.1 %, but was absent in the control group and in patients with type 1 diabetes. In a more comprehensive study that included >1500 Japanese subjects with type 2 diabetes the mutation was found in 2.6 % and it was concluded that IAPPS20G is linked to an increased risk for the development of this disease (172). A study performed on a Chinese population identified the mutation in 2.6 % of the individuals with early-onset type 2 diabetes but in none of the control subjects. Screening for the mutation in other populations failed to identify the S20G variant (173).There is an increase in the fibrillation propensity of S20G IAPP in vitro (174, 175) and expression of the mutant in Cos-1 cells induced more apoptosis (175). The in vitro findings indicate that S20G may form more cell toxic amyloid in vivo. A gene promoter polymorphism in the region -132 G/A of IAPP has been identified in a Spanish population. The frequency of the G/A genotype was 9.7% in the studied 186 individuals with type 2 diabetes and 1.5% in the non-diabetic control group (176). The presence of the mutation has been shown to increase the basal transcriptional rate of the IAPP promoter (177). This is 21 interesting for the amyloidogenesis since over expression and increase of the amyloid precursors is believed trigger amyloid formation. However, the search for the promoter mutations in other countries have failed to show association to type 2 diabetes or islet amyloid load (178). Genome-wide associated (GWA) studies performed in Caucasian (179, 180) and in Han Chinese (181) populations have until know identified 20 different polymorphisms with shifting associations to type 2 diabetes (T2D), and hitherto, neither of the pinpointed loci include IAPP. Importance of amyloid in transplanted islets Impact of amyloid in transplanted human islets is a fairly new field. Islet transplantation as a possible strategy to restore or improve the glucose homeostasis in patients with type 1 diabetes was tried out already in the 1970s, but with low success (182). Despite major changes in e.g. islet isolation protocols, transplantation procedure and immunesuppression regime few recipients remained insulin independent 1 year after transplantation. Over the years many experimental transplant studies have been performed with rat and mouse islets which are protected against islet amyloid formation (see above). In a study from 1995, human islets were implanted under the kidney capsule of nude mice which were either normoglycaemic or made diabetic with alloxan (146). The implants were recovered after 2 weeks and, surprisingly, amyloid was detected in 16 out of 22 transplants (73%) after Congo red staining or by immune electron microscopy. There was no difference between diabetic and nondiabetic recipients. Further studies on transplanted human islets showed that amyloid formation was not restricted to kidney 22 implants and amyloid developed to the same degree in human islets implanted to the spleen or liver (183). Experimental studies with transgenic mouse islets, expressing human IAPP have verified the findings. A graft containing 100 islets isolated from transgenic mice were implanted under the kidney capsule on mice with streptozotocin induced diabetes. The graft was sufficient for adjusting the blood glucose level, but over the 6 following weeks an increase in plasma glucose concentration was detected but was not seen in mice transplanted with non-transgenic mouse islets. The implants were recovered after 6 weeks and amyloid was found in 92 % of the transplants with transgenic islets and the beta-cell volume was reduced by 30% (184). Studies in human material have of natural reasons been very limited. We have, hovever, studied the amyloid content in human islets implanted to the liver of a type 1 diabetic man, dying from a myocardial infarction (185). The recipient received three different grafts and was off insulin treatment for a period between transplantations. Amyloid was found in about 50 % of the islets identified in the liver. This finding clearly points to amyloid as important factor for loss of graft survival. Is it possible to extend the survival of transplanted islets? Marzban et.al. reduced the proIAPP expression by 75% through the introduction of short interference (si) RNA in human islets kept in culture (186). The reduction of proIAPP synthesis reduced the amyloid load by 63% in islets cultured for 10 days. The results indicate that the proIAPP synthesis most likely must be abolished if amyloid formation should be prevented. 23 32-33 split proinsulin, 19 AC187, 9 adrenomedullin, 6 alpha-cell, 4 amylin, 1, 3, 24 amyloid fibrils, 12, 16, 19 anorectic effects, 9 anorexia nervosa, 10 AP/NST, 9 apoptosis, 16, 17, 20 autocrine, 7 beta-cell, 2, 4, 5, 16, 17, 18, 22, 24 beta-sheet structures, 14 bone, 10 brain, 3, 6, 9, 10, 16 brain-4, 3 Brochmann body, 6 calcitonin, 3, 6, 24 cat, 8, 24 chaperones, 17, 19 chicken, 6, CHOP, 18 clearance of IAPP, 5 C-peptide, 4 crinophagy,. 17 dexamethasone, 15 diabetes mellitus,, 8 dog, 8 enteroendocrine cells, 6 ER-stress, 18, 20 fish, 3, 6 gastric emptying, 8 gastrin, 6 gastrointestinal tract, 6 glycogen phosphorylase, 8, glycogen synthase, 8 growth hormone, 15 HbA1c, 11, 14 HSPA5, 18 hyperglycemia, 15, hyperinsulinemic, 19 hypothalamus, 10 IAPP, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 14, 15, 16, 17, 18, 19, 20, 21, 22, 24 IAPP gene, 3, 5, 15, 20 IAPP in the secretory granule, 18 insulin, 3, 4, 5, 6, 7, 8, 11, 13, 14, 15, 17, 19, 21, 22 intermedin, 6 islet amyloid, 1, 2, 12, 13, 14, 15, 18, 21, 24 islet amyloid polypeptide, 1, 24 Macaca mulatta, 13 Macaca nigra, 13 misfolding diseases, 11 monkey, 9, 29 mouse, 6, 9, 14, 15, 18, 21, 22 N-IAPP, 19 Octodon degu, 14 oligomers, 2, 16, 18, 20, 24 osteoblasts, 10 osteoclasts, 10 paracrine, 7 PC1/3, 3, 4, 19 PC2, 4, 19 pdx-1, 3 peptide YY, 6 plasma levels of IAPP, 4 postprandial glucose, 8 posttranslational processing, 17 Pramlintide/symlin, 10 preproIAPP, 5 primates, 13 proIAPP, 4, 18, 19, 22 proinsulin, 19 proline substitutions, 10, 14 rat, 6, 7, 8, 9, 10, 14, 15, 17, 18, 21 regulation of food intake, 10 S20G, 20 satiety factor, 9 secretory granules, 4, 17, 18 short interference (si) RNA, 22 somatostatin, 5, 6 streptozotocin, 22 transgenic mouse, 15, 22 transplanted islets, 21, 22 type 1 diabetes, 8, 20, 21 type 2 diabetes, 2, 3, 11, 12, 13, 18, 20, 21, 24 UPR, 17 24 Conclusion Taken together the results from the animal studies show that amyloid develops before beta-cell deficiency and the occurrence of oligomers and amyloid intracellular induce beta cell death. Prevention of islet amyloid will save beta-cells and extend hormone secretion. Acknowledgements I thank Per Westermark for valuable suggestions. Supported by The Swedish Research Council, the European Framework 6 Program to EURAMY, the Swedish Diabetes Association and Family Ernfors Fund.