Ophthalmoscope
advertisement

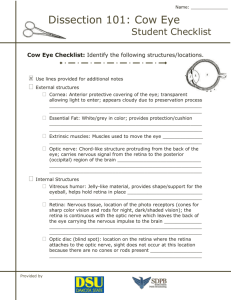
Anterior Chamber The cavity in the front part of the eye between the lens and cornea is called the Anterior Chamber. It is filled with Aqueous, a water-like fluid. This fluid is produced by the ciliary body and drains back into the blood circulation through channels in the chamber angle. It is turned over every 100 minutes. Chamber Angle Located at the junction of the cornea, iris, and sclera, the anterior chamber angle extends 360 degrees at the perimeter of the iris. Channels here allow aqueous fluid to drain back into the blood circulation from the eye. May be obstructed in glaucoma. Ciliary Body A structure located behind the iris (rarely visible) which produces aqueous fluid that fills the front part of the eye and thus maintains the eye pressure. It also allows focusing of the lens. Conjunctiva A thin lining over the sclera, or white part of the eye. This also lines the inside of the eyelids. Cell in the conjunctiva produce mucous, which helps to lubricate the eye. Cornea The transparent, outer "window" and primary focusing element of the eye. The outer layer of the cornea is known as epithelium. Its main job is to protect the eye. The epithelium is made up of transparent cells that have the ability to regenerate quickly. The inner layer of the cornea is also made up of transparent tissue, which allows light to pass. Hyaloids Canal A narrow channel that runs from the optic disc to the back surface of the lens. It serves an embryologic function prior to birth but none afterwards. Iris Inside the anterior chamber is the iris. This is the part of the eye which is responsible for one's eye color. It acts like the diaphragm of a camera, dilating and constricting the pupil to allow more or less light into the eye. Pupil The dark opening in the center of the colored iris that controls how much light enters the eye. The colored iris functions like the iris of a camera, opening and closing, to control the amount of light entering through the pupil. Lens The part of the eye immediately behind the iris that performs delicate focusing of light rays upon the retina. In persons under 40, the lens is soft and pliable, allowing for fine focusing from a wide variety of distances. For individuals over 40, the lens begins to become less pliable, making focusing upon objects near to the eye more difficult. This is known as presbyopia. Macula The part of the retina which is most sensitive, and is responsible for the central (or reading) vision. It is located near the optic nerve directly at the back of the eye (on the inside). This area is also responsible for color vision. Optic Disc The position in the back of the eye where the nerve (along with an artery and vein) enters the eye corresponds to the "blind spot" since there are no rods or cones in these location. Normally, a person does not notice this blind spot since rapid movements of the eye and processing in the brain compensate for this absent information. This is the area that the ophthalmologist studies when evaluating a patient for glaucoma, a condition where the optic nerve becomes damaged often due to high pressure within the eye. As it looks like a cup when viewed with an ophthalmoscope, it is sometimes referred to as the Optic Cup. Optic Nerve The optic nerve is the structure which takes the information from the retina as electrical signals and delivers it to the brain where this information is interpreted as a visual image. The optic nerve consists of a bundle of about one million nerve fibers. Retina The membrane lining the back of the eye that contains photoreceptor cells. These photoreceptor nerve cells react to the presence and intensity of light by sending an impulse to the brain via the optic nerve. In the brain, the multitude of nerve impulses received from the photoreceptor cells in the retina are assimilated into an image. Sclera The white, tough wall of the eye. Few diseases affect this layer. It is covered by the episclera (a fibrous layer between the conjunctiva and sclera ) and conjunctiva, and eye muscles are connected to this. Vitreous Next in our voyage through the eye is the vitreous. This is a jelly-like substance that fills the body of the eye. It is normally clear. In early life, it is firmly attached to the retina behind it. With age, the vitreous becomes more water-like and may detach from the retina. Often, little clumps or strands of the jelly form and cast shadows which are perceived as "floaters". While frequently benign, sometimes floaters can be a sign of a more serious condition such as a retinal tear or detachment and should be investigated with a thorough ophthalmologic examination. HOW IT WORKS The human eye belongs to a general group of eyes found in nature called “camera-type eyes.” Instead of film, the human eye focuses light onto a light sensitive membrane called the retina. Here’s how the human eye is put together and how it works: The cornea is a transparent structure found in the very front of the eye that helps to focus incoming light. Behind the cornea is a colored ring-shaped membrane called the iris. The iris has an adjustable circular opening called the pupil, which can expand or contract depending on the amount of light entering the eye. A clear fluid called the aqueous humor fills the space between the cornea and the iris. Situated behind the pupil is a colorless, transparent structure called the crystalline lens. Ciliary muscles surround the lens. The muscles hold the lens in place but they also play an important role in vision. When the muscles relax, they pull on and flatten the lens, allowing the eye to see objects that are far away. To see closer objects clearly, the ciliary muscle must contract in order to thicken the lens. The interior chamber of the eyeball is filled with a jelly-like tissue called the vitreous humor. After passing through the lens, light must travel through this humor before striking the sensitive layer of cells called the retina. The retina is the innermost of three tissue layers that make up the eye. The outermost layer, called the sclera, is what gives most of the eyeball its white color. The cornea is also a part of outer layer. The middle layer between the retina and sclera is called the choroids. The choroids contain blood vessels that supply the retina with nutrients and oxygen and remove its waste products. Embedded in the retina are millions of light sensitive cells, which come in two main varieties: rods and cones. Rods are good for monochrome vision in poor light, while cones are used for color and for the detection of fine detail. Cones are packed into a part of the retina directly behind the retina called the fovea. When light strikes either the rods or the cones of the retina, it's converted into an electric signal that is relayed to the brain via the optic nerve. The brain then translates the electrical signals into the images we see. Ophthalmoscope: A lighted instrument, one of the most important tools of the physician, used to examine the interior of the eye, including the lens, retina and optic nerve. The common clinical ophthalmoscope consists of a concave mirror and a batterypowered light (contained within the handle). The operator looks through a single monocular eyepiece into the patient's eye. The ophthalmoscope is equipped with a rotating disc of lenses to permit the eye be examined at different depths and magnifications. This may be enhanced by drugs that dilate the pupil and enlarge the opening into the structures within the eye. The ophthalmoscope is invaluable in many fields of medicine, including cardiology (cardiovascular disease), diabetes, hematology, medical genetics, neurology, neurosurgery, rheumatology, family medicine, pediatrics, internal medicine, and geriatrics. The invention of the ophthalmoscope is often erroneously credited to the great German physician-scientist Hermann von Helmholtz (1821-1894). Helmholtz demonstrated the principle of the ophthalmoscope in 1850 using a crude device (cardboard, glue, and microscope glass plates). By means of his ophthalmoscope, Helmholtz could place the eye of the observer in the path of the rays of light entering and leaving the patient's eye, allowing the patient's retina to be seen. However, Helmholtz was neither the first person to look into the living retina nor the first to fashion a device for viewing the retina. In 1823 Johannes Purkinje observed the back of the eye and in 1847 Charles Babbage fashioned an ophthalmoscope similar to the one later developed by Helmholtz. The work of Purkinje and Babbage lay largely unknown. Helmholtz rediscovered the ophthalmoscope and immediately realized and communicated its importance. The Ophthalmoscope and the Treatment of Eye Injuries The Medical and Surgical History of the War of the Rebellion specifically states that the ophthalmoscope was not used by army physicians during the war. Thus, Adams was correct in making that point, but his fact gives a misleading idea of the development of the field of ophthalmology in the U.S. at the time. American physicians had a great interest in the field before and during the war and were beginning to specialize in it, as shown by the found of the American Journal of Ophthalmology in 1864. They were able to use the arrangement of lenses, without a light source, called an ophthalmoscope; they were aware of problems associated with its use as shown by an entry in the Confederate States Medical and Surgical Journal in 1864. The article points out that an extract of the Calabar bean could reverse the prolonged blurring of vision resulting from the instillation of atropine to dilate the pupil to aid in ophthalmoscopic examination. Much later such extracts were found to contain physostigmine, which counteracts the effect of atropine. However, treatment of eye trauma is more relevant to a discussion of the quality of Civil War ophthalmology. A condition called sympathetic ophthalmia causes inflammation in an uninjured eye when one eye is inflamed. This process often develops following injury to an eye. It can cause serious loss of vision, even blindness, in the uninjured eye. We know of an autoimmune mechanism for this process and can treat it but there was no effective treatment during the Civil War. Avoiding it was most important, and the only way to avoid it was to remove a damaged, inflamed eye before inflammation developed in the good eye. Removal of such a damaged eye to protect the other one was first suggested by a physician named Pritchard in England in 1851. The fact that excision was ineffective once inflammation had developed in the good eye was a subject covered at the first International Conference on Ophthalmology which occurred at Heidelberg in 1863 although medical histories states that the entity was not well established until 1866. Prophylactic excision became the standard treatment, and remained so for decades. Civil War era surgeons were acquainted with sympathetic ophthalmia. The condition is discussed at length in the Medical and Surgical History in the first surgical volume which was written after the war, in the 1870s and probably reflects post-war knowledge. The article describes 1,190 cases of wounds to one or both eyes treated during the war. Details of 254 cases of gunshot wounds of one eye are given and the statement is made that, "In forty-one of these cases vision in the uninjured eye became affected sympathetically, and in four instances was ultimately lost." The analysis concludes with the statement that, "A general survey of the accounts of gunshot injuries of the eye, reported during the war, instructs us that whenever foreign bodies are lodged in the glove, they should be extracted at all hazards. If it is impracticable to find them, the globe should be extirpated to preserve the other eye." This post-war statement of an important principle is correct, but there is no clear evidence that such prophylactic excision was done during the war. The discussion, however, documents that Civil War era American physicians were up-to-date in their knowledge of traumatic diseases of the