Nutritional Supplement Program
advertisement

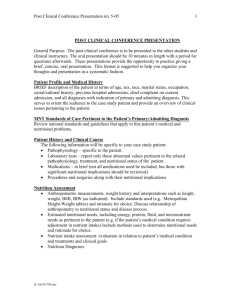
PRESCRIBER STATEMENT OF MEDICAL NECESSITY NUTRITIONAL SUPPLEMENT PRE-AUTH FORM For Tube-Fed Patients and Patients with an Inborn Error of Metabolism Maryland Medicaid - Division of Pharmacy Services Tel # 410-767-1755 or 1-800-492-5231 Option 3 Fax to: 410-333-5398 (Incomplete forms will be returned) PHYSICIANS: Please complete and sign: 1. Patient’s Name________________________________________________Phone # __________________ Patient’s Address_______________________________________________________________________ Patient’s Medicaid ID # ______________________________________Date of Birth:________________ Patient location: ___ Residence; ___ Nursing Home; ___ Hospital Body Weight:________Circle kg or lb; Height: ____________ Date measured:____/________/________ 2. Justification for nutritional supplement need: a/ Diagnosis and dates of onset_____________________________________________________________ b/ If recipient has an inborn error of metabolism, list specific condition:_____________________________ c/ Is patient currently tube-fed? Yes___No___If partially tube-fed, only amount of enteral nutrition actually being tube-fed will be approved. Please circle approximate percentage of partial tube-feeding: 100%; 75%; 50%; 25%; <25% Anticipated duration of tube feeding ______(# days) _____(# months) _____indefinitely Place and date when G-tube was inserted:__________________________________________________ For REM recipients not tube-fed and without a metabolic disorder, the following documentation must be submitted to the Program for a determination of medical necessity: a/ a comprehensive metabolic panel, prealbumin/albumin levels, serum magnesium&phosphorus values. b/ a BMI/Age chart in lieu of the standard growth chart. All values shown on the chart must be legible. c/ a recent medical history and physical examination documenting weight loss over the prior 6 months justifying need for the product along with the weight measurements and dates when measured. 3. Rx: Nutritional Supplement Order- A new medical necessity form must be submitted for each nutritional product and for each change in product, dosage/dosage frequency Product&Dosage Form:__________________________________Package Size:________#cans/Case:_____ Dose&dosage frequency: _____________________________________________________Must specify: ________ gram/day of unreconstituted powder (specify quantity before dilution) – Use “gram” and not “can” to indicate package size since 1 can could be of any size.Note: 1lb can= from 423 to 480g. _________packet/day of unreconstituted powder _________ml/day of premixed ready-to-use liquid formula) or liquid concentrate before dilution _________ready-to-use-can(s)/day (must specify can size= _________ml/can) (i.e. 120ml or 240ml can) _________cans/day (must specify: # ________ml /can or # _________gram/can _________ calories prescribed per day- Convert daily calories to ml or gm or packet/day based on the specific product used X 30 days = ________________.This must approximate the total units billed on-line per 30 day supply. 4. Prescriber’s Signature:_______________________________Medicaid ID# ______________________ Prescriber’s Name:______________________________________________Date:_________________ Address: ____________________________________________________________________________ Phone# (____) ____________ Fax: (_____) ______________ ________________________________________________________________________________________ Nutritional supplement to be filled at the following pharmacy Pharmacy’s Name________________________________________Phone# (_______)________-________ Pharmacy’s Address______________________________________Fax#: (________)_________-________ Product NDC ________________________ Quantity per month:___________________ _________________________________________________________________________________________ FOR INTERNAL USE - APPROVED:____ from:__________to_________REJECTED: ____DATE: ________Initials: _____ DHMH 3495 (Rev. 06/2004) - Form may be duplicated. Division of Pharmacy Services- Maryland Medicaid Nutritional Supplement Program BILLING INSTRUCTIONS FOR PHARMACY PROVIDER Upon notification of approval of payment for the nutritional supplement by the Program, pharmacy providers are to submit claims on-line as follows: . Bill the actual NDC of the nutritional product dispensed. Bill the exact units as quantity dispensed. Units must be exact, expressed in”cc” for liquids, readyto-use or premixed formulas or liquid concentrates requiring further dilution; “each” for powders before reconstitution (i.e. each gram or each packet). Do not think of quantity as number of cans. Program reimbursement is calculated based on these exact units submitted. For example, a 1 lb canister may contain 420g or 450g of powder, or 8 oz (=240ml) of ready-to-use liquid depending on the specific product. Do not round-up or estimate quantities, i.e. 1 lb = 480 grams, or 1 pint = 480 ml. If 3 cans of 420g were dispensed, quantity billed should be = 1,260 (3 x 420) and not 1,440 (3 x 480). Quantity billed per Rx must be exact multiples of the unit package size expressed in “grams” or “cc = ml”. Maximum allowed on each claim is 34 days supply per Rx. Max # of refills per Rx is 11. Although the nutritional supplement is considered an over-the-counter item, the Program still requires a valid prescription for the product to be dispensed. Such prescription must be kept on file at the pharmacy for 6 years. Claim will initially deny with any of the following NCPDP error codes, “70 = NDC Not Covered”, “75= PA required”, “76 – Max Quantity Exceeded”, or “78= Cost Exceeds Max”, or “88-Overuse, Early Refill, Therapeutic duplication”, etc. Providers are to call 410-767-1755 or 1-800-492-6008 for an override if the claim should deny. Service overrides may be issued for an extended period which will allow claims to go through without need for prior-authorization during the allowed time frame. For continuation of nutritional therapy, a new Nutritional Supplement Prior-Auth Form must be completed at the following time intervals: every 6 months for tube fed recipients and for REM recipients who are not tube-fed or have no metabolic disorder, and every 2 years for metabolic recipients. Any change in dosage/dosage frequency requires completion of a new form. Providers will be notified of the status of their nutritional supplement requests within 24 hours of date of request. It is expected that prescribers reassess the nutritional status of their patients based on this time schedule. Requests for priorauthorization for payment of oral nutritional supplements for the REM population who is not tube-fed, or does not have a metabolic disorder is evaluated on a case-per-case basis, with careful consideration to the nutritional and the clinical status of the individual recipient, and not based strictly on the diagnosis. For REM Recipient on existing oral nutritional supplement, a one-time 30 day emergency supply of the nutritional supplement will be prior-authorized until the documentation is received by the State for a determination of medical necessity for the continuation of nutritional therapy. Worksheet for calculation of total quantity dispensed per month based on prescriber’s order: Unreconstituted Powder __________gram X ______times per day =:__________gm/day x 30 days = ______________ grams Liquid ready-to-use premix or Liquid Concentrate requiring further dilution _________ml X _____times per day =___________ml/day x 30 days= __________________ml Powder packets (before reconstitution) _______packets X _____times/day = _______packets per day x 30 days= ______________packets Mailing or faxing of Medical Necessity Form. Submit or fax completed Nutritional PA Request Form (3495) to: Office of Operations, Eligibility & Pharmacy Services (OOEP) - 201 W. Preston St., 4th floor -Baltimore, MD 21201. Fax #: 410-333- 5398. For all inquiries, call: Tel: 410-767-1755 or 1-800-492-5231 Option 3. DHMH 3495 (01/2007)