Supplying Lithium Therapy - National Patient Safety Agency
advertisement

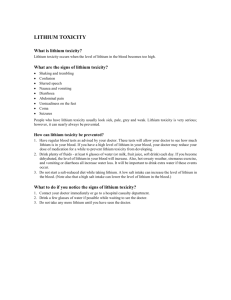
STANDARD OPERATING PROCEDURE Supplying Lithium Therapy Date of Preparation: Date of next review: Prepared by: Signature: Date review takes Version number: place and initials STANDARD OPERATING PROCEDURE SUPPLYING LITHIUM THERAPY This standard operating procedure (SOP) should be read in conjunction with the accompanying guidance notes and should be tailored to meet your individual circumstances. SCOPE This procedure covers the supply of lithium therapy by the pharmacy and includes prescription receipt, pharmaceutical assessment, interventions and problem solving, assembly and labelling, accuracy checking and transfer to patient. PROCEDURE The order and the way in which you carry out these steps in your pharmacy may vary from the list below. While professional judgement should prevail, as a principle THERAPY SHOULD NOT BE WITHHELD. The SOP identifies specific circumstances where the decision to withhold therapy should be considered. P1 Pharmacy staff authorised to take in prescriptions. Following procedures outlined in P2 of the SOP, the following pharmacy staff are authorised to take in prescriptions for lithium. Name P2 Prescription receipt [Pharmacy staff authorised to take in prescriptions for lithium] Follow your existing SOP for taking in a prescription. In addition: Ask for the lithium therapy record book and permission for the pharmacist to review it. Alert a member of the pharmacy team if the patient; does not have their lithium therapy record book declines permission to review (proceed to P4 below) has never received a lithium therapy record book. Check if the patient is taking any OTC medicines, in particular non-steroidal anti-inflammatory drugs (NSAIDs) and sodium-containing antacids. Inform the pharmacist if the patient is taking any OTC medicines. P3 Pharmaceutical assessment, interventions and problem solving [Pharmacist] Follow your existing SOP for legal and clinical assessment. In addition: Where the lithium therapy book is unavailable or the information is missing it is acceptable to: verbally confirm the target blood level range and current blood level with the clinic/GP or patient/carer as appropriate; however a record that this has occurred should then be made in the PMR and lithium therapy record book. Where no details are available proceed to P4 below. Ensure the following information is available and recorded in the PMR: o current brand, formulation and dose of lithium o lithium target blood level range o current lithium blood level o estimated glomerular filtration rate (eGFR) o thyroid function tests (TFTs, TSH ± FreeT4) o weight or BMI. Review this information each time a prescription is dispensed. Retain a record of as many results as possible to enable changes to be tracked. Verify that the prescription, record book and PMR are consistent. Reconcile any discrepancies. Check whether the current lithium blood level is within the patient’s blood level range and whether the lithium blood level has been checked within the last three months. If the current blood level is above 2mmol/L or above 1.5mmol/L and the patient has symptoms of toxicity refer the patient to Accident and Emergency. It is advisable that you do not dispense lithium in these circumstances. If the current blood level is above the target range and the patient has symptoms of toxicity it is advisable that you refer the patient immediately to the clinician/consultant/GP or, if the patient is unlikely to be seen promptly, to Accident and Emergency. It is advisable that you consider not dispensing lithium in these circumstances. If the current blood level is below the target range or above the target range but the patient has no symptoms of toxicity, inform the clinician/GP at the earliest opportunity. If the lithium blood level has not been checked within the last three months, inform the clinician/consultant/GP as appropriate. Check whether the TFTs (Thyroid stimulating hormone (TSH), FreeT4) are clinically significant for comment (refer to clinical information table). Also determine whether the TFTs have been checked within the last six months. Pharmacist to inform clinician/consultant/GP or refer if TSH values imply treatment with levothyroxine or TFTs are not regularly monitored. Check whether any changes to the eGFR imply dosing issues and whether the eGFR has been checked within the last six months. Pharmacist to inform clinician/consultant/GP if eGFR results imply dosing adjustments should be considered, or renal function is not being regularly monitored. Check whether there have been any gross changes to weight or BMI, the values increase rapidly or changes represent an issue for patients and whether the weight or BMI has been checked within the last 12 months. Pharmacist to inform clinician/consultant/GP if weight or BMI changes represent an issue or are not being regularly monitored. Check the patient’s PMR to see if there have been any changes to the patient’s other medication or if you have been informed that they are taking medicines OTC. Check for drugs which may alter lithium levels, in particular ACE inhibitors, NSAIDs, thiazide diuretics or sodium containing antacids. Refer to the latest BNF or the latest edition of Stockley’s Drug Interactions where available and the ‘Drug interactions’ section in the guidance notes for more detail. If a patient is prescribed these drugs, pharmacist to assess and consult the clinician/consultant/GP as appropriate. P4 Pharmaceutical assessment when lithium therapy record details unavailable [Pharmacist] If you are unable to verify any details of a patient’s lithium therapy; Check for signs of lithium toxicity and refer where appropriate. If the patient does not have symptoms of toxicity, explain the importance of the pharmacist reviewing the lithium therapy record book on each occasion and ask them to bring it next time. If the patient does not bring their lithium therapy record book with them repeatedly, pharmacist to inform the clinician/consultant/GP or PCT as appropriate that they are unable to comply with Patient Safety Alert – Safer lithium therapy (NPSA 2009/PSA 005) or if the patient refuses consent to review their therapy, ask permission to inform the clinician/consultant/GP that you are unable to review their lithium therapy. If the patient refuses consent to inform the clinician/consultant/GP, record this on the PMR and consider the appropriateness of disclosure without patient consent. P5 Assembly and labelling [Pharmacy staff authorised to assemble and label prescriptions] Follow your existing SOP for assembly, labelling and dispensing. In addition: Confirm the brand of lithium which the patient takes by checking the PMR or lithium therapy record book. Assemble the prescription using the correct brand of lithium. Where possible, avoid instructions such as ‘as directed’ on the label. It would be acceptable to label as ‘take as directed in your lithium record book’ Ensure a Patient Information Leaflet is included. Attach the ‘Li’ prescription alert sticker to the bagged up package. Lithium may be included in monitored dosage systems following risk assessment. P6 Accuracy checking [Pharmacy staff authorised to accuracy check or pharmacist] Follow your existing SOP for checking and bagging a prescription. In addition: Double check that the correct brand has been selected. Double check that the correct strength(s) have been selected. Double check that the dosage on the label(s) is correct. Double check that the labels for different strengths have not been transposed. P7 Pharmacy staff authorised to transfer lithium prescriptions to a patient Following procedures outlined in P8 of the SOP the following staff are authorised to transfer prescriptions for lithium to a patient. Name P8 Transfer to patient [Pharmacy staff authorised to transfer prescriptions for lithium to a patient] Follow your existing SOP for giving out a prescription. In addition: Check the expected dose, formulation and brand of lithium with the patient or representative and ascertain that this is what was expected. Check that the patient and/or carer understand how to take the correct dose in relation to the number of mg and the number of tablets and explain the importance of remembering to take every dose as prescribed. If the dosage instructions are ‘as directed’, check that the patient knows what their dose should be and check that this information is in their lithium therapy record book. Make a note in the PMR that a dosage was not on the prescription but was verbally reinforced. Check for and respond appropriately to any questions the patient might have. Ask the patient if they have noticed any side-effects from their treatment. Refer such patients to the pharmacist. Pharmacist to check if adverse effects could be side-effects and advise accordingly. When signs of lithium toxicity are suspected refer to the clinician/consultant/GP/out of hours/Accident and Emergency as appropriate. Side effects of lithium Upset stomach – particularly at the start of treatment Signs of lithium toxicity Severe hand shake (‘tremor’) Stomach ache along with nausea and diarrhoea Find shake (‘tremor’) of hands Muscle weakness Metallic taste in mouth Being unsteady on feet Weight gain Muscle twitches Swelling of ankles Slurring of words Feeling of thirst and passing a lot of urine Blurred vision Reduction in thyroid activity Confusion Alteration of renal function Feeling sleepy Remind the patient that they need to maintain a consistent intake of fluid and specifically not to become dehydrated. Ensure the patient is aware of the potential for lithium to interact with other medicines, including those bought over-the-counter, and that they understand the need to consult with a pharmacist or the prescriber before taking other medicines. Return the lithium therapy record book to the patient. APPENDIX 1 I have read and understood this standard operating procedure. Date Name Signature GUIDANCE NOTES SUPPLYING LITHIUM THERAPY In December 2009 the National Patient Safety Agency (NPSA) issued a Patient Safety Alert on safer lithium therapy: NPSA Patient Safety Alert – Safer lithium therapy (NPSA 2009/PSA005). The alert was in response to reports of harm caused to patients, including fatalities, involving lithium therapy. The alert was developed in collaboration with the Prescribing Observatory for Mental Health (POMH-UK) of the Royal College of Psychiatrists, the National Pharmacy Association (NPA), other organisations, clinicians and patients. It was designed to help NHS organisations, including community pharmacies, in England and Wales to take steps to minimise the risks associated with lithium therapy and to ensure that potential harm to patients is minimised. The deadline for action is 31 December 2010. The NPSA Patient Safety Alert includes actions which are relevant to community pharmacy. This resource aims to help you review your dispensing procedures and prepare a written standard operating procedure (SOP) to ensure that you are complying with the Patient Safety Alert when lithium is supplied in your pharmacy. While all NPSA Patient Safety Alert actions may apply to your practice, those in italics are particularly relevant for the majority of community pharmacies: prescribers and pharmacists check that blood tests are monitored regularly and that it is safe to issue a repeat prescription and/or dispense the prescribed lithium; systems are in place to identify and deal with medicines that might adversely interact with lithium therapy; at the start of lithium therapy and throughout their treatment patients receive appropriate ongoing verbal and written information and a record book to track lithium blood levels and relevant clinical tests; patients prescribed lithium are monitored in accordance with NICE guidance; there are reliable systems to ensure blood tests results are communicated between laboratories and prescribers; Administration of lithium in social care settings such as care homes and the use of monitored dosage systems are outside the scope of the Patient Safety Alert. However, it would be good practice to review lithium blood levels and health checks of patients in care homes. Lithium may be included in monitored dosage systems following risk assessment. A pharmacist is allowed to write in the patient’s lithium therapy record book. A pharmacist can make notes in the patient’s information booklet, lithium alert card and record book as appropriate. Signing and dating the entry will maintain an audit trail. When reviewing a patient’s lithium therapy it may be appropriate for the pharmacist to discuss observations with the patient. The pharmacist should use their professional judgement to determine if discussion with the clinician/consultant/GP is in the patients’ interest. If you are aware that tests are not being conducted in accordance with the Patient Safety Alert this SOP directs that you contact the prescriber making them aware of the issues. You must document this communication. Use Lithium: is the gold standard used alone or in combination for mania and prophylaxis in bipolar disorder is an option for Treatment Resistant Depression (TRD) has anti-suicidal effects. Different brands The BNF states that lithium preparations vary widely in bioavailability. The brand or formulation should not be changed without appropriate communication and monitoring. Drug interactions Many drugs have been found to interact with lithium, in particular thiazide diuretics, NSAIDs, ACE inhibitors and sodium containing antacids. In principle if a drug acts on or through the kidney, an interaction is possible. When assessing potentially interacting medication consider: if lithium levels are being monitored more frequently. if the use of the drugs is occasional. You may need to advise a patient of the potential harm of using an interacting drug occasionally. if lithium dosing has been altered to compensate for interacting drugs. sodium-containing antacids reduce lithium levels. To compensate, the patient’s dose may have been increased. If the patient then stops taking the antacid toxicity may occur. CLINICAL INFORMATION Test Clinical reason Frequency of test Lithium blood level Blood levels are an indication of clinical efficacy or potential toxicity. Levels should be within target range, not sub therapeutic or toxic. Toxicity has been seen at levels ≥1.2 mmol/L, but it is very dependent on renal function. In elderly renally compromised patients, levels <1 mmol/L have been toxic. Once blood levels are stable, ‘normally’ every 3 months. Monitoring should be increased with potential drug – drug interactions, such as the introduction of thiazide diuretics. Thyroid function tests (TFTs) Lithium is associated with long-term risk of hypothyroidism. A change in formulation should be treated as initiation of therapy for monitoring i.e weekly until stable. Every 6 months. Normal range Determined by prescriber and documented in the patient’s lithium therapy record book. Potential range between 0.4mmol/L – 1mmol/L. NICE suggests 0.6-0.8 mmol/L as the optimum range. However, some patients who are young with excellent renal function may require up to 1.2mmol/L. Higher levels are required for patients with acute exacerbations of mania. Laboratories vary in the method of testing and in the units of reporting, thus the ‘normal’ range may vary. Approximate normal reference ranges are: Thyroid-stimulating hormone (TSH) 0.5 – 5.5mU/L Free thyroxine (FT4) 926pmol/l FreeT4 is depressed with hypothyroidism. Patients with a sustained increase in TSH of greater than twice the upper limit of ‘normal’ (~10 mU/L) which is confirmed by repeat testing after 2 weeks should be treated with levothyroxine. What to check for What to do Levels below or above the patient’s target blood level range. Also, the trend in blood levels. Progressively increasing lithium levels are a consequence of deteriorating renal function. Be more vigilant with elderly patients, or patients experiencing side effects which could be signs of toxicity. Reassure the patient if tests are unremarkable. Inform clinician/GP or refer if appropriate. TSH values which are increasing and/or free T4 values that are decreasing. Reassure the patient if tests are unremarkable. Inform clinician/GP or refer if appropriate. Document your actions in the PMR or dedicated record. Patients with levels above 2mmol/L should be referred to Accident and Emergency. Document your actions in the PMR or dedicated record. Test Estimated glomerular filtration rate (eGFR) Weight/BMI Clinical reason Measures the level of kidney function. Lithium associated with long-term risk of chronic renal impairment. Commonly patients do gain weight; however, loss of weight is linked to worsening depression. Weight gain may be linked to hypothyroidism and viewed as a complication of lithium therapy. Frequency of test Every 6 months Every 12 months as part of a general health check. Every 6 months when prescribing medication for children, adolescents or during an acute manic episode. Normal range A patient with a TSH which is around double the normal upper limit (~10 mU/L) or between the upper normal limit and double the normal upper limit (~5.5mU/L - ~10mU/L) may require additional monitoring and possible treatment with levothyroxine. Assays vary between laboratories. Values below 60 ml/min/1.73 m2 are noteworthy, >90 ml/min/1.73 m2 is considered normal. Renal function deteriorates with age. Varies between patients What to check for An eGFR which is decreasing and/or results imply dosing adjustments should be considered. Trends in change in weight, or sudden changes in weight, in particular rapid weight gain. What to do Reassure the patient if tests are unremarkable. Inform clinician/GP or refer if you have concerns that renal function is deteriorating and no dose adjustments appear to have been made. Document your actions in the PMR or dedicated record. Monitoring and achieving goals for weight should be encouraged. May be viewed as an indicator of health status. Rapid weight gain should be referred. The absence of a weight check is not a reason for withholding therapy. Document your actions in the PMR or dedicated record. RESOURCES AND FURTHER INFORMATION NPSA The Patient Safety Alert, supporting documentation and PDFs of a Lithium Therapy Record book, Lithium Therapy – Important information for patients booklet and Lithium Alert Card can be accessed and downloaded from the NPSA website at http://www.npsa.nhs.uk. You are advised to read this material and store a copy for reference in your pharmacy. Supplies of the patient information booklet, lithium alert card and record book are available from the current NHS Non-Secure Contract held by 3M. Orders should be sent to: Telephone 0845 610 1112 Email: nhsforms@spsl.uk.com The contact for the Alert is: Dr David Gerrett Senior Pharmacist National Patient Safety Agency 4-8 Maple St London W1T 5HD david.gerrett@NPSA.NHS.UK NPA resources The following items can be obtained from NPA Sales on 01727 800401: Prescription alert stickers Medicine care cards – can be used to provide further information and/or reminders to help patients remember to take their medicines correctly. NHS resources Lithium therapy record books and the booklet Lithium therapy important information for patients are available to purchase from NHS forms (0845 6101112). Please note that some clinics may have produced their own lithium therapy record book based on the NPSA version. The clinician/consultant initiating therapy or GP for patients being maintained in the community are primarily responsible for providing the lithium therapy record book, the Lithium therapy important information for patients booklet and the lithium alert card. However, repeats of the record book may be made available from clinicians/consultants, GP or community pharmacists. CPPE Training materials on bipolar disorder are available on the CPPE website www.cppe.ac.uk/ NICE guidance NICE guidance on the management of bipolar disorder can be found at: http://guidance.nice.org.uk/CG38/Guidance/pdf/English Further References Ward ME, et al. Clinical pharmacokinetics of lithium. J Clin Pharmacol 1994;34:280–5. Reiss RA, et al. Lithium pharmacokinetics in the obese. Clin Pharmacol Ther 1994;55:392–8. Thomsen K, Schou M. Avoidance of lithium intoxication: advice based on knowledge about the renal lithium clearance under various circumstances. Pharmacopsychiatry 1999;32:83–6. Sproule BA, et al. Differential pharmacokinetics of lithium in elderly patients. Drugs Aging 2000;16:165–77. Kripalani M, Shawcross J, Reilly J, Main J. Lithium and chronic kidney disease. BMJ 2009;339:b2452 Livingstone C, Rampes J. Lithium: a review of its metabolic adverse effects. Psychopharmacol 2006;20(3):347-55.