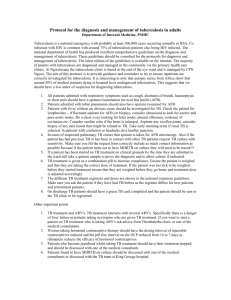
Tuberculosis
advertisement

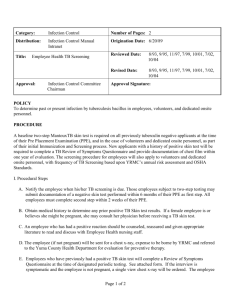
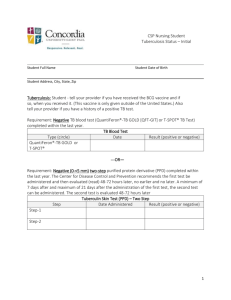
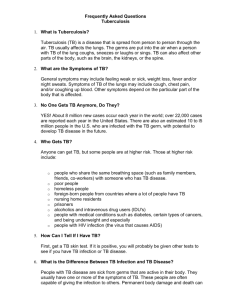
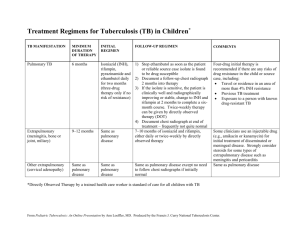
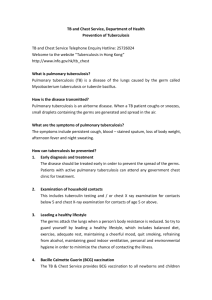
Tuberculosis Introduction Tuberculosis (TB) is an infection caused by a germ called the tubercle bacillus or Mycobacterium tuberculosis. It can affect the lungs (pulmonary TB) or other parts of the body, such as the lymph nodes (tuberculous adenitis or scrofula), the skin and the bones. Tubercle bacilli can remain dormant for years before producing active disease. In most cases lung infection is well controlled by the immune system, and shows no symptoms. Active lung disease occurs if the immune system becomes less effective. A person may have had an infection with tuberculosis without being aware. This can be discovered by a tuberculin skin test, the Heaf (or Mantoux) test. When positive, it indicates that the person has a degree of natural immunity. People who test negative do not have this immunity and are more susceptible to infection by TB. Tuberculin-negative people may benefit from BCG inoculation. This uses a vaccine made from a modified version of the TB germ. It reduces the risk of developing TB in about 70% of those vaccinated for approximately 15 years. Symptoms Symptoms of pulmonary TB include fever, fatigue, loss of appetite and weight, night sweats and persistent cough. Phlegm coughed up may be streaked with blood. Tuberculous pleurisy (affecting the membranes around the lungs) leads to an accumulation of fluid in the pleural cavity (the normally very small space between the membranes) and partial collapse of the lung. Causes Pulmonary tuberculosis (which affects your lungs) is caught from an infectious person by breathing in tubercle bacilli germs when they cough or sneeze. However, tuberculosis is not easy to catch, and you need to be in close contact with an infectious person for a prolonged period of time to be at risk. The TB germ has a thick capsule, and can survive dry and usually hostile conditions (although it is killed by UV light, for example, sunlight). Risks Tuberculosis is spread in a similar way to a common cold; by coughing and sneezing. However, it is much more difficult to catch tuberculosis than it is to catch a cold, because you need to spend a prolonged amount of time in close contact with an infectious person to be at risk. Tuberculosis is unlikely to be spread through spitting and cannot be spread by sharing objects. Therefore, it is unlikely that you will catch tuberculosis unless you are living in the same household as someone who is infectious. Even if this is the case, only about 10% of people who become infected with tuberculosis go on to develop the condition. In most cases, the tubercle bacillus germs are destroyed or contained by your immune system. In addition to this, not everyone who has tuberculosis is infectious. Those who are only remain infectious for about two weeks, if they are receiving the correct treatment. Contact tracing and screening for tuberculosis If you have tuberculosis, your nurse will ask you to list the people you usually spend most time with. These people will then be contacted and invited to be screened for tuberculosis, to see whether or not they have been infected by the condition. In most cases, your close contacts will not have been infected with tuberculosis and no treatment will be necessary. However, it is important that your close contacts are screened so that any cases of tuberculosis are identified and treated as early as possible. This helps to prevent the condition from spreading further. Screening for close contacts of those with tuberculosis may involve a blood test, a chest X-ray, and a skin test (Mantoux test). Treatment Tuberculosis is treated with antituberculous drugs in combination, for at least six months. However, you usually will start to feel better within two to four weeks of starting medication. Treatment normally consists of a combination of antibiotics. The standard treatment involves Isoniazid and Rifampicin being given for at least six months. In addition, Pyrazinamide and Ethambutol are also given for the first two months of treatment. Rifabutin, Cycloserine, Capreomycin and Streptomycin can also be used in the treatment of TB if drug resistance has been shown to be present. It is vital to complete the course of drugs as directed. If this is not done, the bacteria will not be completely gone and drug-resistant strains may develop. Prevention The old BCG vaccination programme, which was delivered through schools, was replaced with an improved programme of targeted vaccination for people at highest risk in September 2005. Parents and health professionals will be able to find information about the changes on the immunisation website or by calling NHS Direct on 0845 4647. This factsheet has been produced using information provided by the NHS Direct website. For more detailed information please visit www.nhs.uk/conditions/tuberculosis