Evaluation of an Automatic Surveillance System of
advertisement
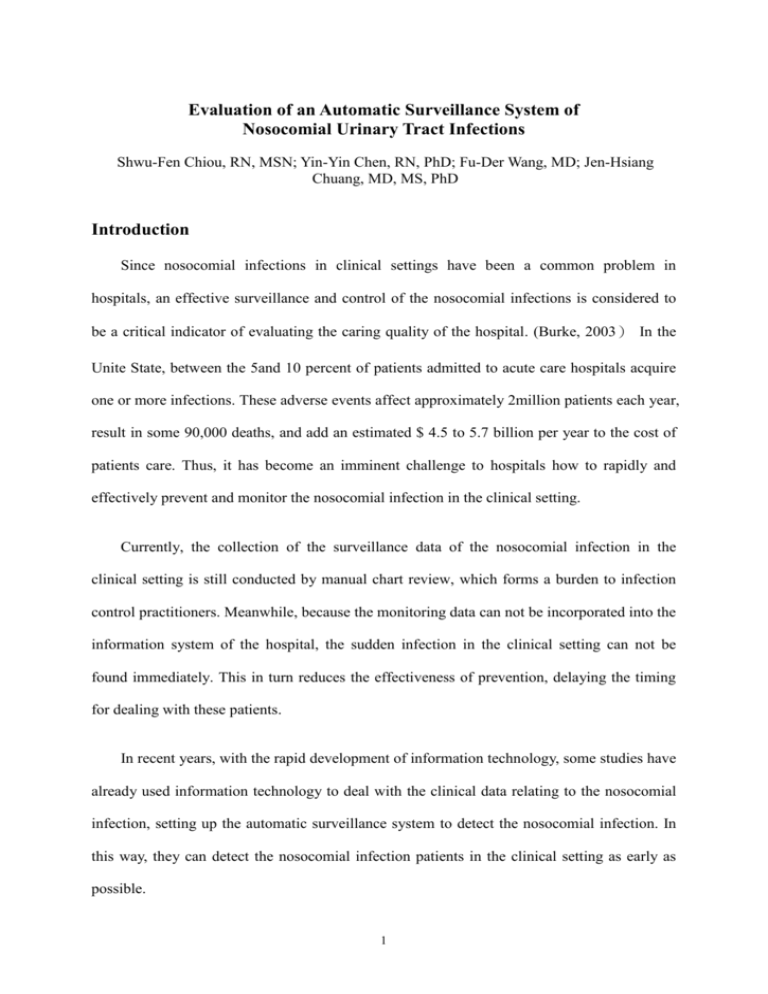
Evaluation of an Automatic Surveillance System of Nosocomial Urinary Tract Infections Shwu-Fen Chiou, RN, MSN; Yin-Yin Chen, RN, PhD; Fu-Der Wang, MD; Jen-Hsiang Chuang, MD, MS, PhD Introduction Since nosocomial infections in clinical settings have been a common problem in hospitals, an effective surveillance and control of the nosocomial infections is considered to be a critical indicator of evaluating the caring quality of the hospital. (Burke, 2003) In the Unite State, between the 5and 10 percent of patients admitted to acute care hospitals acquire one or more infections. These adverse events affect approximately 2million patients each year, result in some 90,000 deaths, and add an estimated $ 4.5 to 5.7 billion per year to the cost of patients care. Thus, it has become an imminent challenge to hospitals how to rapidly and effectively prevent and monitor the nosocomial infection in the clinical setting. Currently, the collection of the surveillance data of the nosocomial infection in the clinical setting is still conducted by manual chart review, which forms a burden to infection control practitioners. Meanwhile, because the monitoring data can not be incorporated into the information system of the hospital, the sudden infection in the clinical setting can not be found immediately. This in turn reduces the effectiveness of prevention, delaying the timing for dealing with these patients. In recent years, with the rapid development of information technology, some studies have already used information technology to deal with the clinical data relating to the nosocomial infection, setting up the automatic surveillance system to detect the nosocomial infection. In this way, they can detect the nosocomial infection patients in the clinical setting as early as possible. 1 Therefore, this study aims to integrate the electronic medical records relating to the nosocomial infection in order to establish an automatic surveillance system for the detection of patients with nosocomial urinary tract infections, and to evaluate the performance of the surveillance system. Methods A retrospective study was conducted in a 2,700-beds medical center in the Taipei area. The research data for nosocomial urinary tract infections from the hospital information system, which consisted of the demographic data of the patients, physicians’ prescriptions, the laboratory data(albumin, white blood cells, hemoglobin, platelets, urine routine, and urine microbiologic report), and medical records during hospitalization. From September, 2004 to December, 2004, 1,609 patients with positive urine culture were collected as training dataset. The training dataset was using to develop the rules for nosocomial urinary tract infections according to the definitions of the Centers for Disease Control and Prevention. In addition, another 624 patients with positive urine culture were collected as testing dataset serving to validate the accuracy of these rules from January 2005 to February 2005. In this study, Detection results from the automatic surveillance system were compared with the infection control practitioners (ICP) used by traditional chart review method for nosocomial urinary tract infections. And then, sensitivity, specificity, positive predictive value, and negative predictive value were calculated to evaluate the performance of the automatic surveillance system. Because ICP investigate the medical records was rather time-consuming, only part of the samples of the training dataset and testing dataset were randomly picked up. Finally, 480 samples were chosen out of the training dataset, while 240, out of testing dataset. 2 Results Concerning all of the related data of detecting the nosocomial urinary tract infections, the existing electronic medical record data were processed by Microsoft Access 2003 to establish database. And the rule-base method was used to develop the judging rules of nosocomial urinary tract infections. Meanwhile, SQL language was employed to write out the rules of the nosocomial urinary tract infections. Until now, five rules of judging the infection were carved out. And Asp.Net was used as a tool to design the Web with the interface of the surveillance system shown as follows. Of the 240 patients detected by the surveillance system, 66 ones belonged to the nosocomial urinary tract infections, while 174 ones did not belong to the nosocomial urinary tract infections. The sensitivity of the automatic surveillance system was 99 %, while specificity was 47 %. The positive predictive value (PPV) was 41 %, and the negative predictive value (NPV) was 99 %. Discussion According to the results of the research, the sensitivity of the automatic surveillance system reached 99%, which meant that this system as a whole could fully detect the patients with nosocomial urinary tract infections. However, the specificity was only 47%, which meant that this system could detect 47% of the cases without nosocomial urinary tract 3 infections. Although this value was seemingly low, this system could save 47% of time the infection control practitioners averagely spent surveying the patients’ medical records and making judgments on when the patients were infected. This could reduce the regular workload of the infection control practitioners. Compared to the study of et al. Bouam(2003), the specificity of this project was much lower that that of Bouam since the sensitivity and specificity of his automatic surveillance system were 91% and 91%, respectively. This was perhaps because his automatic surveillance information system included complete surveillance data of the nosocomial infections. However, the system developed by this study included only some basic data as well as related laboratory reports, lacking some important surveillance data such as body temperatures, patients’ clinical symptoms as the existing incomplete electronic medical records did affect the effectiveness of this system. Judging from these, it could be seen that the completeness of data played a critical part in determining the effectiveness of the automatic surveillance system. Conclusion This study has integrated the current electronic medical records to set up an automatic surveillance system of detecting the nosocomial urinary tract infections, validating the accuracy of its function. It was found that due to the accuracy of the nosocomial urinary tract infections, this system not only could reduce the workload of the infection control practitioners but reach the goal of immediate and effective detection. This could also push the medical and nursing staff to put this system into practice in order to boost the medical and caring quality. 4 Limitation Because of the limitation of time and human resources, this study could only survey the medical records of part of the recruited patients to evaluate the effectiveness of this automatic surveillance system. This may affect the results of this study. In the near future more and more patients can be recruited into this automatic surveillance system for detection, which will persistently correct the program and enhance the accuracy of this system. Acknowledgements We appreciated the grant offered by “Veterans General Hospital University System of Taiwan Joint Research Program” as well as the sincere help offered by the information management department of the hospital. Thanks a lot for they provided information and support. In addition, we ought to pay our tribute to all the infection control practitioners working for the infection control department for their suggestions about nosocomial urinary tract infections. Reference 1. Bates, D. W., & Gawande, A. A. (2003). Improving safety with information technology. N.Engl.J.Med., %19;348(25), 2526-2534. 2. Bates, D. W., Evans, R. S., Murff, H., Stetson, P. D., Pizziferri, L., & Hripcsak, G. (2003). Detecting adverse events using information technology. J.Am.Med.Inform.Assoc., 10(2), 115-128. 3. Bouam, S., Girou, E., Brun-Buisson, C., Karadimas, H., & Lepage, E. (2003). An intranet-based automated system for the surveillance of nosocomial infections: prospective validation compared with physicians' self-reports. Infect.Control Hosp.Epidemiol., 24(1), 51-55. 4. Burke, J. P. (2003). Infection control - a problem for patient safety. N.Engl.J.Med., 348(7), 651-656. 5. Evans, R. S., Larsen, R. A., Burke, J. P., Gardner, R. M., Meier, F. A., Jacobson, J. A., et al. (1986). Computer surveillance of hospital-acquired infections and antibiotic use. The Journal of the American Medical Association, 256(8), 1007-1011. 6. Fiszman, M., Chapman, W. W., Aronsky, D., Evans, R. S., & Haug, P. J. (2000). Automatic detection of acute bacterial pneumonia from chest X-ray reports. 5 J.Am.Med.Inform.Assoc., 7(6), 593-604. 7. Haas, J. P., Mendonca, E. A., Ross, B., Friedman, C., & Larson, E. (2005). Use of computerized surveillance to detect nosocomial pneumonia in neonatal intensive care unit patients. American Journal of Infection Control.33(8):439-43, 33(8), 439-443. 8. Jarvis, W. R. (1996). Selected aspects of the socioeconomic impact of nosocomial infections: morbidity, mortality, cost, and prevention. Infect Control Hosp Epidemiol, 17(8), 552-557. 9. Jarvis, W. R. (2001). Infection control and changing health-care delivery systems. Emerg Infect Dis, 7(2), 170-173. 10. Lamma, E., Mello, P., Nanetti, A., Riguzzi, F., Storari, S., & Valastro, G. (2006). Artificial intelligence techniques for monitoring dangerous infections. IEEE Trans.Inf.Technol.Biomed., 10(1), 143-155. 11. Pittet, D., Safran, E., Harbarth, S., Borst, F., Copin, P., Rohner, P., et al. (1996). Automatic alerts for methicillin-resistant Staphylococcus aureus surveillance and control: role of a hospital information system. Infect Control Hosp Epidemiol, 17(8), 496-502. 12. Pokorny, L., Rovira, A., Martin-Baranera, M., Gimeno, C., onso-Tarres, C., & Vilarasau, J. (2006). Automatic detection of patients with nosocomial infection by a computer-based surveillance system: a validation study in a general hospital. Infect.Control Hosp.Epidemiol., 27(5), 500-503. 13. Weinstein, R. A. (1998). Nosocomial infection update. Emerg Infect Dis, 4(3), 416-420. 14. Wilson, J. W., Oyen, L. J., Ou, N. N., McMahon, M. M., Thompson, R. L., Manahan, J. M., et al. (2005). Hospital rules-based system: the next generation of medical informatics for patient safety. Am.J.Health Syst.Pharm., 62(5), 499-505. 15. Wisniewski, M. F., Kieszkowski, P., Zagorski, B. M., Trick, W. E., Sommers, M., & Weinstein, R. A. (2003). Development of a clinical data warehouse for hospital infection control. J.Am.Med.Inform.Assoc., 10(5), 454-462. 16. Wright, M. O., Perencevich, E. N., Novak, C., Hebden, J. N., Standiford, H. C., & Harris, A. D. (2004). Preliminary assessment of an automated surveillance system for infection control. Infect.Control Hosp.Epidemiol., 25(4), 325-332. 6